Introduction
Diagnosing heart failure is often a challenge for the healthcare providers due to it’s non-specific and usually subtle physical presentations. The outcomes for treatment are strongly related to the stage of the disease. Considering the importance of early and accurate diagnosis, it is important to have an easy, inexpensive, non-invasive, reliable and reproducible method for diagnosis of heart failure. Recent advancement in radiology and cardiology are supporting the emerging technique of lung ultrasound through B-line evaluation for identifying extravascular lung water.
Aim
To establish lung ultrasound as an easy, inexpensive, non-invasive, reliable and reproducible method for diagnosing Acute Decompensated Heart Failure (ADHF) in emergency department.
Materials and Methods
The study was a cross-sectional, prospective, observational, diagnostic validation study of lung ultrasound for diagnosis of acute heart failure in an emergency department and was performed at Amrita Institute of Medical Science, Kochi, Kerala, India.
A total of 42 patients presenting with symptoms suggestive of acute decompensated heart failure were evaluated by plasma B-type Natriuretic Peptide (BNP), Echocardiography (ECHO) and X-ray. Lung ultrasound was done to look for the presence of B-lines.
Statistical Analysis
Sensitivity, specificity and predictive value of diagnostic modalities were calculated using Mc Nemar’s Chi-square test for the presence and absence of heart failure.
Results
Lung ultrasound showed a sensitivity of 91.9% and a specificity of 100% in diagnosing acute heart failure comparable to plasma BNP which had a sensitivity of 100% and a specificity of 60%. It was also superior to other methods of diagnosing ADHF namely X-ray and ECHO and showed a good association.
Conclusion
Lung ultrasound and its use to detect ultrasonographic B-lines is an early, sensitive and an equally accurate predictor of ADHF in the emergency setting as compared to BNP.
Introduction
Acute Decompensated Heart Failure (ADHF) is defined as an acute worsening of cardiac failure symptoms and is represented through signs of dyspnea, peripheral oedema and lethargy. Even after the extensive improvement and modernization in the management strategies and treatment modalities for acute heart failure, the condition still remains one of the major causes of morbidity and mortality across the globe [1]. The leading reason for hospitalization to the emergency department and death in the cases of acute heart failure has been found to be pulmonary congestion rather than low cardiac output [2].
Diagnosing heart failure is often a challenge for the healthcare providers due to it’s non-specific and usually subtle physical presentations. The outcomes for treatment are strongly related to the stage of the disease [3]. Furthermore, the evidence-based treatment specific to the disease status, provided on correct time, helps in improving patient’s condition as well as prognosis to a great extent. Therefore, early and specific diagnosis of heart failure is crucial for not only reducing the related morbidity and mortality but also for improving patient’s post-treatment life quality along with reducing the overall cost of the disease management [4].
The various established tools for diagnosis of acute heart failure either lack specificity or sensitivity. Physical examination is crucial for the consideration of treatment strategy in the patients with acute heart failure. While this traditional method is high on specificity, it lacks sensitivity to identify elevated cardiac filling pressures [5]. The recently developed Clinical Congestion Scores (CCS) [6,7] for the evaluation of congestion signs in the patient lack the credibility and reliability of extensive research and comparison with established tools. The routinely used chest X-ray and ECG (electrocardiograph) are legitimately specific in identifying certain presentations like cardiomegaly or T-wave abnormality respectively; they lack the sensitivity to exclude the development of heart failure [8]. The amino-terminal portion of the B-type natriuretic peptide (NT-proBNP) has emerged as a strong neurohormonal predictor for heart failure, the utility of its serum testing remains debatable [9]. Thus, definitive diagnosis is hugely reliant on the radio-imaging techniques. Echocardiography with Doppler examination remains the gold standard for the diagnosis of a heart patient. However, it is not always possible to have a quick and extensive echo testing which is evaluated by a radiologist and interpreted by a cardiologist, in the emergency department or even after hours. Additionally, echo may not be indicated for the patients presenting to the emergency department with acute pulmonary oedema or undifferentiated dyspnea, but who have chronic heart failure and established echocardiographic detection of poor left ventricular function [10]. Lung ultrasound can provide sufficient data to verify or preclude the diagnosis of ADHF.
Recent advancement in radiology and cardiology are supporting the newly emerged technique of lung ultrasound through B-line evaluation as an easy, non-invasive and reliable technique for identifying extravascular lung water and thus diagnose acute heart failure [10,11].
Lung ultrasound and significance of B-lines: Lung ultrasound has not been explored extensively for the evaluation of lungs [12]. A normal lung is filled with air and therefore when the ultrasound beam is targeted on the lung, no visible images are obtained. The air in lungs do not allow for any acoustic mismatch which can reflect the beam [13]. Only pleura of a normal lung can be visualized, using lung ultrasound, which appears as a hyperechoic horizontal line moving synchronously with respiration. In case of Extravascular Lung Water (EVLW), subpleural interlobular septa are thickened by oedema which can be detected by the ultrasound beams [10]. These reflected ultrasound beams create comet-tail reverberation artifact known as B-lines or ultrasound lung comets [11]. The B-lines appear as hyperechoic image arising from the pleural line and extending up to the bottom of the screen. These discrete, standing laser-like images move synchronously with respiration. Number of B-lines increase with increasing EVLW and decreasing air content. Multiple B-lines on a sonograph are suggestive of lung interstitial syndrome [11].
Protocol for lung ultrasound to diagnose heart failure: “Lung comet score” are used to define lung ultrasound positivity. First described by Jambrik et al., this lung ultrasound technique focuses on the scanning of anterior and lateral chest walls at fixed locations [14]. The scanning locations are defined at parasternal, mid-clavicular, anterior axillary and middle axillary lines, from the second to the fifth intercostal space on the right chest and from the second to the fourth intercostal space on the left chest, for a total of 28 scan sites [15]. The additional benefit of lung comet scores is that they can be grouped into grades of severity [16] as shown in [Table/Fig-1].
Lung comet score and related severity of cardiac failure.
| Lung comet score | Severity |
|---|
| 5-14 | Mild |
| 15-29 | Moderate |
| >30 | Severe |
There is a dearth of research which can evaluate the application of lung ultrasound for the diagnosis of acute heart failure in an emergency department in an Indian hospital setup.
Aim
The primary aim of the study was to evaluate the effectiveness of lung ultrasound as an easy, inexpensive, non-invasive, reliable and reproducible method for diagnosing acute heart failure in an emergency department compared to BNP. Secondary aim was to correlate the outcomes of lung ultrasound with other established non-invasive diagnostic tools for acute heart failure.
Materials and Methods
The study was a cross-sectional, prospective, observational, diagnostic validation study of lung ultrasound for diagnosis of acute heart failure in an emergency department. The study was also comparative as the test diagnostic tool was compared with established diagnosis methods for acute heart failure including BNP, lung x-rays, diastolic dysfunction and systolic dysfunction.
The study was done on the patients attending the emergency department at Amrita Institute of Medical Sciences, Kochi as well as on those who were acutely shifted to the CCU (Critical Care Unit) of the same institution and was carried out from 1st of January to 31st of December 2014 for a period of 1 year.
Based on the sensitivity and specificity of lung ultrasound as reported by the earlier studies [10,11], the sample size was calculated to be 42 with a 99% confidence interval and a 20% allowable error. Consecutive patients presenting with complaints of breathlessness, lethargy and ankle oedema of over 48 hour’s duration, with no obvious recurrent or self-limiting cause, were enrolled.
Inclusion Criteria
Both male and female patients aging 20-80 years.
Patient having acute onset breathlessness and recent onset fatigue.
Patients with a presence of structural heart disease or conditions that might precipitate ADHF.
Patient with acute myocardial infarction with LV dysfunction.
Exclusion Criteria
Patients with any form of renal dysfunction.
Patients who need dialysis.
Patients with stage D refractory heart failure.
Patients with chest wall injuries.
Other serious co-morbidities such as hepatic disorders, acute respiratory distress syndrome and pneumonia.
Patients who were unable to give consent.
The study protocol was approved by the internal ethics committee and all the procedures were done in accordance to the declaration of Helsinki. Patient’s demographic and clinical data were recorded. Peripheral venous blood samples of the patients were evaluated for BNP/NT-pro-BNP using ELISA Chemiluminescence method. Comprehensive transthoracic echocardiography at rest was performed in all the patients and recorded. Chest X-rays were taken with orthostatic posteroanterior and lateral projections for all patients. Lung ultrasounds by the aforementioned techniques explaining B-lines and lung comet scores were taken and recorded. The blood tests were performed by the lab technician while the lung ultrasound and ECHO were done by the consultant cardiologist.
All the data were analysed and interpreted by two independent cardiologists and radiologists in a blinded manner. The diagnosis of acute heart failure was substantiated by a laboratory estimation of BNP > 266 (according to the normal range set by the in-house laboratory). The presence of structural heart disease, systolic and diastolic dysfunction was noted.
Systolic Dysfunction was defined as the ejection fraction <45%. Diastolic Dysfunction was described as the echocardiographic presence of grade 2,3 and 4 diastolic dysfunctions. X-ray was seen for the presence of signs of pulmonary congestion. Lung ultrasound of all the patients was performed by the same researcher.
Each participant was diagnosed as either having ADHF or not having ADHF (ADHF+ or ADHF−) via medical record and clinical examination. The medical records were reviewed by the treating physician for making the diagnosis who was blinded to the results of lung ultrasound in order to avoid bias.
Statistical Analysis
Sensitivity, specificity and predictive value were calculated using Mc Nemar’s Chi-square test for the presence and absence of heart failure. Sensitivity, specificity and predictive value of lung ultrasound were also compared with other non-invasive methods namely X-ray and ECHO. The p-value of 0.005 was considered significant.
Results
A total of 42 patients (26 males and 16 females) were enrolled in the study over the period of one year. The mean age of the patients was 64.4 years. Out of the 42 patients who were suspected to have acute heart failure, a total of 34 patients were finally diagnosed to have ADHF based on the evaluation of chest x-rays, electrocardiography and BNP assessment.
The cross-section of the patient population was having various cardiac conditions which included ischemic heart disease, hypertensive heart disease, valvular heart disease, Aorto-Aortitis, Eisenmenger syndrome and idiopathic dilated cardiomyopathy.
Vital sign assessment of all the patients showed low oxygen saturation (90-91%), tachycardia (pulse rate more than 100) and elevated breathing rate (RR more than 30). Most of the patients were hypertensive except those patients with cardiomyopathy had lower blood pressure.
Signs of congestion were observed by careful auscultation of heart and lung sounds and physical examination of hepatomegaly as well as peripheral oedema. Jugular venous distension procedure was not applied for assessing congestion.
Lung ultrasound findings had statistically significant association with the diagnosis of ADHF [Table/Fig-2]. The sensitivity of B lines came out to be 91.9% and specificity of 100% positive predictive value of the same came out to be 100% while a negative predictive value of 62.9%. Overall accuracy was 92%.
Comparison of presence of B-line and ADHF.
| B Lines | ADHF (as confirmed by the treating physician) | p-value |
|---|
| Presentn(%) | Absentn(%) |
|---|
| Present | 34 (100.0) | -- | <0.001 |
| Absent | 3 (37.5) | 5 (62.5) |
Plasma BNP was significantly associated with the presence of ADHF [Table/Fig-3]. Sensitivity was 100% for diagnosing ADHF although the specificity was 60%. Positive predictive value was 4.9% and a negative predictive value of 100%. Overall accuracy for the same was 95.2%.
Comparison of BNP presence and ADHF signs.
| BNP | SIGNS OF ADHF | p-value |
|---|
| Presentn(%) | Absentn(%) |
|---|
| Present | 37 (94.9) | 2 (5.1) | <0.001 |
| Absent | -- | 3 (100.0) | |
On testing the correlation of B-lines with other non-invasive methods, it was found that B-lines had a statistically significant association with raised plasma BNP, chest x-rays and diastolic dysfunction but no significant association with the presence of systolic dysfunction [Table/Fig-4].
Comparison of BNP, chest radiograph, Diastolic dysfunction and systolic dysfunction with B-lines.
| Method | B-Lines | p-value* |
|---|
| Presentn(%) | Absentn(%) |
|---|
| BNP | Present | 34 (87.2) | 5 (12.8) | 0.005 |
| Absent | -- | 3 (100.0) |
| Chest Radiograph | Present | 25 (96.2) | 1 (3.8) | 0.003 |
| Absent | 9 (56.2) | 7 (43.8) |
| Systolic Dysfunction | Present | 24 (88.9) | 3 (11.1) | 0.110 |
| Absent | 10 (66.7) | 5 (33.3) |
| Diastolic Dysfunction | Present | 33 (89.2) | 4 (10.8) | 0.003 |
| Absent | 1 (20.0) | 4 (80.0) |
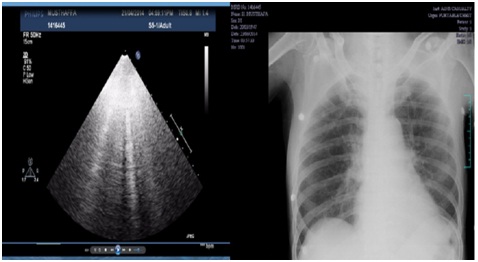
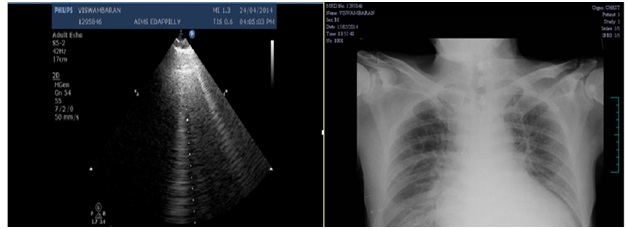
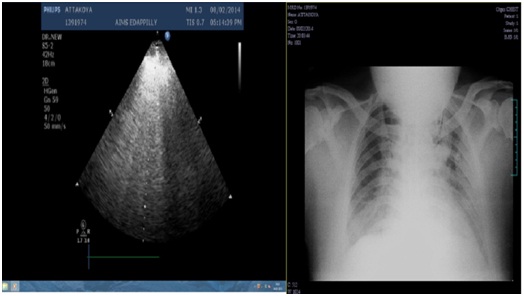
A comparison of chest X-rays and lung ultrasound for explaining severity of the cardiac failure are depicted in [Table/Fig-5,6 and 7].
Chest X-ray and lung ultrasound of same patient showing mild cardiac failure.
Chest X-ray and lung ultrasound of same patient showing moderate cardiac failure.
Chest X-ray and lung ultrasound of the same patient showing severe cardiac failure.
Discussion
The study showed the lung ultrasound interpreted using B-lines is an effective, reliable and reproducible method for the diagnosis of acute cardiac failure in an emergency department setting.
Observing the final diagnosis of enrolled patients as compared with the other radiological findings, the study found that lung comet score obtained using lung ultrasound is an effective tool to identify the degree of pulmonary congestion and therefore, diagnose ADHF in an emergency department. A larger scale study which recruited 340 patients with acute cardiac failure suggested that a lung comet score increases with the severity of dyspnea. It also stated that classification of the lung comet score as mild, moderate, and severe can be correlated with the NYHA (New York Heart Association) functional classification for heart failure. The same study showed increased lung comet scores were also seen with worsening diastolic dysfunction and ejection fraction (r= -0.354, p<0.001) [17].
The present study also established that a lung comet score of 13-15 is a reliable diagnostic cut-off for detecting acute heart failure. This observation was in correlation with the study done by Miglioranza et al., which identified that a lung comet score of 15 or more is quick and reliable apparatus for the assessment of pulmonary congestion in chronic cardiac failure patients [18].
The authors also define a positive lung scan as multiple B-lines (at least 3 B lines <7mm apart) located diffusely across either both anterolateral or both lateral lung surfaces. A comparative study of BNP and lung comet score, as well as B-lines, showed that a score of four B-lines gave the best diagnostic accuracy with a sensitivity of 81% and a specificity of 85%. In the present study, score of five B-lines gave best diagnostic accuracy with a sensitivity of 91.9 % and specificity of 100% positive predictive value.
The most prominent finding of the present study is that the lung ultrasound can effectively rule out pulmonary oedema when there is an absence of multiple B-lines or a low lung comet scores. In this study, lung ultrasound was highly sensitive and specific in making the diagnosis of ADHF similar to plasma BNP. B- lines, as demonstrated by lung ultrasound, had a sensitivity of 91.9% in diagnosing ADHF and a specificity of 100%. Plasma BNP, on the other hand, had a sensitivity of 100% but a specificity of just 60%. This is attributed to the cases of acute exacerbation of COPD (Chronic Obstructive Pulmonary Disease) with Cor-pulmonale in which the BNP-values were high due to right heart failure. The lung ultrasound was found to be extremely useful in triaging the patient in the emergency department who were not having ADHF. Moreover, the absence of ADHF was demonstrated by the lung ultrasound much before the BNP reports were available in the emergency department.
Systolic dysfunction of < 45% by 2D-ECHO was a poor predictor of ADHF having a sensitivity of 70% and a specificity of 80%. On the other hand, it was noted that in patients with acute dyspnea who were suspected to have ADHF, presence of diastolic dysfunction was an important predictor with a sensitivity of 97% but a weak specificity of 80%. The high sensitivity of diastolic dysfunction is attributed to the high LV filling pressure causing pulmonary venous congestion and ADHF. These findings clearly showed that 2D- ECHO, though an essential and helpful investigation for the heart function, lacks the sensitivity and specificity to diagnose ADHF.
Chest X-ray had a poor sensitivity of 70% but a specificity of 100% clearly showing that presence of signs of pulmonary oedema on X-ray more or less clinches the diagnosis. This reflects that there might be a delay in features of frank pulmonary oedema to appear on chest X-ray hence the modality has a low sensitivity.
Furthermore, lung ultrasound also correlated well with X-ray findings and diastolic dysfunction. Although, the association of B-lines with systolic dysfunction was disappointing. Thus, the presence or absence of ECHO findings shall not be taken as a sole predictor of acute decompensation.
The strength of the study lies in the fact that clearly defined lung ultrasound protocol along with lung comet score as well as B-line interpretation is used as an effective tool for not only confirming the presence of acute heart failure but also to preclude this condition in the patients not having it.
Limitation
Small sample size and single center design are the most prominent limitation of the study. Furthermore, detailed assessment of diastolic dysfunction could not be performed in the emergency settings. Correlation of the findings with that of the invasive catheter assessment could not be done.
Conclusion
Despite its limitations, the study was successful in establishing the lung ultrasound as a rapid, sensitive and an accurate predictor of ADHF in the emergency setting as compared to BNP. Along with other non-invasive methods, lung ultrasound can be used as an additive modality for rapid and inexpensive diagnosis of acute heart failure. However, still larger studies are needed to apply the conclusion to the general population.
[1]. Gheorghiade M, Filippatos G, De Luca L, Burnett J, Congestion in acute heart failure syndromes: an essential target of evaluation and treatmentAm J Med 2006 119:S3-S10. [Google Scholar]
[2]. Adams Jr KF, Fonarow GC, Emerman CL, LeJemtel TH, Costanzo MR, Abraham WT, Characteristics and outcomes of patients hospitalized for heart failure in the United States: rationale, design, and preliminary observations from the first 100,000 cases in the Acute Decompensated Heart Failure National Registry (ADHERE)Am Heart J 2005 149:209 [Google Scholar]
[3]. Task FM, McMurray JJV, Adamopoulos S, Anker SD, Auricchio A, Böhm M, ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure 2012Eur Heart J 2012 33:1787-847. [Google Scholar]
[4]. Fonarow GC, Stough WG, Abraham WT, Albert NM, Gheorghiade M, Greenberg BH, Characteristics, treatments, and outcomes of patients with preserved systolic function hospitalized for heart failure: A report from the OPTIMIZE-HF RegistryJ Am Coll Cardiol 2007 50:768 [Google Scholar]
[5]. Hunt SA, Abraham WT, Chin MH, Feldman AM, Francis GS, Ganiats TG, 2009 focused update incorporated into the ACC/AHA 2005 Guidelines for the Diagnosis and Management of Heart Failure in Adults: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines developed in collaboration with the International Society for Heart and Lung TransplantationJ Am Coll Cardiol 2009 53:e1-e90. [Google Scholar]
[6]. Gheorghiade M, Follath F, Ponikowski P, Barsuk JH, Blair JE, Cleland JG, Assessing and grading congestion in acute heart failure: a scientific statement from the Acute Heart Failure Committee of the Heart Failure Association of the European Society of Cardiology and endorsed by the European Society of Intensive Care MedicineEur J Heart Fail 2010 12:423-33. [Google Scholar]
[7]. Rohde LE, Beck-da-Silva L, Goldraich L, Grazziotin TC, Palombini DV, Polanczyk CA, Reliability and prognostic value of traditional signs and symptoms in outpatients with congestive heart failureCan J Cardiol 2004 20:697-702. [Google Scholar]
[8]. Wong GC, Ayas NT, Clinical approaches to the diagnosis of acute heart failureCurr Opin Cardiol 2007 22(3):207-13. [Google Scholar]
[9]. Jessup M, Abraham WT, Casey DE, Feldman AM, Francis GS, Ganiats TG, 2009 focused update: ACCF/AHA guidelines for the diagnosis and management of heart failure in adults A report of the american college of cardiology foundation/american heart association task force on practice guidelines developed in collaboration with the international society for heart and lung transplantationJ Am Coll Cardiol 2009 53(15):1343-82. [Google Scholar]
[10]. Ang S-H, Andrus P, Lung ultrasound in the management of acute decompensated heart failureCurrent Cardiology Reviews 2012 8(2):123-36. [Google Scholar]
[11]. Volpicelli G, Caramello V, Cardinale L, Mussa A, Bar F, Frascisco MF, Detection of sonographic b-lines in patients with normal lung or radiographic alveolar consolidationMed Sci Monit 2008 14(3):CR122-28. [Google Scholar]
[12]. Harrison’s principles of internal medicine 2008 17th editionNew YorkMcGraw-Hill [Google Scholar]
[13]. Lichtenstein DA, General Ultrasound in the Critically Ill 2007 II editionBerlinSpringer Verlag [Google Scholar]
[14]. Jambrik Z, Monti S, Coppola V, Agricola E, Mottola G, Miniati M, Picano E, Usefulness of ultrasound lung comets as a nonradiologic sign of extravascular lung waterAm J Cardiol 2004 93(10):1265-70. [Google Scholar]
[15]. Gargani L, Frassi F, Soldati G, Tesorio P, Gheorghiade M, Picano E, Ultrasound lung comets for the differential diagnosis of acute cardiogenic dyspnoea: A comparison with natriuretic peptidesEur J Heart Fail 2008 10(1):70-77. [Google Scholar]
[16]. Mallamaci F, Benedetto FA, Tripepi R, Detection of pulmonary congestion by chest ultrasound in dialysis patientsJACC Cardiovasc Imaging 2010 3(6):586-94. [Google Scholar]
[17]. Frassi F, Gargani L, Gligorova S, Ciampi Q, Mottola G, Picano E, Clinical and echocardiographic determinants of ultrasound lung cometsEur J Echocardiogr 2007 8(6):474-79. [Google Scholar]
[18]. Miglioranza MH, Gargani L, Sant’Anna RT, Rover MM, Martins VM, Mantovani A, Lung ultrasound for the evaluation of pulmonary congestion in outpatients: a comparison with clinical assessment, natriuretic peptides, and echocardiographyJACC: Cardiovascular Imaging 2013 6(11):1141-51. [Google Scholar]