Introduction
Computed Tomography (CT) plays an important diagnostic role in patients with sinonasal diseases and determines the treatment. The CT images clearly show fine structural architecture of bony anatomy thereby determining various anatomical variation, extent of disease and characterization of various inflammatory, benign and malignant sinonasal diseases.
Aim
To evaluate sensitivity and specificity of CT in diagnosis of sinonasal diseases and to characterise the benign and malignant lesions with the help of various CT parameters. Also, to correlate findings of CT with histo-pathological and diagnostic nasal endoscopy/ Functional Endoscopic Sinus Surgery (FESS) findings.
Materials and Methods
In this hospital based prospective study 175 patients with symptomatic sinonasal diseases were evaluated by clinical diagnosis and 16 slice Multi Detector Computed Tomography (MDCT). The details of findings of nasal endoscopy, Functional Endoscopic Sinus Surgery (FESS), histopathological examination and fungal culture were collected in all those cases where those investigations were done. All those findings were correlated with CT findings and statistical analysis was done by using Test statistics (sensitivity, specificity, Positive Predictive Value (PPV), Negative Predictive Value (NPV) and accuracy), Chi-Square test and Z-test for single proportions. Software used in the analysis was SPSS 17.0 version and graph pad prism 6.0 version and p < 0.05 was considered as statistically significant.
Results
CT diagnosis had higher sensitivity, specificity, PPV and NPV in diagnosing various sinonasal diseases in comparison to clinical diagnosis. On correlating CT diagnosis with final diagnosis, congenital conditions have 100% sensitivity and specificity. Chronic sinusitis has 98.3% sensitivity and 97.8% specificity. For fungal sinusitis the sensitivity was 60% and specificity was 99.3%. Polyps have sensitivity of 94.4% and specificity of 98.1%. Benign neoplasms have sensitivity of 90.9% and specificity of 99.2%, malignant neoplasms have sensitivity of 94.1% and specificity of 99.3%. The p-value in all instances was <0.05, i.e. <0.0001 indicating the significance of the findings.
Conclusion
CT is the modality of choice in imaging the sinonasal region for evaluating various congenital, inflammatory, benign and malignant pathologies and associated complications thereby planning the further management of the patient. CT is the best modality of choice for evaluating the bone erosion or destruction. The potential pitfalls to differentiate on CT are fungal sinusitis and dense secretions.
Diagnostic nasal endoscopy, Functional endoscopic sinus surgery, Sinonasal pathologies
Introduction
Sinonasal imaging has progressed in an orderly fashion as each generation of imaging modality has advanced gradually on the domain of the former generation. New generation of imaging modalities have completely changed the picture of sinonasal imaging. Previously plain radiography was most commonly done, now it’s been replaced by Computed Tomography (CT) as per endoscopic sinus surgeon requirement for greater anatomic precision [1].
The nasal passage and paranasal sinuses plays host to a wide spectrum of diseases and conditions which can be collectively termed as sinonasal disease. The sinonasal pathologies include broad spectrum of conditions ranging from inflammatory to neoplasms, both benign and malignant. The radiological evaluation of sinonasal diseases is very essential as the clinical findings in these cases may be non-specific [2,3]. Available imaging techniques include plain radiography, CT, Magnetic Resonance Imaging (MRI), and Positron Emission Tomography (PET).
Each of these modalities has certain advantages and disadvantages. The plain films are no longer considered to be a part of the primary imaging armamentarium as they give only an outline of the anatomy and underlying pathology [4]. The CT and MRI have the advantage of being able to show fine anatomic detail in serial tomographic section, thus, eliminating the gross volume averaging inherent in plain films [4].
CT has become the investigation of choice for radiological diagnosis of nasal and sinus diseases [5] as CT images clearly show air spaces, opacified sinuses and fine structural architecture of bony anatomy. Multidetector CT (MDCT) allows assessment of the patency of sinonasal passages and shows the effect of anatomic variants, inflammatory disease or both on patency. MDCT can show anatomic structures that are not visualised by physical examination or diagnostic nasal endoscopy and is, hence, the study of choice for the surgeon who is considering functional endoscopic sinus surgery [6].
CT also plays an important role in excluding the existence of aggressive infections or neoplasms with features of extra-sinus extension, osseous destruction and local invasion. MRI can be done in cases of complications of sinusitis, extra sinus extension of malignancy and to evaluate intracranial extension [6]. CT is superior to MRI in evaluating fine bone details, fibro-osseous lesions of PNS and sinofacial trauma.
CT aids in the diagnosis and management of recurrent and chronic sinonasal disease by determining the distribution and extent of disease. CT is best at defining the complex sinonasal anatomy and anatomic variations that are inaccessible by physical examination or endoscopy because of its 3D high resolution [7].
CT is the investigation of choice for pre-operative evaluation of the nasal cavity and paranasal sinuses and is the gold standard for description of inflammatory sinus disease resulting from obstruction [8]. Coronal CT images closely correlates with the surgical approach [9]. Therefore, CT is the preferred study for Functional Endoscopic Sinus Surgery (FESS) because coronal images mimic the appearance of the sinonasal cavity from the perspective of the endoscope [10].
CT helps in the diagnosis of the anatomic variations that may lead to intra-operative and post-operative FESS complications and reduces the mortality and morbidity of patients. A combination of CT and diagnostic endoscopy has become the mainstay in evaluation of the sinonasal diseases. Hence, CT has immense value and offers standard imaging of sinonasal diseases [11]. This study was conducted to characterise various benign and malignant sinonasal lesions with the help of various CT parameters and correlate CT finding with histo-pathological findings and diagnostic nasal endoscopy/ functional endoscopic sinus surgery and evaluate sensitivity and specificity of CT in diagnosis of sinonasal diseases (in cases where those investigations were done).
Materials and Methods
This hospital based prospective study was carried out in Department of Radio diagnosis of AVBRH hospital from August 2014 to May 2016. Institutional Ethical Approval was obtained for the study.
The sample size was calculated by the formula nSe = Z2α/2 Sen (1-Sen) ÷ d2 × Prev
For α= 0.05, Zα/2 is inserted by 1.96; Sen and Prev are the pre-determined values of sensitivity and prevalence of disease respectively and d as the precision of estimate (i.e., the maximum marginal error) is pre-determined by clinical judgment of investigators [12].
The pre-determined values of sensitivity were 89.4% (the overall sensitivity of CT obtained in previous study [11]) and prevalence of disease 20.8 (prevalence of sinonasal diseases in AVBRH hospital, Wardha). Marginal error was d 0.10.
1.96x 1.96 x .894 x.106/ 0.10x 0.10 x 0.208 = 175
The 175 patients with clinically suspected sinonasal pathologies referred to Department of Radio diagnosis from ENT Department were included in the study. Patients with allergy to contrast agent and pregnant women were excluded from the study. Informed consent from the patients was received.
CT machine and techniques
The CT was done using Philips 16 Slice BRILLIANCE 190P MDCT and images were acquired in both axial and coronal planes. Post contrast study was done in those who required further evaluation.
Patient position was supine for axial and coronal sections. Slice thickness for axial and coronal planes was 3mm and inter-space was 3mm, exposure factors used were 120kvp and 60 mAs. Scan time was 1.5sec. Soft tissue window level and width (50/200) and bone window level and width (350/2500). Contrast agent Omnipaque 350 was used if indicated and consent was obtained from the patient.
CT findings were evaluated in all the patients and characterisation of the various sinonasal lesions were done with the help of various CT parameters.
Out of 175 patients, 154 patients had further undergone either nasal endoscopy/FESS or histopathological examination and rest 21 were treated medically.
Clinical diagnosis and CT diagnosis was correlated with final diagnosis which was obtained on basis of nasal endoscopy/FESS and histopathological findings in these 154 patients.
Statistical analysis was done by using descriptive and inferential statistics using Test statistics (sensitivity, specificity, PPV, NPV and accuracy). Chi-Square test and Z-test for single proportions. Software used in the analysis was SPSS 17.0 version and graph pad prism 6.0 version and p < 0.05 was considered as statistically significant. Our study included 110 males and 65 females aged between 6 months and 85 years, as all the patients with suspected sinonasal pathologies presented during the specified period of study were included without taking age as criteria for exclusion. The most common symptom with which the patients presented were nasal obstruction and nasal discharge. On basis of CT findings, the various sinonasal pathologies were categorised into congenital/developmental, inflammatory and neoplastic conditions.
Results
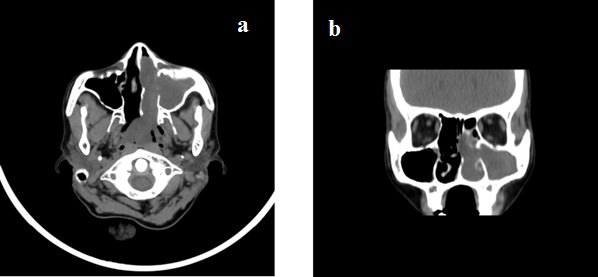
Age distribution of patients is shown in [Table/Fig-1]. Sex distribution is shown in [Table/Fig-2]. All the 175 patients who had undergone CT, were categorised according to aetiology into congenital/developmental, inflammatory and neoplastic based on CT findings as shown in [Table/Fig-3]. The maxillary sinus was most commonly affected sinus. Most common anatomical variations were Deviated Nasal Septum (DNS) and concha bullosa. The distribution of inflammatory cases is shown in [Table/Fig-4]. The most common inflammatory pathology was sinusitis [Table/Fig-5] followed by sinonasal polyps [Table/Fig-6a,b].
Age-wise distribution of patients.
| Age in years | Number (N=175) | Percentage |
|---|
| Male | Female | Total |
|---|
| 0-10 | 3(1.71%) | 1(0.57%) | 4 | 2.29 |
| 11-20 | 17(9.71%) | 11(6.29%) | 28 | 16.00 |
| 21-30 | 26(14.86%) | 18(10.29%) | 44 | 25.14 |
| 31-40 | 24(13.71%) | 16(9.14%) | 40 | 22.86 |
| 41-50 | 14(8%) | 9(5.14%) | 23 | 13.14 |
| 51-60 | 14(8%) | 6(3.43%) | 20 | 11.43 |
| 61-70 | 7(4%) | 3(1.71%) | 10 | 5.71 |
| >70 | 5(2.86%) | 1(0.57%) | 6 | 3.43 |
| Mean ±SD | 110(62.86%) | 65(37.14%) | 175 | 100.00 |
| 2-value | 2.48, p-value=0.92, NS, p>0.05 |
Sex-wise distribution of patients.
| Sex | Number of patients | Percentage |
|---|
| Male | 110 | 62.86 |
| Female | 65 | 37.14 |
| Total | 175 | 100.00 |
Characterisation of the various sino nasal lesions on basis of CT parameters.
| Aetiology | Number of cases | Percentage |
|---|
| Congenital/ developmental | 3 | 1.71% |
| Inflammatory | 135 | 77.14% |
| Neoplastic | 37 | 21.14% |
| Total | 175 | 100% |
Distribution of cases with inflammatory aetiology.
| Inflammatory/ infective | Number of cases | Percentage | Z-value |
|---|
| Sinusitis (other than fungal) | 71 | 40.57% | 10.93,S |
| Sinonasal polyps | 41 | 23.43% | 7.32,S |
| Sinusitis + polyps | 15 | 8.57% | 4.05,S |
| Fungal | 4 | 2.29% | 2.02,S |
| Mucocele | 1 | 0.57% | 1.00,NS |
| Rhinoscleroma | 2 | 1.14% | 1.42,NS |
| Total | 134 | 76.57% | 23.92,S |
Left antrochoanal polyp: Axial and coronal CT image showing homogeneous soft tissue attenuating mass extending from antrum to choana with widening of maxillary ostium.
Out of the 38 neoplastic pathologies, 21 were diagnosed as benign and 17 as malignant on CT as shown in [Table/Fig-7]. The distribution of benign and malignant cases is shown in [Table/Fig-8,9].
Distribution of neoplastic cases.
| Type of lesion | Number of cases | Percentage |
|---|
| Benign | 21 | 12.00% |
| Malignant | 17 | 9.71% |
| Total | 38 | 21.71% |
Distribution of cases of benign neoplasms.
| Type of lesion | Number of cases | Percentage | Z-value |
|---|
| Nasopharyngeal angiofibroma | 7 | 4.00% | 2.70,S |
| Fibrous dysplasia | 4 | 2.29% | 2.02,NS |
| Inverted papilloma | 4 | 2.29% | 2.02,NS |
| Capillary haemangioma | 3 | 1.71% | 1.75,NS |
| neurofibroma | 1 | 0.57% | 1.00,NS |
| Ivory osteoma | 1 | 0.57% | 1.00,NS |
| Squamous papilloma | 1 | 0.57% | 1.00,NS |
Distribution of cases of malignant neoplasms.
| Type of malignancy | No of cases | Percentage |
|---|
| Squamous cell carcinoma of maxilla | 8 | 4.57 |
| Nasopharyngeal carcinoma | 4 | 2.29 |
| Nasal carcinoma | 5 | 2.86 |
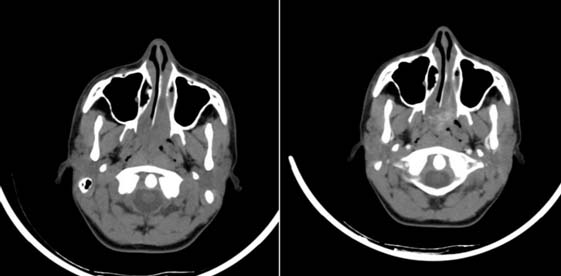
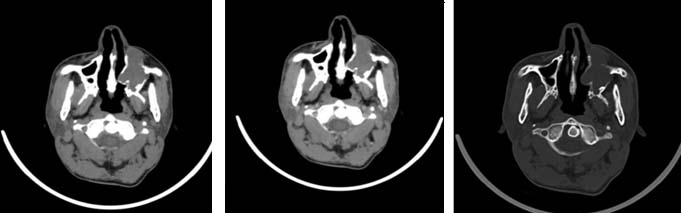
The most common benign pathology was nasopharyngeal angiofibroma [Table/Fig-10a,b] followed by inverted papilloma [Table/Fig-11a-c]. The most common malignant pathology found in present study was squamous cell carcinoma of maxillary sinus [Table/Fig-12a-c]. All of them were histologically proven.
Nasopharyngeal angiofibroma: Axial plain and post contrast CT shows soft tissue attenuating mass in nasopharynx widening the sphenopalatine foramen and showing intense post contrast enhancement.
Right inverted papilloma: Axial and Coronal CT shows lobulated soft tissue attenuating mass in right nasal cavity extending into maxillary sinus with adjacent bony remodeling.

Squamous cell carcinoma: CT images show soft tissue enhancing mass in left maxillary sinus with bony destruction of surrounding walls and extra sinus extension.
CT had diagnosed bone involvement in all the cases as shown in [Table/Fig-13]. Correlation of CT findings with final diagnosis which is obtained from histopathological findings, diagnostic nasal endoscopy/FESS is shown in [Table/Fig-14].
| Bone involvement | Number | Percentage | Sensitivity | Specificity |
|---|
| In clinical diagnosis | 3 | 1.71 | 12% | 97.35% |
| CT Diagnosis | 25 | 14.29 | 100% | 100% |
| Final diagnosis | 25 | 14.29 | - | - |
Correlation of CT with final diagnosis -an evaluation.
| Parameters | Sensitivity | Specificity | PPV | NPV | Accuracy | p-value | Result |
|---|
| Congenital | 100% | 100% | 100% | 100% | 100% | 0.0001 | Signi-ficant |
| Chronic sinusitis | 98.3%% | 97.8% | 96.77% | 98.91% | 98.05% | 0.0001 | Significant |
| Fungal sinusitis | 60% | 99.3% | 75.0% | 98.67% | 98.05% | 0.0001 | Significant |
| Polyp | 94.4% | 98.1% | 94.44% | 98.31% | 97.40% | 0.0001 | Significant |
| Other inflammatory conditions | 90.9% | 99.3% | 90.91% | 99.30% | 98.70% | 0.0001 | Significant |
| Benign neoplasms | 90.9%% | 99.2% | 95.24% | 98.50% | 98.05% | 0.0001 | Significant |
| Malignant neoplasms | 94.1% | 99.3% | 94.12% | 99.27% | 98.70% | 0.0001 | Significant |
Discussion
Recently CT has become the best diagnostic modality for evaluation of nasal cavity, paranasal sinuses and for demonstrating various sinonasal diseases. Acute sinus infection is evaluated by clinical assessment, whereas, persistent sinus disease refractory to medical therapy is investigated by CT [13–16]. This was a prospective correlational descriptive clinical study carried out on 175 symptomatic sinus diseased patients who had undergone CT imaging of paranasal sinuses in both coronal and axial sections. In present study, the patient’s age ranged between 6 months - 85years which was consistent with study done by Harika Surapaneni et al., and Nepal A et al., [17,18]. Most patients were in the 2nd and 3rd decades of their life with male: female ratio of 1.6:1 which is comparable to study done by Bist S et al., [19].
Most common sinus involved was maxillary sinus followed by anterior ethmoid, posterior ethmoid, frontal and sphenoid sinuses. Present study correlates well with studies done by Suthar et al., [20] Chaitanya CS et al., [11] Kushwah APS et al., where maxillary sinus was most commonly involved [21]. In all the studies sphenoid was least involved, which is also observed in the present study. Commonest pattern of inflammation was osteomeatal unit pattern followed by sinonasal polyposis which was also observed in study by Maru YK et al., [22].
The various sinonasal pathologies diagnosed on CT are classified based on their imaging features. Most common sinonasal pathology in present study was inflammatory (77.14%) followed by benign neoplastic (12%) and malignant lesions (9.7%). Similar findings were also found in studies done by Vijay Prabhu et al., Khan N et al., Vikas Dhillon et al., [23–25]. The most common inflammatory pathology was sinusitis followed by polyps [Table/Fig-4], which was also found in study done by Azzam MA, Salami et al., [26] accounting to 33.3% and 20% resepectively. Sinusitis was also most common in study doneby Vijay Prabhu et al., accounting to 56% [23].
The most common benign pathology was nasopharyngeal angiofibroma [Table/Fig-6] which was also seen in study done by Mohammed A. Gomaa et al., [27]. The most common malignant pathology was squamous cell carcinoma of maxillary sinus [Table/Fig-7] which was also seen in studies done by in Azzam MA. Salami et al., study [26], Mohammed A. Gomaa and Hammad MS and Chow et al., [27,28].
Sensitivity and specificity of CT in diagnosing fungal sinusitis was 60% and 99.3% respectively. The sensitivity of CT in diagnosing fungal sinusitis as described in literature was 76% by Zenreich SJ et al., which was a retrospective study [29]. However, CT plays a major role in diagnosing invasive nature of fungal sinusitis like extra sinus spread to adjacent structures, bone destruction or erosion.
In this study CT detected the bone destruction or erosion in all the 25 patients, which was confirmed on endoscopy/FESS. The sensitivity and specificity of CT to detect involvement of bone such as bone erosion or destruction was 100%. Therefore, the CT has definite advantage over the MRI in assessing the involvement of bones. The p-value in all instances was <0.05 i.e., <0.0001, indicating the significance of the findings.
Thus, CT plays an important role in diagnosing and also in adding important findings for the better management of the patients with sinonasal diseases.
Limitation
The potential drawback of CT in the present study was noted in diagnosis of invasive fungal sinusitis. However, the invasiveness and extent of the disease was correctly diagnosed on CT. Early sinonasal polyps were missed on CT which were diagnosed on diagnostic nasal endoscopy.
Conclusion
This study emphasizes the significant role of CT in diagnosis and characterisation of various sinonasal diseases. It proves the better sensitivity and specificity of CT in evaluation of various sinonasal pathologies in symptomatic patients for the diagnosis, staging and thereby better planning of management. CT is the best modality of choice for evaluating osteomeatal complex anatomy, variations and for assessing bony changes in various sinonasal diseases.
[1]. Yousem DM, Imaging of sinonasal inflammatory diseaseRadiology 1993 188(2):303-14. [Google Scholar]
[2]. Zinreich JS, Functional anatomy and Computed Tomography imaging of the paranasal sinusesThe American Journal of the Medical Sciences 1998 316(1):2-12. [Google Scholar]
[3]. Mafee MF, Endoscopic sinus surgery: Role of the RadiologistAJNR Am J Neuroradiol 1991 12(5):855-60. [Google Scholar]
[4]. Fatterpekar G, Delman B, Som P, Imaging the paranasal sinuses: Where we are and where we are goingAnat Rec 2008 291(11):1564-72. [Google Scholar]
[5]. Zinreich S, Rhinosinusitis: Radiologic diagnosisOtolaryngology - Head and Neck Surgery 1997 117(3):27-34. [Google Scholar]
[6]. Miller JC, Imaging for Sinusitis. Radiology Rounds A Newsletter for Referring Physicians Massachusetts General Hospital Department of Radiology 2009 7(8) [Google Scholar]
[7]. Momeni AK, Roberts CC, Chew FS, Imaging of chronic and exotic sinonasal disease: ReviewAJR 2007 189:S35-S45. [Google Scholar]
[8]. Duvoisin B, Landry M, Chapuis L, Krayenbuhl M, Schnyder P, Low-dose CT and inflammatory disease of the paranasal sinusesNeuroradiology 1991 33:403-06. [Google Scholar]
[9]. Spector SL, Berstein IL, Li JT, Joint task force on practice parameters, joint council of allergy, asthma and immunology. Parameters for the diagnosis and management of sinusitisJ Allergy Clin Immunology 1998 102(6, part 2):s107-44. [Google Scholar]
[10]. Gotwald TF, Zinreich SJ, Corl F, Fishman EK, Three-dimensional volumetric display of the nasal ostiomeatal channels and paranasal sinusesAJR 2001 176(1):241-45. [Google Scholar]
[11]. Chaitanya CS, Computed tomographic evaluation of diseases of paranasal sinusesInternational Journal of Recent Scientific Research 2015 6(7):5081-86. [Google Scholar]
[12]. Hajian-Tilaki K, Sample size estimation in diagnostic test studies of biomedical informaticsJournal of Biomedical Informatics 2014 48:193-204. [Google Scholar]
[13]. Joshua BZ, Sachs O, Shelef I, Vardy-Sion N, Novack L, Vaiman M, Comparison of clinical data, CT, and bone histopathology in unilateral chronic maxillary sinusitisOtolaryngol Head Neck Surg 2013 148(1):145-50. [Google Scholar]
[14]. Groppo ER, El-Sayed IH, Aiken AH, Glastonbury CM, Computed tomography and magnetic resonance imaging characteristics of acute invasive fungal sinusitisArch Otolaryngol Head Neck Surg 2011 137(10):1005-10. [Google Scholar]
[15]. Shahbazian M, Jacobs R, Diagnostic value of 2D and 3D imaging in odontogenic maxillary sinusitis: a review of literatureJ Oral Rehabil 2012 39(4):294-300. [Google Scholar]
[16]. Maillet M, Bowles WR, McClanahan SL, John MT, Ahmad M, Cone-beam computed tomography evaluation of maxillary sinusitisJ Endod 2011 37(6):753-57. [Google Scholar]
[17]. Surapaneni H, Sisodia SS, Aaetiology, diagnosis and treatment of chronic rhinosinusitis: a study in a teaching hospital in TelanganaInt J Otorhinolaryngol Head Neck Surg 2016 2:14-17. [Google Scholar]
[18]. Nepal A, Chettri ST, Joshi RR, Karki S, Benign sinonasal masses: A clinicopathological and radiological profileKathmandu Univ Med J 2013 41(1):4-8. [Google Scholar]
[19]. Bist S, Kusum A, Varshney S, Clinico-pathological profile of sinonasal masses: An experience in tertiary care hospital of UttarakhandNational Journal of Maxillofacial Surgery Natl J Maxillofac Surg 2012 3(2):180 [Google Scholar]
[20]. Bhumikaben P. Suthar, Divya Vaidya, Pukhraj P. Suthar, The Role of Computed Tomography in the Evaluation of Paranasal Sinuses LesionsInt J Res Med 2015 4(4):75-80. [Google Scholar]
[21]. Kushwah APS, Bhalse R, Pande S, CT evaluation of diseases of Paranasal sinuses & histopathological studiesInt J Med ResRev 2015 3(11):1306-10.doi: 10.17511/ijmrr. 2015.i11.237 [Google Scholar]
[22]. Maru YK, Gupta Y, Concha bullosa: Frequency and appearances on sinonasal CTIndian Journal of Otolaryngology and Head and Neck Surgery 2000 52(1):40-44. [Google Scholar]
[23]. Prabhu VR, Adaikappan M, Sethurajan S, Computed Tomographic Evaluation of Paranasal Sinus and PathologiesJournal of Evolution of Medical and Dental Sciences 2015 4(33):5741-47. [Google Scholar]
[24]. Khan N, Zafar U, Afroz N, Ahmad SS, Hasan SA, Masses of nasal cavity, paranasal sinuses and nasopharynx: A clinicopathological studyIndian J Otolaryngol Head Neck Surg 2006 58(3):259-63. [Google Scholar]
[25]. Dhillon V, Dhingra R, Davessar JL, Chaudhary A, Monga S, Kaur M, Arora H, Correlation of clinical, radiological and histopathological diagnosis among patients with sinonasal massesInternational Journal of Contemporary Medical Research 2016 3(6):1612-15. [Google Scholar]
[26]. Azzam M.A, Salami Unilateral Sinonasal Disease: analysis of the clinical, radiological and pathological featuresJ Fac Med Baghdad 2009 51(4):372-75. [Google Scholar]
[27]. Gomaa MA, Hammad MS, Abdelmoghny A, Magnetic Resonance Imaging Versus Computed Tomography and different imaging modalities in evaluation of sinonasal neoplasms diagnosed by histopathologyClinical Medicine Insights Ear, Nose and Throat 2013 6:9-15. [Google Scholar]
[28]. Chow JM, Leonetti JP, Mafee MF, Epithelial tumors of the paranasal sinuses and nasal cavityRadiolClin North Am 1993 31:61-74. [Google Scholar]
[29]. Zinreich SJ, Kennedy DV, Malat J, Fungal sinusitis: diagnosis with CT and MR imagingRadiology 1988 169(2):439-44. [Google Scholar]