A Case Report on Unilateral Accessory Humeral Head of Pronator Teres
Suman Verma1, Sulochana Sakthivel2
1 Assistant Professor, Department of Anatomy, JIPMER, Pondicherry, India.
2 Assistant Professor, Department of Anatomy, JIPMER, Pondicherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Suman Verma, Assistant Professor, Anatomy, JIPMER, Pondicherry-605006, India.
E-mail: suman2v@gmail.com
The presence of an accessory muscle in the forearm is likely to compress on the neurovascular structures and has clinical implications. We encountered an accessory humeral head of pronator teres during routine dissection of left upper limb in a male cadaver. The accessory head had fleshy origin from medial supracondylar line, medial intermuscular septum and brachialis fascia. It coursed downwards in the cubital region covering brachial artery and median nerve. Further, it narrowed becoming mostly tendinous and joined with the humeral head of pronator teres. Awareness of accessory head is essential to explain multiple sites of nerve compression. High proximal origin of pronator teres and its course superficial to median nerve makes it more susceptible for distal entrapment neuropathy. Accessory muscles affect surgical field and can be confused with soft tissue pathologies.
Accessory muscle, Neurovascular compression, Supracondylar
Case Report
An accessory muscle was observed in left upper limb of a 50-year-old male cadaver during routine undergraduate dissection class. This muscle was seen in arm, proximal to the humeral head of pronator teres and eventually fusing with it distally. It was subsequently identified as the accessory humeral head of pronator teres.
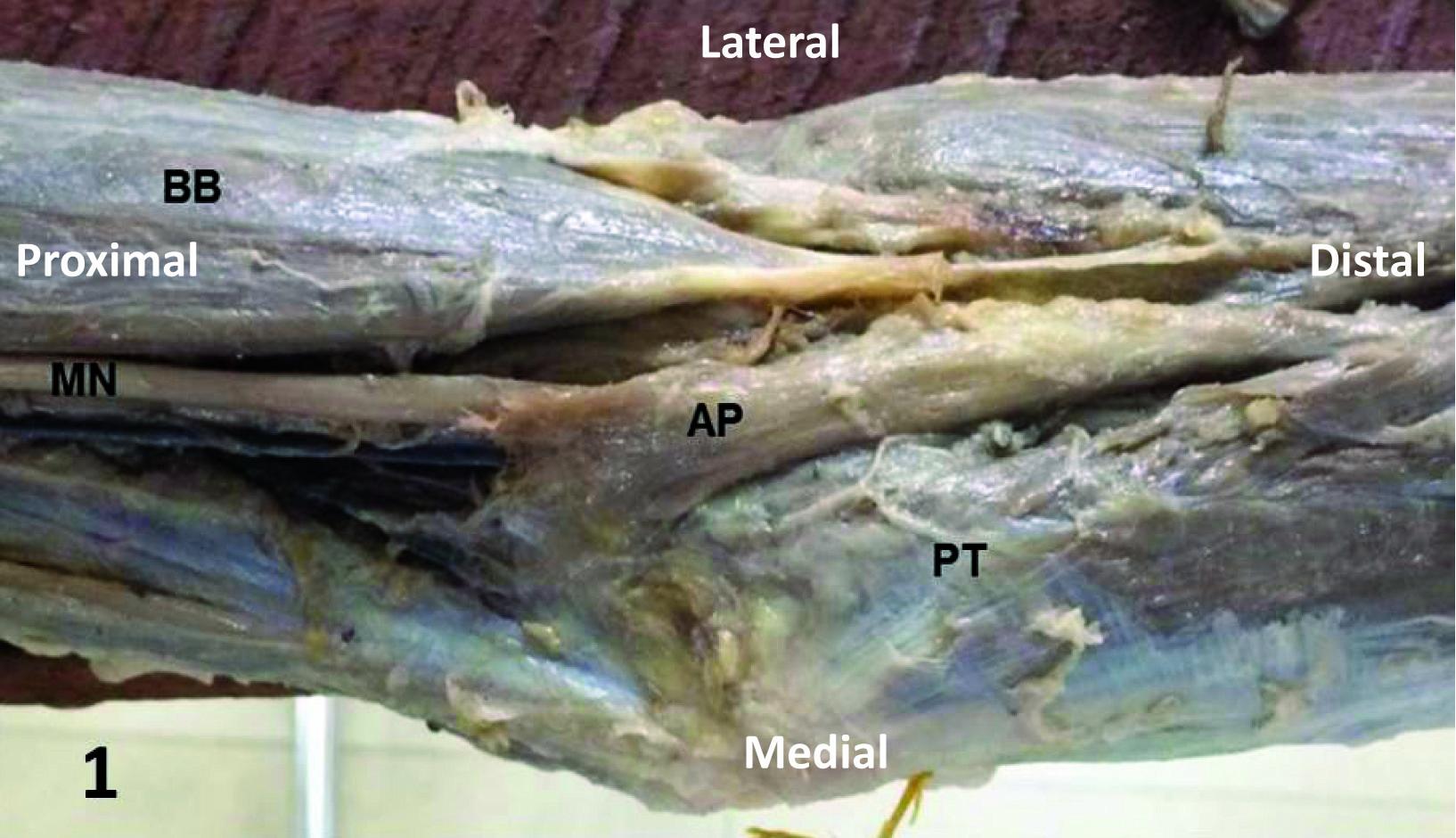
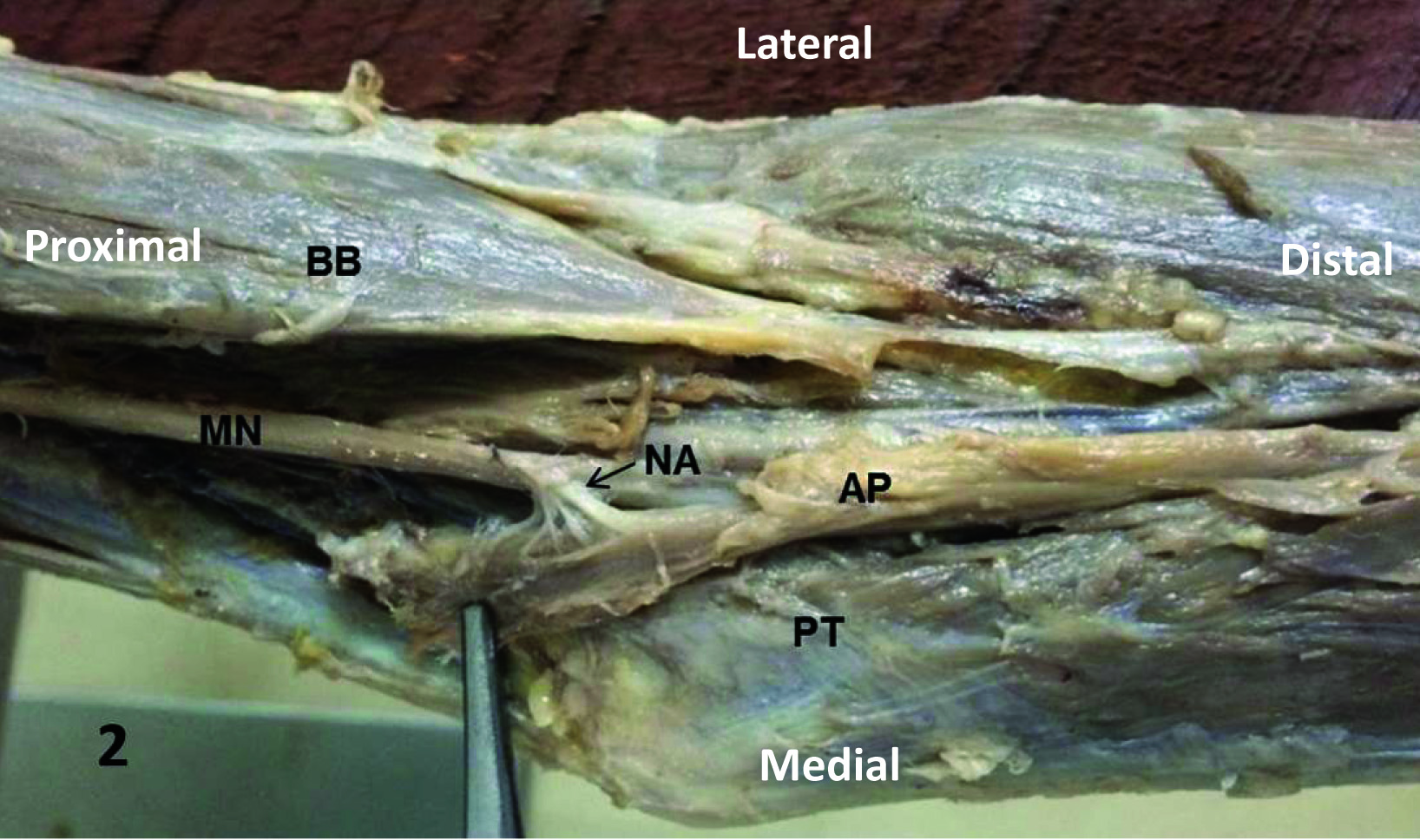
The accessory head had a thin, broad and fleshy origin. It took attachment from medial supracondylar line, medial intermuscular septum and fascia over brachialis. As it coursed downwards and laterally, becoming increasingly narrow, it remained distinct from the humeral head. The muscle was seen arching over median nerve and brachial artery in cubital fossa from medial to lateral side. Further, it tapered becoming mostly tendinous and joined with main humeral head of pronator teres on its lateral aspect in the upper third of forearm [Table/Fig-1]. Just above medial epicondyle, median nerve gave a branch to accessory head while passing under it [Table/Fig-2]. Apart from its branch to accessory head, median nerve did not give any other branch to pronator teres proximal to elbow joint. No further variation in course and branches of median nerve proximal or distal to accessory muscle was observed.
Anterior view of left upper limb showing accessory head of pronator teres. BB – biceps brachii, MN – median nerve, AP – accessory muscle, PT – Pronator teres
Nerve supply to accessory head of pronator teres. BB – biceps brachii, MN – median nerve, AP – accessory muscles, PT – pronator teres, NA – nerve to accessory muscle.
Discussion
Pronator teres is a muscle of flexor compartment of the forearm with two heads of origin - humeral and ulnar. The larger humeral head takes origin from medial supracondylar ridge, common flexor origin, intermuscular septum between it and flexor carpi radialis and antebrachial fascia. It joins with the smaller ulnar head to form a flat tendon and attaches to the lateral aspect of the shaft of radius. The accessory fasciculi of pronator teres may take origin from supracondylar process of humerus, medial intermuscular septum or from biceps brachii and brachialis muscles. Median nerve runs between two heads though in some cases it passes through the humeral head [1].
Multiple structures can compress the median nerve during its course through upper limb. These are brachialis muscle, Struther’s ligament, bicipital aponeurosis, pronator teres, flexor digitorum superficialis, Gantzer’s muscle and vascular structures [2].
According to Nebot et al., incidence of accessory fasciculi of pronator teres is 8.3% and mostly affects ulnar head. These fasciculi were seen taking origin from brachialis (5.0%), from biceps brachii tendon (3.3%), from Gantzer’s muscle (1.6%) or from flexor digitorum superficialis (1.6%) [3]. It has been noted that the median nerve is liable to compression as it passes underneath the hypertrophied muscle or the high proximal origin of pronator teres. Such cases may present with discomfort, fatigue and paresthesia in distribution of median nerve [4]. Thus, cognizance of accessory muscle mass and its relation to median nerve is vital for understanding of entrapment neuropathies. Here, we presented a distinctive case of accessory humeral head of pronator teres in left limb of a male cadaver.
Gupta and Ray described a third head of pronator teres in the left limb associated with the third head of biceps brachii in right limb of the same cadaver. The third head of pronator teres took origin from medial intermuscular septum and fused with the ulnar head of pronator teres at insertion. This additional head overlapped median nerve and brachial artery [5]. In the present case, the accessory pronator teres muscle joined with the humeral head of pronator teres after covering brachial artery and median nerve. The existence of such variations should be considered in the cases of high median nerve palsy with features of brachial artery or vein compression [5]. In another analogous instance of accessory muscle overlying neurovascular structures at elbow, Nayak et al., observed a supernumerary muscle joining the humeral head of pronator teres, concomitant with two extra heads of biceps brachii in the right limb of a cadaver. The presence of accessory muscles is one of the predisposing factors for the high median nerve entrapment neuropathy [6]. This supernumerary muscle took origin from the shaft of humerus unlike the accessory muscle in our case which has extensive soft tissue origin.
As per a case presented by Kumar et al., third head of pronator teres was seen with high division of brachial artery in the right limb. The third head was attached to the fascia covering brachialis, enclosed the ulnar artery and joined with the humeral head [7]. Ahmad et al., reported a case of additional head of pronator teres in right limb, taking origin from flexor carpi radialis and uniting with tendon of pronator teres, with median nerve crossing between ulnar and humeral heads. Also, it was suggested that such unusual muscle mass can compress median nerve and would also affect surgical procedures by mimicking soft tissue tumours [8].
Pronator teres syndrome presents with numbness along the course of median nerve with muscle weakening. If limb is repeatedly pronated, it can bring forth or worsen the symptoms, suggesting nerve constraint at pronator teres. The surgical exploration in these instances has revealed an increased muscle mass or a tendinous band in muscle, or an anomalous muscle. Such median nerve compression in elbow makes the nerve more susceptible to compression in the carpal tunnel and improvement may occur after relief of proximal nerve compression [4]. Thus, the accessory muscle bundles like that of our case by overlapping the median nerve, is likely to impede the nerve function and make it more liable to develop entrapment neuropathies at distal locations.
In fetal life, myogenic cells from somites enter the limb bud to form muscles. The process of muscle morphogenesis is directed by the connective tissue of the developing limb. The myogenic cells in limb initially form flexor and extensor muscle masses. The final form of muscles is dependent on factors like the splitting of muscle masses, the T-box transcription factors controlling muscle pattern, and changes in muscle primordia. The secretion of PDGF (Platelet Derived Growth Factor) by the surrounding blood vessels plays an important role in muscle mass cleavage and the formation of muscle sheaths. The Tbx-5 transcription factor regulates the early limb bud formation and also the limb muscle patterning in later stages. In some muscles, the muscle primordia undergo programmed cell death so as to cause disappearance of a muscle layer. So, the change in pattern of blood vessels, or mutations of T-box genes, or defective apoptosis in muscle primordia can cause abnormal muscle development in limbs [9].
Conclusion
The knowledge of arrangement of accessory muscles in arm is significant for diagnosis and treatment of entrapment neuropathies. It is also noteworthy for surgeons to effectually handle operative field and for radiologists to infer scans.
[1]. Biant LC, Elbow and forearm. In: Standring S, editorGray’s anatomy: The anatomical basis of clinical practice 2016 41st editionElsevier:848-58. [Google Scholar]
[2]. Bilecenoglu B, Uz A, Karalezli N, Possible anatomic structures causing entrapment neuropathies of the median nerve; An anatomic studyActaOrthop Belg 2005 71:169-76. [Google Scholar]
[3]. Nebot-Cegarra J, Reina-de la Torre F, Perez-Berruezo J, Accessory fasciculi of the human pronator teres muscle: incidence, morphological characteristics and relation to the median nerveAnn Anat 1994 176(3):223-27. [Google Scholar]
[4]. Hartz CR, Linscheid RL, Gramse RR, Daube JR, The pronator teres syndrome: Compressive neuropathy of median nerveThe Journal of Bone and Joint Surgery 1981 63-A(6):885-90. [Google Scholar]
[5]. Gupta R, Ray SB, Anomalous third head of biceps brachii and pronator teres in single cadaverJIMSA 2013 26(4):224-25. [Google Scholar]
[6]. Nayak SR, Krishnamurthy A, Prabhu LV, Jiji PJ, Ramanathan L, Kumar S, Multiple supernumerary muscles of the arm and its clinical significanceBratisl Lek Listy 2008 109(2):74-75. [Google Scholar]
[7]. Kumar N, Rao SS, Aithal A, Nayak SB, Possible entrapment of the ulnar artery by the third head of pronator teres muscleRev Arg de Anat Clin 2012 4(3):102-05. [Google Scholar]
[8]. Ahmad T, Khan AQ, Sultana A, Variation in the origin of pronator teresJournal of Medical Erudite 2014 2(2):13-17. [Google Scholar]
[9]. Carlson BM, Human embryology and developmental biology 2013 5th editionPhiladelphiaElsevier Health Sciences:206-08. [Google Scholar]