Spinal traumas are common and leading problem in orthopaedic practice. The individuals are at a risk of high energy trauma in modern era [1–3]. Thoracolumbar is the most common segment involved in the vertebral column followed by cervical segment in patients with spinal injuries. It constitutes 67 to 80% of all spinal injuries [4].
Unstable thoracolumbar burst fractures are serious injuries of concern which if left untreated, may result in marked morbidity and disability to the patient such as motor and sensory disturbance, bladder and bowel disturbances, erectile dysfunction, deformities like kyphosis, scoliosis as a result of neurological injury/spinal instabilities. The patients are also prone to bed sores, Deep Venous Thrombosis (DVT) and pulmonary infections.
The primary focus of management in spinal injuries is the stabilization of the injured spinal column, deformity correction and decompression of neural structures facilitating their recovery. The goal should be early mobilization of the patient to reduce disability.
In this study, we have analysed the outcomes of unstable thoracolumbar burst fractures stabilized with short segment posterior instrumentation with transpedicular screws.
Materials and Methods
This was a prospective interventional study undertaken in New Civil Hospital, Surat from January 2014 to December 2015 after obtaining clearance from institutional ethics committee before initiating the study.
Sample Size
Thirty two adult patients with acute thoracolumbar injuries who gave the consent for surgery were included as the study sample. A detailed history was obtained for evaluating the mode of trauma, American Spinal Injury Association (ASIA) grading [5], sensory level and to check for any spinal deformity [6]. All fractures were classified according to the Arbeitsgemeinschaftfür Osteosynthesefragen (AO) classification system [7].
All patients more than 18 years of age with unstable thoracolumbar burst fractures between T10 – L2 with or without neurological deficit, Thoracolumbar Injury Classification and Severity Score (TLICS) [7] of more than 4 and duration of < 2 weeks were included in the study.
Patients with head injury, concomitant spinal fractures at other levels and pathological fractures were excluded from the study.
Pre-operative Work-up
Plain radiograph (static and dynamic wherever necessary)
Magnetic Resonance imaging.
The following measures were taken using plain X-rays of the injured spine:
Sagittal angle.
Sagittal index.
Procedure
The patient was positioned prone on a 4 post spinal frame. A posterior midline incision was made centering over the involved spinal unit and extending 2 levels above and below. The posterior elements of vertebrae one level above and one level below were exposed extending laterally till the tips of transverse process.
Transpedicular screws were inserted by intersection method via free hand technique one level above and one level below the fractured vertebrae. For the lumbar vertebra entry point was the intersection of pars inter-articularis and midline of the transverse process. The entry point of the pedicle screw for the lower thoracic segments was defined after determining the intersection of the mid portion of the facet joint and the superior edge of the transverse process.
An intermediate screw was inserted in the fractured vertebrae on both sides whenever possible by the same technique. All the screws were inserted and after giving appropriate curvature to the rod, assembly was constructed. Distraction was applied for correction of the deformity and to achieve indirect decompression following which the construct was tightened. None of the patients underwent laminectomies and fusion. A thorough homeostasis was achieved and the wound was closed in layers over drain. Clean dressing was applied.
Post-operative treatment
All patients were given post-op intravenous antibiotics for 3 days. Physiotherapy was started from 1st day post-operatively. On the 2nd day, patients were allowed to roll on side to side. They were allowed to sit up and mobilized on a wheel chair with a thoracolumbar brace on 3rd or 4th day post-operatively. Sutures were removed on the 11th day.
Patients wore TLSO (thoracolumbosacral orthosis) braces for about 6 weeks. All patients were given physiotherapy and ambulated as per their neurological recovery. Routine post-operative X-rays were taken prior to discharge. The neurological grading and radiological parameters were recorded at each follow-up visit.
All patients were followed up for a minimum duration of 12 months where clinical, neurological and radiological assessments were done. The patients were advised to undergo implant removal after 1 year.
CASE 1: A 26-year-old male patient having unstable L1 burst fracture after sustaining a fall [Table/Fig-1]. Patient was operated by SSPI with maintenance of reduction at 1 year follow-up [Table/Fig-2,3].
Case 1: # L1 pre-op X-ray.

Case 1: #L1 Immediately post-Op X-ray.
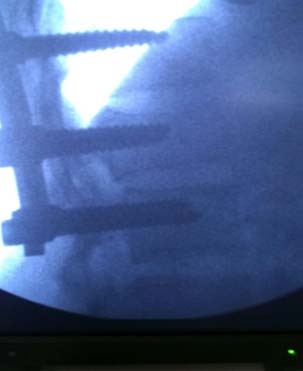
Case 1: At 1 year follow-up X-ray.

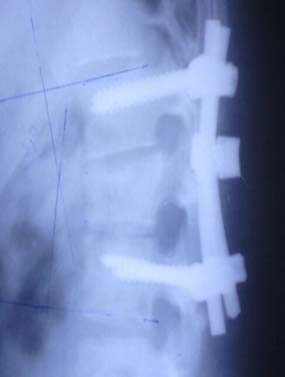
CASE 2: A 24-year-old male patient having unstable L2 burst fracture after a road traffic accident. The pre-op radiograph showed AVH (anterior vertebral height) of 15 mm and segmental kyphosis of 20° [Table/Fig-4]. Patient was operated by SSPI in conventional method without insertion of an intermediate screw [Table/Fig-5]. Immediate post-op showed 6° of lordosis which at 6 months follow-up showed 9° of kyphosis [Table/Fig-6,7].
Case 2: #L2 Pre-op X-ray.

Case 2: #L2 Immediate Post Op X-ray.

At 6 month Follow-up X-ray.

Case 2: At 1 Year Follow-up X-ray.
Statistical Analysis
The data thus obtained was entered in a spread sheet and analysed using Independent t-test for quantitative variables, paired t-test for paired observation and chi-square test for categorical observations. Value of 0.05 was considered as statistical significance level and all the values below that level were considered statistically significant.
Results
The mean age for males was 35.57 ± 11.62 years and for females was 33.56 ± 11.2 years. There were 23 males and 9 females. The most common vertebra involved was T12 (31.25%), followed by L1 (21.88%), L2 (18.75%), T11 (15.62%) and T10 (12.5%). Two third (66%) patients had a fall from height as the mode of injury; whereas, 34% injuries were due to road traffic accident. The mean duration of injury to admission was 2.44 days. The mean duration of injury to surgery was 4.1 days. The mean duration of hospital stay was 10.8 ± 2.77 days. In 65% patients in study group, the duration of injury to surgery was less than or equal to 4 days, whereas in about 35% patients, it was more than 4 days.
The mean regional angle observed during pre-operative stages was 16.0°±5.1°. The mean difference in the regional angle between pre-operative stage and 6th post-op week was 12.2°, between pre-operative and 12th post-op week was 11.95°, between pre-operative and 24th post-op week was 12.05°, between pre-operative and at the end of first year was 11.95°. There was a statistically significant (p<0.05) difference between pre-op and post-operative regional angles.
The mean anterior wedge angle observed during pre-operative stages was 18.0°±6.9°. The mean difference in the anterior wedge angle between pre-operative stage and 6th post-op week was 14.05°, between pre-operative and 12th post-op week was 13.45°, between pre-operative and 24th post-op week was 13.6°, between pre-operative and at the end of 1st year was 13.6°. There was a statistically significant difference (p<0.05) between pre-op and post-operative anterior wedge angles.
The mean vertebral height during the pre-operative stage was 15.2±3.2mm. The mean difference in vertebral height between the pre-operative stage and 6th post-op week was 8.8mm, between pre-op and 12th post-op week was 7.95mm and between pre-op and 24th post-operative week was 7.95mm, between pre-operative and at the end of 1st year was 8.5mm. There was a statistically significant difference (p<0.05) in the vertebral height between pre-operative and post-operative stages.
There was a statistically significant difference in ASIA grading between pre-operative and 12th post-operative week, pre-operative and 24th post-op week, and pre-operative and 1st year follow-up, as shown in [Table/Fig-8]. But there was no statistically difference in ASIA grading between pre-operative and 6th post-operative week.
ASIA grading for neurological status in the study group.
| ASIA grade | Pre-operative n (%) | 6th post-op week n (%) | 12th post-op week n (%) | 24th post-op week n (%) | 1 year post-op n (%) |
|---|
| A | 12(37.5) | 10(31.25) | 8(25.0) | 6(18.75) | 5(15.62) |
| B | 5(15.63) | 3(9.38) | 2(6.25) | 3(9.38) | 2(6.25) |
| C | 7(21.88) | 5(15.63) | 4(12.5) | 2(6.25) | 2(6.25) |
| D | 6(18.75) | 5(15.63) | 6(18.75) | 6(18.75) | 4(12.5) |
| E | 2(6.25) | 9(28.13) | 12(37.5) | 15(46.88) | 15(46.88) |
Seven patients were in a state of spinal shock when operated hence they were considered in ASIA grade A.
Pre-op - 6th post-operative week: χ2 value = 5.561 df=4 p-value=0.23
Pre-op-12th post-operative week: χ2 value = 10.05 df= 4 p-value=0.039
Pre-op-24th post-operative week: χ2 value = 15.22 df= 4 p-value=0.004
Pre-op – 1st post-operative year: χ2 value = 17.1 df = 4 p-value = 0.002
Out of the 32 patients, intermediate screw was not inserted in 11 patients who showed gradual decrease in the vertebral height at 1st year post-op follow-up, as shown in [Table/Fig-9].
The effect of intermediate screw.
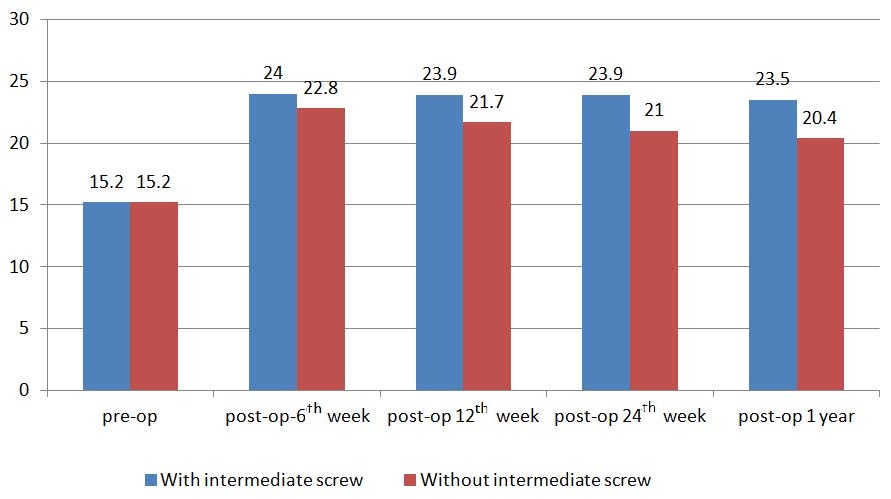
The mean vertebral height of patients with intermediate screw at pre-op was 14.8 mm. The mean vertebral height of patients without intermediate screw at pre-op was 14.7mm. The Mean vertebral height of patients with intermediate screw at immediate post-op was 23.7 mm while the mean vertebral height of patients without intermediate screw at immediate post-op was 22.9mm. The mean vertebral height of patients with intermediate screw at 1 year follow-up was 23.4mm whereas mean vertebral height of patients without intermediate screw at 1 year follow-up: 20.5mm. p-value for this difference by paired t-test is <0.001 which is highly significant.
In 6 patients out of the 21 patients in whom intermediate screws were placed at the fracture level, the Load Sharing Classification was seven which traditionally is an indication for anterior reconstruction. None of these patients showed loss of correction or implant failure. It suggests that the technique of short segmental posterior instrumentation may be useful for treatment of thoracolumbar burst fractures that would otherwise require anterior column reconstruction.
In the entire study, about 22% patients had minor complications - Pressure sores (4), screw impingement (2), and discharging sinus (1) were observed.
Discussion
Acute fracture of the thoracolumbar spine is a major cause of disability in adult population. Posterior transpedicular fixation has been the preferred method for stabilizing acute unstable thoracolumbar fractures [8].
Short segment fixation of the fracture level has replaced the traditional long segment instrumentation to decrease the number of motion segments sacrificed in the fixation process. However, when there is significant disruption of the load-sharing anterior column, the simple one level above and one level below short segment fixation does not ensure adequate stability, resulting in poor reduction in the kyphotic deformity and occurrence of instrument failure [8]. This necessitates more extensive approaches, such as anterior reconstruction via an anterior approach or posteriorly using balloon-assisted vertebroplasty [8].
This study used stabilization of the cases of the unstable thoracolumbar spine injuries with short segment posterior instrumentation.
The mean age of the study group was 35 ± 11 years. The mean age of males was 35.6 years with a SD of 11.6 years and mean age of females’ was 33.6 years with a SD of 11.2 years in this study. These results were almost comparable to a study by Uzumcugil et al., [9]. Alvine et al., in their study found that average age was 31 years with a male predominance [10]. Sasso RC et al., in their study had 77% males and 23 % females with a mean age of 34 years [11]. The mean age of the present study is almost comparable to these studies.
Alvine et al., noted that 52% patients had injury due to fall from height [10]. Uzumcugil et al., noted it as 60% [9]. These results are comparable to the present study in which 65% of the patients had injury due to fall from height.
The most common vertebra involved in this study was T12. Alvine noted that 70% of patients had injury between T11 to L2 [10]. Sasso noted it up to 80% [11].
In this study the mean duration of injury to admission to hospital was 2.4 days, duration of injury to surgery was 4.1 days and mean duration of stay in hospital was 10.8 days. Sasso et al., noted that average time interval between injuries to surgery was 4 days and the hospital stay was 17 days [11]. Uzumcugil et al., noted that average time duration of injury to surgery was 5.6 days and mean duration of hospital stay was 24 days [9]. In this study about 25% of the patients were operated within 4 days of injury and about 75% were operated after 4 days of injury. This difference in time was may be due to the fact that this being a tertiary center the patients were referred from the peripheral centers from distant places wasting valuable time for the much needed surgery. These patients were discharged after stitch removal which accounted for increased hospital duration stay.
The average regional angle during the pre-operative stage was 16.0° ± 5.1° and 4.2° ± 4.1° during the 1st post-operative year.
Nasser MG et al., noted that the kyphotic angle was 23.6° on admission, 7° post-operatively and 11.5° at last follow-up [12]. Alvine et al., noted that sagittal plane angulation was 12° pre-operatively 1° post-operatively and 6° at follow-up [10]. Sasso et al., noted that kyphotic angle was 17.6° pre-operatively, 3.5° post-operatively and 11.6° at latest follow-up [11].
These studies using long segment fixation suggests that short segment fixation is equally efficient in maintaining the achieved correction and hence biomechanical stability, as shown in [Table/Fig-10]. Previous studies have shown that the mean loss of kyphosis correction ranging from 3° to 12° was reported in the clinical results of short segment pedicle screw fixation [13–15]. The mean correction loss in our series was 0.35°, which was similar to those of the series of anterior decompression and stabilization [16]. The improvement achieved in this study is equivalent to those achieved in long segment fixation of above studies. This improvement can be attributed to the intermediate screw. The screw at the fracture level may provide a mass effect and prevent the vertebra from collapsing. It also may help to support anterior column, which is vital for the stability of the construct [17]. This maintenance of correction must be due to the fact that this technique provides the correction of deformity through vertebral endplate augmentation with its buttress effect (bending force) like in the rod-sleeve method, which was used in spinal instrumentation in recent past.
Comparison of kyphotic angle among studies on Thoracolumbar fractures.
| Study | On admission | Post-operative | Follow-up |
|---|
| Nasser MG et al., [12] | 23.6° | 7° | 11.5° |
| Alvine et al., [10] | 12° | 1° | 6° |
| Sasso et al., [11] | 17.6° | 3.5° | 11.6° |
| This study | 16° | 4.2° | 4.55° |
The ASIA grading for the neurological state during pre-operative period; 37.5% were graded as grade A, 15.6% as grade B, 23.9% as C, 18.8% as D and 6.3% as E. During last follow-up grade A was 15.62%, grade B was 6.25%, C was 6.25%, D was 12.5% and E was 46.9%.
Nasser MG et al., noted that patients who had neurological deficits showed at least grade 1 improvement at latest follow-up [12]. Alvine et al., noted that neurological improvement was seen in 50% of cases with 40% improving with 1 grade and 20% with 2 grades and none had decrease in neurological level [10]. Sasso et al., in their study noted that all patients with incomplete neurological deterioration improved at least by 1 grade [11]. In the current study, there was a statistically significant difference in ASIA grading between pre-operative and 1st year follow-up. These results are comparable to anterior fixation for burst fractures of the thoracic and lumbar spine carried out by Kostuik et al., in which mean neurological recovery was 1.6 grades on the Frankel scale [18]. These results are also comparable to studies done by in which anterior decompression was done for thoracolumbar burst fractures, the patients with motor deficits improved by at least one class in motor strength [19].
A total of 78% of the study group had shown no complications. Pressure sores were observed in 12.5% and screw impingement was observed in 6.25% of the study group. A total of 3% patients also showed a discharging sinus. Uzumcugil et al., noted two instances of hardware loosening and 3 misplaced pedicle screws [9].
Intermediate screw was inserted in 21 patients out of 32. This study showed that fracture level screw fixation technique could achieve and maintain correction, regional angle and vertebral height. First of all, this technique provides the correction of deformity through vertebral endplate augmentation with its buttress effect (bending force) like in the rod-sleeve method, which was used in spinal instrumentation at recent past.
The large bone defect created inside the fractured vertebra after height restoration has been speculated to be an important cause for implant failure, which is mostly seen in short-segment fixation. Therefore, augmentation techniques were designed and used for preventing failure. Transpedicular grafting of the injured anterior vertebral body in addition to short-segment fixation has been offered as a possible solution by Knop et al., and Alanay et al., [20,21]. Cementing of the injured vertebra beside the short-segment fixation is another option which was previously mentioned by Cho et al., [22].
We have used the intermediate screw option in the fractured vertebra level as a method of augmentation in the current study. The intermediate screws insertion leads to a stronger 3-point posterior support (instead of a 2-point fixation in the “conventional” method) for the failed anterior column in eligible cases. Insertion of additional screws [intermediate] would only marginally increase the operative time, blood loss and surgical cost as rest of the procedure would remain the same.
The 1 year follow-up does not meet the typical 2-year follow-up criterion which is contemporary for most spine studies. However, this 2-year period is most relevant to studies evaluating spinal arthrodesis. This was not the goal in the current study. The goal was to evaluate the feasibility of fracture reduction, correction and healing. Thus, the shorter duration of follow-up was thought to be adequate.
Limitation
One of the major limitation of this study was that it was a cross- sectional study where a group of comparison was not used to validate the value of short segment posterior instrumentation against long segment fixation. A standard sample size and sampling technique has also not been used.
Conclusion
Short segment posterior instrumentation is a very stable implant construct in maintenance of deformity correction and fracture reduction along with the added advantage of sparing of the motion segments which are sacrificed in the conventional long segment fixation and avoiding the morbidity of anterior approach for anterior reconstruction.
Insertion of the screws at the fracture level improved biomechanical stability by providing additional fixation points which may aid in fracture reduction and kyphosis correction.
Seven patients were in a state of spinal shock when operated hence they were considered in ASIA grade A.
Pre-op - 6th post-operative week: χ2 value = 5.561 df=4 p-value=0.23
Pre-op-12th post-operative week: χ2 value = 10.05 df= 4 p-value=0.039
Pre-op-24th post-operative week: χ2 value = 15.22 df= 4 p-value=0.004
Pre-op – 1st post-operative year: χ2 value = 17.1 df = 4 p-value = 0.002