Primary Liver Abscess with Anterior Abdominal Wall Extension Caused by Mycobacteriumtuberculosis Complex
Jayashri Sanjay Pandya1, Rahul Vilas Kandekar2, Ajeet Ramamani Tiwari3, Rahul Kadam4, Devbrata Radhikamohan Adhikari5
1 Professor, Head of Unit and Trauma Incharge, Department of General Surgery, Topiwala National Medical College and Bai Yamunabai Laxman Nair Charitable Hospital, Mumbai, Maharashtra, India.
2 Resident, Department of General Surgery, Topiwala National Medical College and Bai Yamunabai Laxman Nair Charitable Hospital, Mumbai, Maharashtra, India.
3 Resident, Department of General Surgery, Topiwala National Medical College and Bai Yamunabai Laxman Nair Charitable Hospital, Mumbai, Maharashtra, India.
4 Resident, Department of General Surgery, Topiwala National Medical College and Bai Yamunabai Laxman Nair Charitable Hospital, Mumbai, Maharashtra, India.
5 Assistant Professor, Department of General Surgery, Topiwala National Medical College and Bai Yamunabai Laxman Nair Charitable Hospital, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ajeet Ramamani Tiwari, Resident, Department of General Surgery, Topiwala National Medical College and Bai Yamunabai Laxman Nair Charitable Hospital, Mumbai, Central-400008, Maharashtra, India.
E-mail: drajeetramantiwari@gmail.com
Tubercular liver abscess is generally secondary to some other primary foci in the body, most notably pulmonary and gastrointestinal system. To find primary tubercular liver abscess is rare, with prevalence of 0.34% in patients with hepatic tuberculosis. Abscess tracking into abdominal wall from spinal and para spinal tuberculosis is known, however primary liver tuberculosis rupturing into anterior abdominal wall has been reported only twice in literature. We report a case of 43-year-old female with direct invasion of the anterior abdominal wall from an isolated tubercular parenchymal liver abscess, caused by Mycobacterium tuberculosis complex, diagnosed primarily on smear for Acid Fast Bacilli (AFB), imaging and isolated by culture and BACTEC MGIT 960 KIT. We discuss here the diagnostic dilemma, management and outcome of primary tubercular liver parenchymal abscess with direct invasion into anterior abdominal wall.
Abdominal wall abscess, Acid fast bacilli, BACTEC MGIT 960, Tubercular liver abscess
Case Report
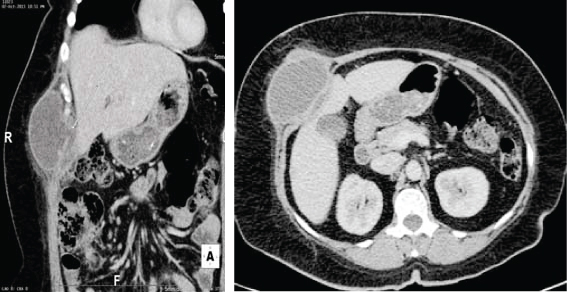
A 43-year-old female, presented with occasional, localized dull aching, non-radiating pain in right hypochondrium, anorexia and intermittent low grade fever of 3 to 4 months duration. No history of weight loss, cough with expectoration, haemoptysis, breathlessness. Patient was well built and averagely nourished. No evidence of generalised lymphadenopathy. On abdominal examination moderate hepatomegaly was noted. Haematological and biochemical profile was normal. Chest X-ray was normal [Table/Fig-1]. Ultrasonography of abdomen was suggestive of moderate hepatomegaly measuring 17cm and intra parenchymal liver abscess in segment V measuring 10cc (3x2.2x3.7) which appeared to communicate with anterior abdominal wall with collection measuring 140cc (8.7x4.5x6.7) [Table/Fig-2]. CT scan was done to rule out intra-peritoneal rupture. CT scan was suggestive of well defined, unilocular, thick walled enhancing collection in the intra-muscular plane of anterolateral aspect of anterior abdominal wall in right hypochondriac region with peripheral enhancing wall. The liver abscess situated in segment V measuring 10cc (3.7x1.4x2.2) was seen to communicate through a rent measuring 8.9mm posteromedially with the anterior abdominal wall with collection measuring 140cc (8.4x4.5x7.0) [Table/Fig-3,4].

USG of liver abscess before aspiration.

CT scan showing coronal and axial views of primary liver parenchymal abscess communicating with anterior abdominal wall.
USG Guided aspiration of liver abscess was done with a wide bore needle till dry tap was obtained (as shown in [Table/Fig-5]). Seropurulent aspirate was obtained and sent for microbiological investigation [Table/Fig-6]. Pus for Acid Fast Bacilli (AFB) smear showed acid fast bacilli. Aspirate was sent for culture using Lowenstein Jenson medium which showed growth at end of 10 weeks. As aspirate was smear positive, it was cultured using BACTEC MGIT 960 detection kit for early detection which came positive for Mycobacterium tuberculosis complex isolates containing Mycobacteriumtuberculosis, Mycobacteriumbovis and Mycobacterium africanum and Mycobacteriummicroti in 2 weeks. BACTEC MGIT 960 has sensitivity of 62% and specificity of 100%. MGIT 960 has greater sensitivity as compared to culture using Lowenstein Jenson medium [1]. Patient was started on CAT I anti-tubercular drugs under DOTS to which patient responded well.
USG image of liver abscess post aspiration

Seropurulent coloured pus aspirated.

Discussion
Hepatic tuberculosis is one of the rare forms of extra pulmonary tuberculosis. Majority of the tubercular liver abscess are associated with miliary TB or infective foci in the lungs or gastrointestinal tract [2]. Primary liver abscess situated either in the intra-parenchyma or subcapsular location can rupture into anterior abdominal wall. Moreover, till 2003 there was only one case reported of direct invasion of the abdominal wall abscess secondary to extension from sub capsular rupture [3]. Few documented case reports of direct invasion of isolated tubercular parenchymal liver abscess has been reported till 2011 [4,5].
Bestowe., in 1858 first described tubercular liver abscess [6]. Since then, more than 100 case reports and series of hepatic tuberculosis have been reported in various forms. Tubercular liver abscess is generally secondary to some other primary foci in the body, most notably pulmonary and gastrointestinal system. Alvarez et al., Essop et al., and Maharaj et al., reported abnormal chest X-ray in 65%, 75% and 78% respectively [2,7,8] to find primary tubercular liver abscess is rare with prevalence of 0.34% in patients with hepatic tubercular [6]. Complications secondary to tubercular liver abscess like bronchobiliary, gastrobiliary and duodenal fistula have been described. Abscess tracking into abdominal wall from spinal and para spinal tuberculosis is known, however primary liver tuberculosis rupturing into anterior abdominal wall has been reported only twice in literature [4,5].
Katsumi et al., reported a primary tubercular abscess invading the abdominal wall. However, tubercular origin of the abscess could not be confirmed and the diagnosis was based on demonstration of caseous necrosis in histology. Histologically, caseating granuloma in liver biopsy specimen is considered diagnostic of tuberculosis. However, it has occasionally been reported in coccidiodomycosis, Hodgkin’s and brucellosis, but clinical presentation is different [4]. The only confirmed report of primary hepatic tubercular abscess rupturing into anterior abdominal wall came from Gupta et al., in 2011 where PCR aspirate was positive for Mycobacterium tuberculosis however Ziehl-Neelsen (ZN) staining was negative for acid fast bacilli [5]. Our case though initially manifested as routine pyaemic abscess, did not respond to conventional antibiotics and USG guided drainage. Upon further investigations, it came positive for AFB on ZN staining and Mycobacterium tuberculosis Complex by BACTEC MGIT 960 detection kit. Diagnosis of Mycobacterium tuberculosis complex by BACTEC MGIT 960 was made patient was started on anti Koch’s treatment. Patient completed 6 months of anti-tuberculosis treatment and is asymptomatic at present.
Various authors have tried to classify liver tuberculosis, foremost being Kansal et al., Reed et al., and Levine et al., [9–11]. Precise diagnosis of tubercular abscess even in high prevalence country like India, where tuberculosis is an alarming public health problem, is delayed owing to conditions like, pyogenic and amoebic liver abscess, which are more prevalent. However, high index of suspicion when unusual presentation and failure to respond to conventional treatment is desirable. It is also observed that tubercular liver abscess is associated with normal white blood cell count, WBC count was 9000/cc unlike amoebic or pyogenic liver abscess which usually present with raised white blood cell counts. Diagnosis of tubercular origin of liver abscess relies on demonstration of AFB on ZN staining or indirect evidence in the form of caseating granuloma on histology. However, ZN staining is positive only in 0-35% cases and liver tissue may not always be available [4].
TB PCR (sensitivity 9-100% and specificity 5-100%) and BACTEC MGIT 960 (sensitivity 62% and specificity 100%) have emerged as highly sensitive diagnostic modality for tuberculosis that can give accurate results in less time [1]. They should be considered in the diagnostic evaluation of liver abscess not responding to conventional treatment. Patients generally respond well to category I anti-tuberculosis treatment; however some authors suggest percutaneous drainage or even instillation of anti-tuberculosis drugs into the abscess cavity [6].
Conclusion
One of the differentials to be considered in liver abscess not responding to treatment is tuberculosis. Proper diagnostic protocol which includes ZN staining, culture, histopathology, PCR and BACTEC MGIT 960 helps in diagnosing and aids in start of appropriate therapy.
[1]. Deshmukh M, Nikam C, Ragte T, Shetty A, Rodrigues C, Is a composite reference standard (CRS) an alternative to culture in assessment and validation of a single tubenested in-house PCR for TB diagnosis?The Egyptian Society of Chest Diseases and Tuberculosis 2013 62(4):805-15. [Google Scholar]
[2]. Alvarez SZ, Hepatobiliary tuberculosisJ Gastroenterol Hepatol 1998 13(8):833-39. [Google Scholar]
[3]. Desai N, Patil S, Thakur BS, Das HS, Manjunath SM, Sawant P, Abdominal wall abscess secondary to subcapsular tubercular liver abscessIndian J Gastroenterol 2003 22(5):190-91. [Google Scholar]
[4]. Abe K, Aizawa T, Maebayashi T, Nakayama H, Sugitani M, Sakaguchi M, Isolated tuberculosis liver abscess invading the abdominal wall report of a caseSurg Today 2011 41(5):741-44. [Google Scholar]
[5]. Gupta G, Nijhawan S, Katiyar P, Mathur A, Primary tubercular liver abscess rupture leading to parietal wall abscess: a rare disease with a rare complicationJ Postgrad Med 2011 57(4):350-52. [Google Scholar]
[6]. Hassani KI, Ousadden A, Ankouz A, Mazaz K, Taleb KA, Isolated liver tuberculosis abscess in a patient without immunodeficiency: A case reportWorld J Hepatol 2010 2(9):354-57. [Google Scholar]
[7]. Essop AR, Segal I, Posen J, Noormohamed N, Tuberculosis abscess of the liver. A case reportS Afr Med J 1983 63(21):825-26. [Google Scholar]
[8]. Maharaj B, Leary WP, Pudifin DJ, A prospective study of hepatic tuberculosis in 41 black patientsQ J Med 1987 63(242):517-22. [Google Scholar]
[9]. Kansal AP, Chopra V, Singh H, Singh U, Tubercular hepatic abscess—a rare PresentationIndian J Tuberc 2008 55(4):217-20. [Google Scholar]
[10]. Levine C, Primary macronodular hepatic tuberculosis: US and CT appearancesGastrointest Radiol 1990 15(4):307-09. [Google Scholar]
[11]. Reed DH, Nash AF, Valabhji P, Radiological diagnosis and management of a solitary tuberculosis hepatic abscessBr J Radiol 1990 63(755):902-04. [Google Scholar]