Paediatric Prescription Analysis in a Primary Health Care Institution
Jinish Jose1, Denny Devassykutty2
1 Assistant Professor, Department of Pharmacology, Government Medical College, Kottayam, Kerala, India.
2 Associate Professor, Department of Pharmacology, Believers Church Medical College, Thiruvalla, Kerala, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jinish Jose, Assistant Professor, Department of Pharmacology, Government Medical College, Kottayam-686008, Kerala, India.
E-mail: drjinishjose@gmail.com
Introduction
Paediatric prescription analysis was done by vari-ous studies in tertiary care centers but not much published data, at primary care level. The Medical Council of India introduced new prescription format and also antibiotic stewardship program was launched by Government of Kerala in the year 2015. So in these contexts this study was conducted.
Aim
To analyse the patterns of prescriptions and drug dis-pensing in pediatric patients using WHO core drug use indicators and parameters in the prescription format prescribed by Medical Council of India.
Materials and Methods
Prospective study was done at a community health center, for a period of four months where parents of children attending the outpatient department were interviewed and the prescriptions and medicines that is with them was examined and analysed for any prescription errors or dispensing errors. For statistical analysis, quantitative variables were expressed in mean and standard deviation and qualitative variables in percentages.
Results
The mean age of the patients was 6.1 (SD±3.4) years. The average number of drugs prescribed was 2.29 (SD±35.91), 98.4% drugs were prescribed by generic name. Majority of drugs prescribed were in the form of syrups (62.73%), use of antibiotics was frequent (73.18%), but injection use was very minimal (0.006%). Weight of the patient was recorded in 58.33% of the prescriptions. Only 30 prescriptions (5.43%) were written in capital letters. A 100% of the prescriptions contain the details of the child along with provisional diagnosis and signature of the doctor. A 98.44% of the drugs prescribed were from the essential drug list. Copy of the essential drug list is available at the institution. The availability of key drugs was 100%. 98.73% knew the correct dosages and 100% of the drugs were adequately labeled.
Conclusion
The prescription pattern is in accordance with the standard guidelines of WHO. Interventions are needed to rectify over prescription of antibiotics to strengthen antibiotic stewardship program so that emergence of drug resistant strains can be avoided.
Antibiotic stewardship, Core drug use indicators, Prescription pattern
Introduction
Prescription analysis is a very good tool to analyse the prevailing disease pattern and drug use in a community. Irrational prescription leads to ineffective and unsafe treatment, exacerbation or prolongation of illness, distress and harm to the patient along with higher costs [1]. It may be due to factors such as patient pressure, bad example of colleagues and high powered salesmanship. Prescription analysis helps in promoting rational use of drugs in which right drug is prescribed for right condition in right dose and duration and gives information about any dispensing errors [2]. It helps in antibiotic stewardship program which is the core in preventing antibiotic resistance. It also helps in cost benefit analysis on drugs and to make policy on drugs by the policy makers. Essential drugs offer a cost-effective solution to health problems [3]. Prescribers can treat patients in a rational way if they have access to essential drugs on a regular basis [3]. Paediatric prescription is more complicated than adults because prescription is according to weight and some drugs are contraindicated in paediatric age groups. Although paediatric prescription pattern studies were done in various tertiary care centers [4–6] limited studies were carried out in paediatric patients in primary health care institutions [7]. So, it is desirable to do a study at this primary care level.
Materials and Methods
The study was conducted as a prospective study at a community health centre in Kerala, India, after obtaining ethical clearance. The duration of the study was four months with a sample size of 552. The community health centre primarily serves the population in a panchayat. There is no other clinic or hospital there. The daily number of patients attending the outpatient department is between 150 to 200 and of these paediatric patients constitute around 40 to 50 cases per day. In the outpatient department, children of all ages can avail medical consultation at a very nominal cost of Rupees 2/OP ticket and drugs are dispensed free of cost. In the outpatient department, children were seen by doctors in one consultation room. There is token system and the parents can take token on coming to the hospital and they will be called-on when their turn comes. There is no separate queue for paediatric cases. There is a waiting area with lots of chairs. There is a television and water purifier in the waiting area. So, the parents don’t have to stand with the children to see the doctor. The hospital pharmacy counter situated on the nearby room where patients will get the medicines from the pharmacist. The children within the age group of 28 days to 12 years were included in the study. Written informed consent was obtained in the mother tongue from the parents or guardian accompanying the children. Those who came for vaccination and those not willing to give consent were excluded from the study. The “core drug use indicators” formulated by World Health Organization (WHO) and the parameters in the prescription format prescribed by the Medical Council of India forms the basis of the study [Table/Fig-1] [2,8]. This is done outside the institution when the parents and children came out of the hospital so that the doctors inside were not aware of the study and the bias of writing the prescription due to monitoring by the investigator can be avoided. For the same reason, two parameters in the patient care indicators like average consultation time and average dispensing time are not measured in this study. Other patient care indicators like percentage of medicines actually dispensed, whether it is adequately labelled, and the parent’s knowledge of when and in what quantity each drug that the child should receive were analysed. Finally, facility indicators were analysed at the end of the study by looking at the facilities in the institution and enquiring about the availability of essential drug list in the institution, the availability of clinical guidelines and the percentage of key drugs available in the institution. The major parameters analysed in the prescription format prescribed by the Medical Council of India includes the patient details, weight of the patient, whether prescription written in capital letters, signature of the doctor and the pharmacist. The essential drug list prepared by the Kerala Medical Service Corporation Limited (KMSCL) is used in the study [9].
Core drug use indicators by WHO.
| Prescribing Indicators:
Average number of medicines prescribed per patient encounter
% medicines prescribed by generic name
% encounters with an antibiotic prescribed
% encounters with an injection prescribed
% medicines prescribed from essential medicines list or formularyPatient Care Indicators:
Average consultation time
Average dispensing time
% medicines actually dispensed
% medicines adequately labelled
% patients with knowledge of correct dosesFacility Indicators:
Availability of essential medicines list or formulary to practitioners
Availability of clinical guidelines
% key medicines availableComplementary Drug Use Indicators:
Average medicine cost per encounter
% prescriptions in accordance with clinical guidelines |
Results
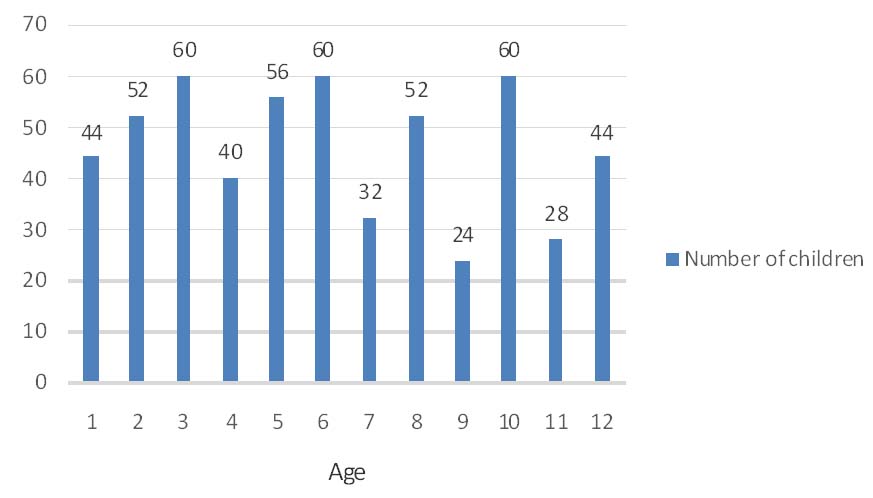
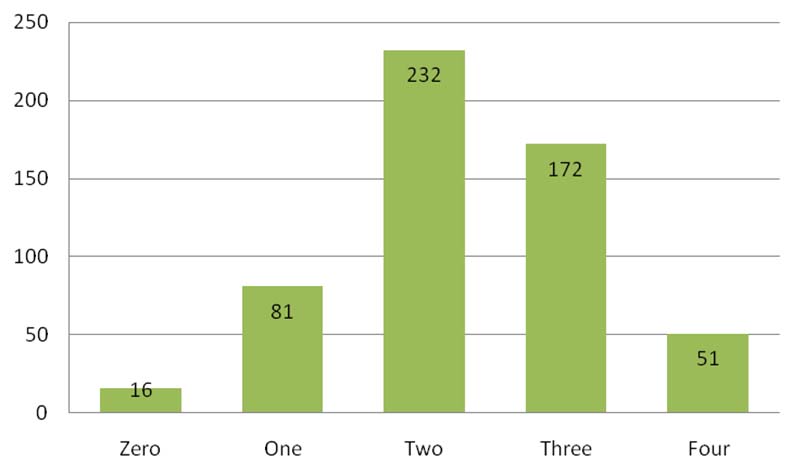
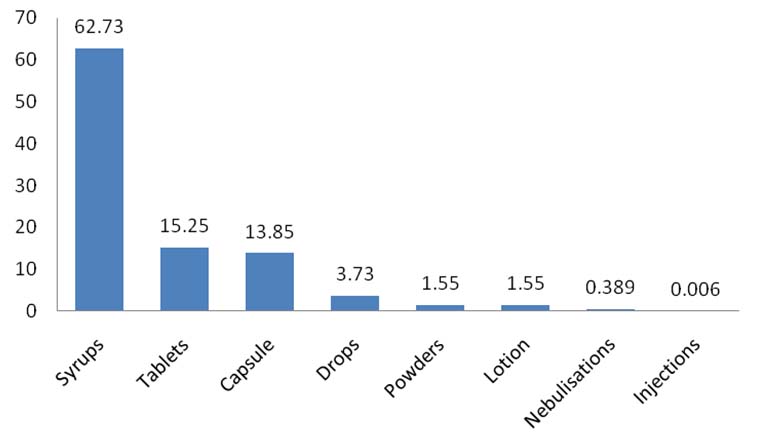
A total of 552 patients with ages ranging from 2 months-12 years were enrolled during the study period of four months [Table/Fig-2]. The mean age of the patients was 6.1 (SD±3.4) years. Male patients were more 306 (55%) compared to female patients 246 (45%). Weight of the patient was recorded in 58.33% of the prescriptions. All prescriptions under the age of five years were recorded the weight of the child. Only 30 prescriptions (5.43%) were written in capital letters. A 100% of the prescriptions contained the details of the child along with provisional diagnosis. Signature of the prescribing doctor was there in 100% of the prescriptions but none of the prescriptions contains the signature of the dispensing person. A total of 1285 individual drugs were prescribed for various diseases of which upper respiratory infection received maximum number of drugs [Table/Fig-3]. The average number of drugs per prescription was 2.29 (SD±35.91). The range of drugs per encounter varied from zero to 4 [Table/Fig-4]. There were 16 prescription where in no drug was prescribed (2.89%). All these were wounds for which local cleaning and dressing were done. Generic prescribing dominated (98.4%). Only the zinc syrup that was not available in the hospital pharmacy was the only branded prescription. Drugs were prescribed in eight different dosage forms. Syrups were most commonly prescribed (62.73%) and injection use was very less (0.006%) [Table/Fig-5]. Antibiotics were widely used for treatment. The number of encounters with antibiotics was 404 out of the total 552 prescriptions (73.18%). Antibiotics constituted 31.43% of the total number of drugs prescribed. A single antibiotic was prescribed in 404 prescriptions. Antibiotics were prescribed to all children diagnosed with acute upper respiratory infections, lower respiratory tract infections, conjunctivitis and chicken pox. Four children with wounds were also given antibiotics. Among the antibiotics-azithromycin, amoxicillin-clavulanic acid, amoxicillin and cephalexin were prescribed for children with acute tonsillitis. Azithromycin and cefixime were prescribed for children with acute otitis media. Azithromycin, amoxicillin-clavulanic acid was the two antibiotics prescribed for children diagnosed with lower respiratory tract infection. All children diagnosed with acute conjunctivitis were given tobramycin eye drops. Acyclovir was prescribed for children with varicella [Table/Fig-6]. Azithromycin was the most commonly prescribed antibiotic. Every child with acute gastroenteritis was prescribed oral rehydration salts. No anti-diarrheal drugs and antibiotics were prescribed in these children. I.V fluids were given to eight children with acute diarrhoea. Zinc syrup was also prescribed in 20 cases with diarrhoea. A 98.44% (1265/1285) of prescribed drugs were actually dispensed by the hospital pharmacy. All the dispensed drugs were in the same strength as prescribed. On cross checking the dispensed medicines given to the patient, it was seen that no patient received a wrong drug or an incorrect dosage. A 100% of the drugs were adequately labelled. A 98.73% (545/552) of parents knew the correct dosage schedule for all the drugs prescribed. Regarding facility indicators the hospital has all the facilities for outpatient care. Three doctors are working at the institution so at a time at least one doctor will be available for patient care even if one or two will be on leave or went for immunization at sub centres/conference/training. There is lab facility at the institution with auto analyser and power back up. There is filtered drinking water and waiting area for the patients at the institution. Soft and hard copy of essential drug list prepared by the KMSCL is available at the institution.
Relationship between age and number of children.
Number of children with diseases and number of drugs given for each.
| Disease | Number of children | Total number ofdrugs given |
|---|
| Upper respiratory tract infections | 329 | 824 |
| Lower respiratory tract infections | 40 | 160 |
| Viral fever | 38 | 84 |
| Acute diarrhoeal diseases | 32 | 60 |
| Conjunctivitis | 28 | 28 |
| Worm infestation | 28 | 28 |
| Bronchial asthma | 20 | 35 |
| Wounds | 22 | 10 |
| Pityriasis alba | 12 | 24 |
| Varicella | 3 | 12 |
Range of drugs per prescription.
Various dosage forms and their percentage.
Key drugs prescribed for the respective diseases.
| Disease | Key drugs prescribed |
|---|
| Upper respiratory tract infections | Azithromycin, Amoxicillin, Cephalexin, Cefixime |
| Amoxicillin clavulanic acid, Paracetamol, Cetrizine |
| Lower respiratory tract infections | Azithromycin, Amoxicillin clavulanic acid, |
| Salbutamol, Paracetamol |
| Viral fever | Paracetamol, Saline nasal drops, Cetrizine |
| Acute diarrhoeal diseases | ORS, Zinc, IV fluids, Domperidone |
| Conjunctivitis | Tobramycin |
| Worm infestation | Albendazole |
| Bronchial asthma | Salbutamol, Cetrizine |
| Wounds | Local dressing, Multi vitamin |
| Pityriasis alba | Multi vitamin, Hydrocortisone ointment |
| Varicella | Acyclovir, Cetrizine, Paracetamol, Calamine lotion |
Discussion
The core prescribing indicators measure the performance of prescribers, the patient care indicators measure what patients experience at health facilities and the facility indicators measure whether the health personnel can function smoothly and effectively. Prescribing indicators were analysed by scrutinizing the prescriptions written by the doctors in the institution. The average number of drugs per patient is 2.29 is close to 2.0, the value recommended by the WHO [2] and is less than previous studies [4,7,10]. Maximum number of drugs per prescription is four and range of drugs per prescription is from 0-4 and is less than other similar studies [4,7]. The number of drugs per prescription should be as low as possible because as the number of drugs increases the chances of drug interactions and adverse effects will also increase along with increase in hospital cost. The mean age of patients is 6.1 years and is more than similar studies done previously [4]. So, this shows that breast feeding is adequate in the children offering protection in the toddler age. A 98.4% of the drugs are prescribed in generic name and is more than other studies [4,7,11–13]. The reason for this is due to availability of these key drugs in the hospital itself, which is given free of cost. The number of prescriptions with antibiotic is 73.18% of the total prescriptions and is much higher than one study [6] but slightly less than another study [7]. All diseases diagnosed with upper respiratory infection were given antibiotic and this should be of concern since most of the upper respiratory infections were of viral origin for which antibacterial agents have no role [14,15]. The over prescription of antibiotics is a hindrance in preventing drug resistance which the core objective of antibiotic stewardship program. So why the doctors overprescribed antibiotics needs to be investigated and interventions are needed in this regard. No antibiotics were prescribed for acute diarrheal diseases which is a positive finding in this study compared to other studies [4,16,17]. The usage of injections were also very less in the present study compared to other studies [4]. All the drugs dispensed were in the essential drug list and were available in the hospital and in correct doses. A 100% of the drugs were adequately labelled and is higher than the previous studies [18,19]. Body weight of the patient was recorded only in 58.33% of the patients which needs to be improved. But body weight was recorded for all the patients under the age of five years which is more important. Capital letters were not used in writing majority of the prescriptions and the signature of the dispensing person was not there in none of the prescriptions. So, interventions in the form of awareness training are needed in these issues. There should be adequate facilities for storing the drugs under proper temperatures as in summer season temperature may comes to 40oC which may result in the loss of efficacy of drugs.
Limitation
As the study is conducted in patients attending a government hospital the availability of drugs in the institution may influence prescribing patterns. Also, we cannot generalise the same prescribing pattern in all the primary care centres as more study at different institutions needs to be conducted to accurately know the prescribing patterns.
Conclusion
The present study showed that rational prescription can be achieved in primary care level if policy makers take steps to make essential drugs and qualified staff available. Interventions aimed at improving knowledge and training to staff in the issue of over prescription of antibiotics and in following a uniform prescription pattern designed by regulatory authorities is highly advisable. Further studies like this are recommended after imparting such training to healthcare staff.
[1]. Aronson JK, Medication errors: what they are, how they happen, and how to avoid themQJM 2009 102(8):513-21. [Google Scholar]
[2]. Van den Bemt PMLA, Egberts ACG, Drug related problems, definitions and classificationEur J Hosp Pharm Pract 2007 13:62-64. [Google Scholar]
[3]. International network for rational use of drugs and World Health Organization. How to investigate drug use in health facilities: Selected drug use indicators. EDM research series No.7 [WHO/ DAP/ 93.1]. Geneva:World Health Organization 1993 [Google Scholar]
[4]. Karande S, Sankhe P, Kulkarni M, Patterns of prescription and drug dispensingThe Indian Journal of Pediatrics 2005 72:117-21. [Google Scholar]
[5]. Cole CP, James PB, Kargbo AT, An evaluation of the prescribing patterns for under-five patients at a tertiary paediatric hospital in Sierra LeoneJournal of Basic and Clinical Pharmacy 2015 6(4):109-14. [Google Scholar]
[6]. Fadare J, Olatunya O, Oluwayemi O, Ogundare O, Drug prescribing pattern for under-fives in a paediatric clinic in south-western NigeriaEthiopian Journal of Health Sciences 2015 25(1):73-78. [Google Scholar]
[7]. Pandey AA, Thakre SB, Bhatkule PR, Prescription analysis of pediatric outpatient practice in Nagpur cityIndian Journal of Community Medicine 2010 35(1):70-73. [Google Scholar]
[8]. Medical Council of India-211(2) (Gen)/2014-Ethics/155202. Dated 30/01/2015 (Accessed 17th December 2015) [Google Scholar]
[9]. http://www.kmscl.kerala.gov.in/ essential drugs [Accessed 20th July 2015] [Google Scholar]
[10]. Ghaleb MA, Wrong IC, Medication errors in paediatric patientsArch Dis Child Educ Pract 2006 91:20 [Google Scholar]
[11]. Nwolisa CE, Erinaugha EU, Ofoleta SI, Prescribing practices of doctors attending to under fives in a children’s outpatient clinic in Owerri, NigeriaJ Trop Pediatr 2006 52(3):197-200. [Google Scholar]
[12]. Ahmed AM, Awad AI, Drug use practices at pediatric hospitals of Khartoum state, SudanAnn Pharmacother 2010 44(12):1986-93. [Google Scholar]
[13]. Bosu WK, Ofori-Adjei D, An audit of prescribing practices in health care facilities of the Wassa West district of GhanaWest Afr J Med 2000 19:298-303. [Google Scholar]
[14]. Bhanwra S, A study of non-prescription usage of antibiotics in the upper respiratory tract infections in the urban populationJournal of Pharmacology & Pharmacotherapeutics 2013 4(1):62-64. [Google Scholar]
[15]. Sadoh WE, Akinsete AM, Physicians management of sore throat in children in Benin city, NigeriaNiger J Clin Pract 2009 12(4):407-11. [Google Scholar]
[16]. Ravi Shankar P, Partha P, Nagesh S, Prescribing patterns in medical outpatientsInt J Clin Pract 2002 56:549-51. [Google Scholar]
[17]. Ekwochi U, Chinawa JM, Obi I, Obu HA, Agwu S, Use and/or misuse of antibiotics in management of diarrhea among children in Enugu, Southeast NigeriaJ Trop Pediatr 2013 59(4):314-16. [Google Scholar]
[18]. Hazra A, Tripathi SK, Alam MS, Prescribing and dispensing activities at the health facilities of a non-governmental organizationNatl Med J India 2000 13:177-82. [Google Scholar]
[19]. Silva MD, Rosa MB, Franklin BD, Reis AM, Anchieta LM, Mota JA, Concomitant prescribing and dispensing errors at a Brazilian hospital: a descriptive studyClinics (Sao Paulo) 2011 66(10):1691-97. [Google Scholar]