Peritonitis Following Duodenal Ulcer Perforation in a Newborn: A Case Report
Abdolhamid Amouei1, Fatemeh Ehsani2, Mojtaba Babaei Zarch3, Seyed Mostafa Tabatabaei4, Zahra Ghodratipour5
1 Assistant Professor, Department of Surgery, Shahid Sadoughi Hospital, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
2 Resident, Department of Surgery, Shahid Sadoughi Hospital, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
3 Medical Student, School of Medicine, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
4 Resident, Department of Surgery, Shahid Sadoughi Hospital, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
5 Medical Student, Department of General Practitioner, Shahid Sadoughi University of Medical Sciences, Yazd, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Mr. Mojtaba Babaei Zarch, Medical Student, Shahid Sadoughi Hospital, Shahid Sadoughi University of Medical Sciences, Yazd, Mr, Iran.
E-mail: mojtaba.babaei72@yahoo.com
Duodenal ulcer is an uncommon condition in children, that is why it is not usually considered as the differential diagnosis unless it presents with complications including perforation and haemorrhage. Moreover, duodenal ulcer perforation is an uncommon entity in paediatric age group. Early diagnosis and treatment is crucial in order to improve survival. A three-day-old male neonate was admitted to our hospital because of abdominal distension. The neonate was lethargic. He underwent laparotomy. There was a perforated ulcer, 5×5mm in size, on the anterior aspect of the first part of the duodenum. The perforated ulcer was closed with a single layer. Six-month follow-up revealed no abnormality.
Abdominal distension, Neonate, Peptic ulcer
Case Report
A three-day-old male neonate with 38 weeks gestational age, normal vaginal delivery, weighing about 3150 grams at birth, was admitted to the hospital because of abdominal distension which had begun from the second day of birth. The neonate had a history of jaundice on the first day of life, in which serum bilirubin concentration was 10mg/dl. He had been treated with phototherapy and had been discharged with serum bilirubin concentration 8.5mg/dl on the second day of life. Afterwards, the neonate’s mother had requested further investigations from a paediatrician. Abdominal ultrasonography was planned by paediatrician. As the neonate was lethargic with fever (T= 380C) and there was lack of good sucking, a paediatric surgery consultation had been requested.
Neonate’s mother had a history of ulcerative colitis which had been treated using prednisolone and asacol. She had used high doses of both drugs in early pregnancy and lower doses in late pregnancy. Laboratory tests were as follows: WBC=14200, HCT=46.4%, Hb=16.1, Bilirubin=9.2, Blood group=B+. ABG analysis was as follows: pH=7.42, pO2=76, pCO2=35 and O2 Saturation=95%. There was no family history of peptic ulcer. He was started on intravenous fluids and antibiotics. No steroids were ever administered to the baby.
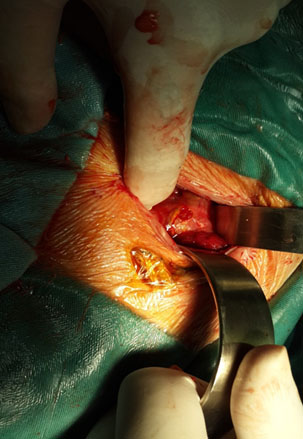
On examination, vital signs were as follows: Blood pressure 60/40, heart rate 170 beats/min, respiratory rate 76 breaths/min and axillary temperature 37.50C. The patient was pale in general appearance. Respiratory distress, tachypnea and severe abdominal distension existed. Bowel sounds were absent on auscultation. There was generalized abdominal tenderness. Neonatal reflexes were weak. Abdominal and chest X-ray were performed. Chest X-ray showed air below the diaphragm [Table/Fig-1] perforation of an organ was suspected. After administration of fluids and antibiotics, neonate underwent laparotomy. Laparotomy was performed with classic transverse incisions above the umbilicus. Large amounts of bile and gas were in the abdominal cavity and pelvic inflammation was present in intestines with a little fibrin. On exploration, there was a perforated ulcer, 5×5mm in size, on the anterior aspect of the first part of the duodenum [Table/Fig-2] which was quite sharp without necrosis. The perforated ulcer was closed with a single layer of absorbable suture (vicryl 1). The abdominal wall was repaired. No drains were used. The patient was transferred to the Neonatal Intensive Care Unit (NICU). The feeding was started after 5 days and the patient was discharged after 9 days with a good general condition. Six-month follow-up revealed no abnormality. After discharge, serum gastrin was checked which was normal: 4.5pmol/L (children<60) and Anti-Helicobacter pylori Ab, was also normal: IgA = 17.7 and IgM = 0.35.
Chest X-ray shows air below the diaphragm.

Intra-operative view shows a peptic ulcer 5x5mm in size.
Discussion
The physicians should be aware of perforated peptic ulcer in children, particularly in the differential diagnosis of shock, gastrointestinal bleeding and acute abdominal pain [1]. The risk factors of duodenal perforation in Low-Birth-Weight (LBW) infants include peptic ulcer, placement of a gastric tube and other unknown reasons [2]. Previously, the causes of duodenal ulcer in neonates were classified into two groups including primary (intrinsic) and secondary (extrinsic). The secondary one is more prevalent in this age group, depending on the aetiology [1,3]. Spontaneous Intestinal Perforation (SIP) is a cause of neonatal intestinal perforation especially in very LBW and extremely LBW neonates [4]. The median gestational age for SIP varies from 25 to 27 weeks. Moreover, the median birth weight varies from 670 to 973g. Risk factors of SIP include prematurity, antenatal and post-natal events. It is important to note that only pre-maturity is well-established risk factor for SIP [5]. The secondary ulcer disease usually occurs in the duodenum part by presentation of life-threatening haemorrhage or perforation. According to one study, 30% of patients presented with perforation [6]. Medications and stress are some external predisposing factors causing secondary ulcer disease. These medications include aspirin, Non-Steroidal Anti-Inflammatory Drugs (NSAIDs) and steroids [1]. In infants, the causes of stress-induced ulcers are traumatic delivery, respiratory or cardiac distress, sepsis, hypoglycaemia or dehydration. In contrast, catastrophic illness and trauma are the main causes of stress-induced ulcers in older children [1]. Kenneth Cruze and Snyder WH reported some cases of acute duodenal perforation. Two patients were receiving corticosteroids (in therapeutic doses) at the time of perforation [6]. It has been reported that, duodenal perforation occurrence has a triphasic pattern in children [3]. During the first week of life to 10 days in neonates, a relatively high acid secretion has been noted. High maternal gastrin level, increased parietal cell and the high acid secretion are probable causes of this condition [7]. Other factors associated with or causing peptic ulcer include: 1) infections which may include dermatitis, otitis media, tuberculosis, nephritis and others; 2) prolonged and difficult delivery; 3) asphyxia with duodenal congestion and mucosal haemorrhage [6]. Acid and pepsin secretion also increases between 10 to 25 weeks of age, related to stress conditions. The next peak is, following primary peptic ulcers, that happen most commonly in children older than six-year-old. The incidence increase in ten year and the clinico-pathological appearance is very similar to that in adults [3]. The administration of steroids does not cause an increase in the gastric secretion of experimental animals. Clinically, however, there seems to be an increased incidence of peptic ulceration with the therapeutic use of this drug. The exact mechanisms in some of these stress factors remain unknown [6]. Barnett M. Miller and Ashok Kumar reported a case of neonatal duodenal perforation which was in the third portion of duodenum and was closed by single layer suture [8]. Man-Chin Hua et al., reported 52 cases of peptic ulcer perforation in children. The anterior wall of the duodenal bulb was the most common perforation site [9]. Laparotomy is often the only way to diagnose patients with secondary ulcer disease because of the presentation of patients with an acute abdomen [1]. Man-Chin Hua et al., concluded that children with perforated peptic ulcer have lower complications and lower mortality rate and have more promising outcome than adult with perforated peptic ulcer. They also reported that, female sex can be a risk factor for poor outcome in paediatric perforated peptic ulcer [9].
Conclusion
Neonatal duodenal perforation is an uncommon condition. It may be presented with abdominal distension. Early diagnosis and treatment is crucial in order to improve survival. This case report emphasizes that paediatricians and paediatric surgeons should be aware of silent abdominal distension resulting from a perforated peptic ulcer in an infant.
[1]. Yadav SK, Gupta V, El Kohly A, Al Fadhli W, Perforated duodenal ulcer: A rare complication of deferasirox in childrenIndian Journal of Pharmacology 2013 45(3):293 [Google Scholar]
[2]. Sugito K, Kusafuka T, Inoue M, Ikeda T, Hagiwara N, Koshinaga T, A rare case of multiple duodenal perforations in early infancyTurk J Paediatr 2008 50:94-97. [Google Scholar]
[3]. Sarin YK, Jacob S, Bhatti W, Duodenal perforation in a neonateIndian Paediatrics 1998 35:1032-33. [Google Scholar]
[4]. Tiwari C, Sandlas G, Jayaswal S, Shah H, Spontaneous Intestinal Perforation in neonatesJournal of Neonatal Surgery 2015 4(2) [Google Scholar]
[5]. Kim ES, Brandt ML, Spontaneous intestinal perforation of the newborn 2016 Available at: http://www.uptodate.com/contents/spontaneous-intestinal-perforation-of-the-newborn. Accessed Jul 2016 [Google Scholar]
[6]. Cruze K, Snyder WH, Acute perforation of the alimentary tract in infancy and childhoodAnn Surg 1961 154:93-99. [Google Scholar]
[7]. Bell JM, Keating JP, Ternberg JL, Bower RJ, Perforated stress ulcers in infantsJ Paediatr Surg 1981 16:998-1002. [Google Scholar]
[8]. Miller BM, Kumar A, Neonatal duodenal perforationJ Paediatr Gastroenterol Nutr 1990 11(3):407-10. [Google Scholar]
[9]. Hua M-C, Kong M-S, Lai M-W, Luo C-C, Perforated peptic ulcer in children: a 20-year experienceJournal of Paediatric Gastroenterology and Nutrition 2007 45(1):71-74. [Google Scholar]