A Rare Case of An Atypical Solitary Fibrous Tumour of Orbit
Hetal Mahendra Mehta1, Avinash Babarao Ingole2, Anuja Mihir Gharat3, Sujit Mardansingh Murade4, Anjali Darius Nicholson5
1 Speciality Medical Officer, Department of Ophthalmology, BMC Eye Hospital, Mumbai, Maharashtra, India.
2 Additional Professor, Department of Ophthalmology, B.Y.L. Nair Ch. Hopsital, Mumbai, Maharashtra, India.
3 Lecturer Adhoc, Department of Ophthalmology, B.Y.L. Nair Ch. Hopsital, Mumbai, Maharashtra, India.
4 Assistant Professor, Department of Ophthalmology, B.Y.L. Nair Ch. Hopsital, Mumbai, Maharashtra, India.
5 Professor and Head, Department of Ophthalmology, B.Y.L. Nair Ch. Hopsital, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hetal Mahendra Mehta, C 1/406, Lok Everest CHS. LTD., JSD Road, Mulund West, Mumbai-400080, Maharashtra, India.
E-mail: mail2hetal@gmail.com
Solitary fibrous tumours are of mesenchymal origin and comprise of uncommon spindle cell neoplasias. Most commonly the lesions arise from pleura but other rarer sites include lungs, peritoneum, pericardium, nasal cavities, thyroid, parotid gland and orbit.
We report the case of a 41-year-old male patient who presented to us with a painless, progressive growth of a mass in the superior part of left orbit with proptosis and inferotemporal displacement of the left eye. Computed Tomography (CT) scan revealed homogeneous enhancing lesion in the superior compartment of left orbit in the extraconal region, extending intraconally and distorting the globe. Upon imaging, the differential diagnosis were lacrimal gland tumour, atypical cavernous haemangioma and nerve sheath tumour. Surgical treatment included complete excision of the mass with the intraoperative finding of mass extending upto the superior oblique tendon, a part of which was excised. Histopathological examination revealed CD34 positive, Bcl-2 and MIC-2 positive tumour with the diagnosis of a solitary fibrous tumour with atypical features but no malignant features. After a follow-up of 18 months, no recurrence was detected.
Immunohistochemistry, Orbit, Spindle cell neoplasias
Case Report
A 41-year-old male patient presented to our outpatient department complaining of slowly progressive painless proptosis along with inferotemporal displacement of the left eye since two years [Table/Fig-1]. He also complained of gradual loss of vision over last two months. His best-corrected visual acuity in the left eye was finger counting 1 meter. On ophthalmological assessment, the left eye fundus showed disc oedema with choroidal folds over the entire posterior pole. His extraocular movements in the left eye showed loss of elevation with limited adduction, abduction and depression. On palpation, a firm, non-tender, non-pulsatile mass with well-defined superior margin could be felt in the superior aspect of the left orbit. The left eye was displaced inferotemporally and showed blepharoptosis due to mass effect. The visual acuity in the right eye was 6/6, N6 with a standard ophthalmological assessment.
Clinical photograph of the patient on presentation, showing marked proptosis and inferotemporal displacement of left eye.

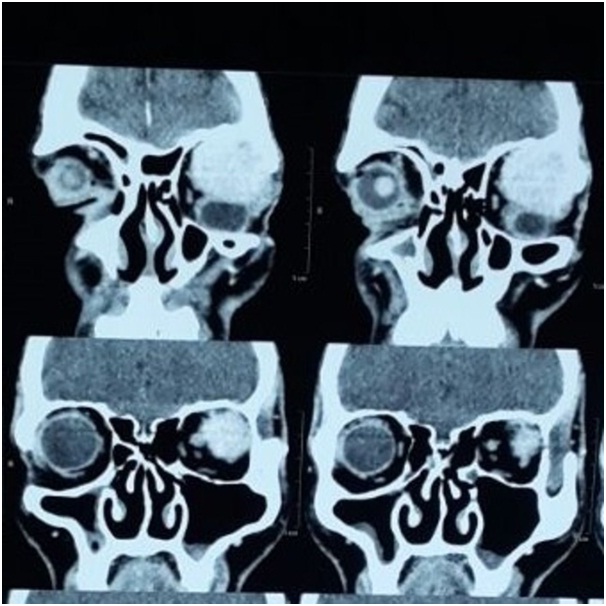
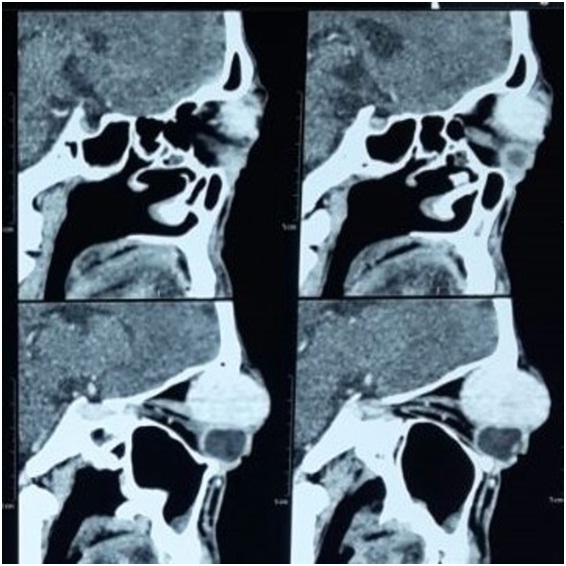
Computed tomography of the left orbit showed a 4.3x3.7x2.8cm sized homogeneous enhancing hyperdense lesion in the superior compartment of the left orbit originating in the extraconal compartment and extending intraconally, causing marked proptosis. The mass was seen distorting the globe and causing scleral buckling, most marked superolaterally [Table/Fig-2,3 and 4]. The fat planes with the optic nerve, sclera, lateral rectus, superior rectus, inferior oblique muscle were focally lost. It showed thinning but no erosion of roof of the left orbit. The differential diagnosis given upon imaging was: lacrimal gland tumour, nerve sheath tumour or atypical cavernous haemangioma.
Axial view of contrast computed tomography scan showing marked proptosis of left eye.
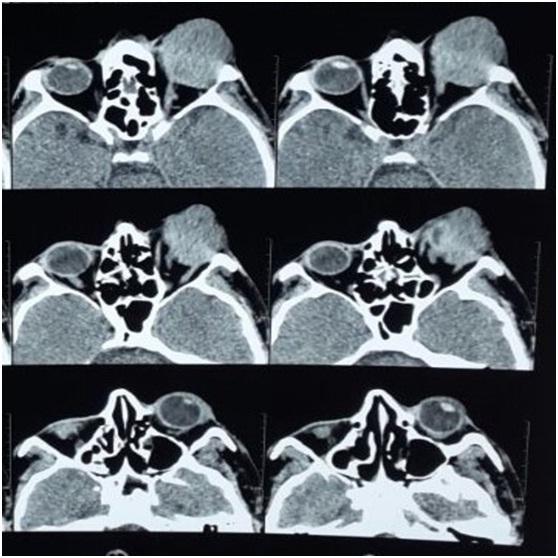
Coronal view of contrast computed tomography scan showing homogenously enhancing lesion causing inferotemporal displacement of globe with marked distortion of globe.
Sagittal view of contrast computed tomography scan showing homogenous enhancing lesion in extraconal compartment extending intraconally and distorting the globe.
The patient underwent left fronto-orbital orbitotomy with unroofing of the orbit. The mass was encapsulated with multiple lobulations on the surface. The mass was not adherent to the surrounding orbital soft tissues, but was noted to be extending upto around one-third of the superior oblique tendon near the insertion of the muscle. Thus, a part of the superior oblique tendon was also excised along with complete mass [Table/Fig-5]. This was followed by orbital roof plating and the case was surgically closed.
The gross specimen of the tumour mass excised.

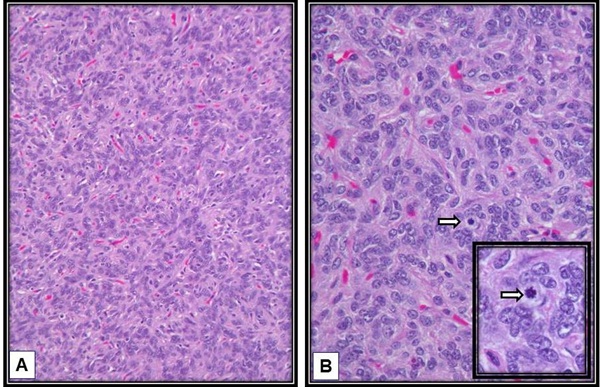
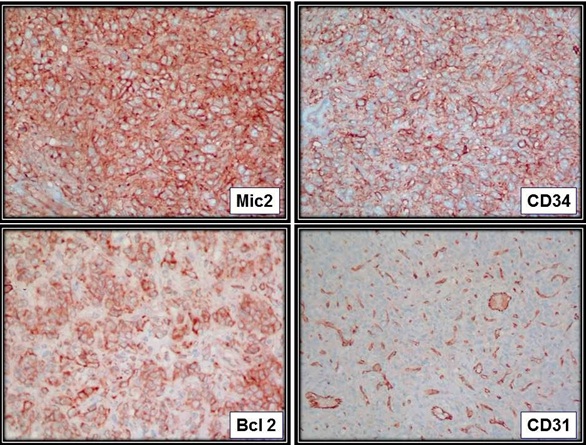
Histopathological examination revealed a lesion composed of oval to spindle shaped cells with focal haemangiopericytoma like vasculature [Table/Fig-6]. Tumour cells showed patternless arrangement. Extracellular collagen deposition was seen focally. Few cells showed intranuclear inclusion body. Few multinucleate giant cells were also observed. Necrosis was not seen. Mitosis was 3-4 /10 High Power Fields (HPF) in highest proliferating areas. On immunohistochemistry, the tumour cells showed CD34, Bcl-2 and MIC-2 positivity. It was seen to be negative for CD31, EMA and PR [Table/Fig-7]. The tumour was concluded to be a solitary fibrous tumour with atypical features. However, it did not show any malignant features.
Histopathology. Slide A shows oval to spindle shaped cells with focal haemangiopericytomatous vasculature. The tumour cells show patternless arrangement (H&E stain,100X). Slide B shows a mitotic figure (arrow) in highest proliferating area; inset shows magnified view of the mitotic figure. (H&E stain,400X).
Immunohistochemistry. Top left slide shows positivity for MIC-2; Top right slide shows strong positivity for CD34; Down left slide shows positivity for Bcl-2 stain; Downright slide shows negativity to CD31.
On 18 months of follow-up, there were no signs of recurrence [Table/Fig-8]. The patient showed signs of improved extraocular movements but had ptosis in the left eye. The patient was planned for cosmetic Strabismus and ptosis surgery.
Clinical photograph of the patient taken at 18 months follow-up showing no evidence of any mass on external examination but ptosis is seen.

Discussion
An orbital solitary fibrous tumour was first reported by Westra et al., in 1994 [1]. Since then only about 61 cases are reported.
Orbital solitary fibrous tumours commonly occur in superior aspect of the orbit. They are found among the middle-age individuals leading to a gradual unilateral progressive proptosis. Atypical presentations include visual disturbance, ocular motility restriction and blepharoptosis [2–4]. Our patient presented with all of the above atypical complaints. Tumour invasion into adjacent bone or soft tissue is also uncharacteristic of this tumour [5]. In fact, recurrent tumours have been reported to involve surrounding orbital tissues as well as paranasal sinuses and intracraniaI space [6]. In our case, the tumour mass was seen adherent to a part of the superior oblique tendon.
The histopathologic morphology of solitary fibrous tumours is similar to haemangiopericytomas, giant cell angiofibromas and fibrous histiocytomas. Some authors view haemangiopericytoma and solitary fibrous tumours as ends of a continuum rather than two lesions with distinctly defined histopathology [7]. However, advances in immunohistochemistry have facilitated a clear distinction amongst these entities.
Various imaging modalities like Ultrasonography, Computed Tomography (CT), Magnetic Resonance Imaging (MRI) have been used to describe solitary fibrous tumours but there are no specific imaging diagnostic features. A well circumscribed mild to moderate enhancing lesion as seen in our case, is a typical CT finding of solitary fibrous tumours [8].
Histopathologically, a “patternless” growth pattern, wherein spindle cells are randomly arranged, is a characteristic feature of solitary fibrous tumour. Cells are often densely arranged with numerous vascular channels that may form a branching or stag-horn like channels, similar to haemangiomapericytoma. These features were consistent with our findings. The degree of collagen can vary from little to extensive keloid-like fibrosis. Histologic features that are suggestive of malignant potential are nuclear atypia, increased cellularity, necrosis and greater than 4 mitoses/10 HPF [9].
Immunohistochemical studies have shown that solitary fibrous tumours have strong and diffuse positivity to CD34, vimentin and Bcl-2. In one of the largest studies by Furusato et al., (n=41), CD34 positivity was seen in all cases, CD99 in 67.5% and Bcl-2 in 47.5% of the cases [10]. Solitary fibrous tumours show non-specific reactivity to CD99 and negativity to desmin, reticulin, cytokeratin, factor VIII related antigen, S-100, SMA and muscle specific actin [1,11]. In contrast to solitary fibrous tumours, haemangiopericytomas show inconsistent and weak positivity to CD34. It is important to differentiate haemangiopericytoma from solitary fibrous tumours because haemangiopericytoma has aggressive behaviour with 83% recurrence rate, 27% distant metastasis and 22% mortality rate, as against the usually benign nature of solitary fibrous tumour [12].
Smooth muscle tumours show positivity to desmin and actin and negativity to Bcl-2 and CD 34. Neural tumours show focal positivity to Bcl-2 and CD34 and strong positivity to S-100 protein.
The mainstay of treatment of orbital solitary fibrous tumours is complete surgical resection with long-term follow-up [4]. But, sometimes complete tumour removal may not be possible and close follow-up may be necessary along with possible further surgery. There is no conclusive evidence supporting any benefit of adjunctive radiotherapy or chemotherapy [3,4,13,14]. Recurrences as late as five years have been reported in case of solitary fibrous tumours. Solitary fibrous tumours are mostly benign in nature but local invasion, recurrence and distant metastasis have been reported in pleural solitary fibrous tumours [9]. Therefore, long-term follow-up is ideal in these cases.
Conclusion
Our case was a solitary fibrous tumour of orbit with atypical clinical presentation as well as atypical histologic features. Thus, although uncommon, solitary fibrous tumours should be considered in the differential diagnosis of a palpable mass with proptosis, blepharoptosis, ocular motility restriction or even visual disturbance. Also, it should be regarded as a possible diagnosis along with other spindle cell tumours and other commoner orbital tumours. Immunohistochemistry plays a significant role in differentiating orbital solitary fibrous tumour from other spindle-cell tumours of the orbit. These cases should be subjected to close long-term follow-up to detect any recurrence.
[1]. Westra W, Gerald W, Rosai J, Solitary fibrous tumour consistent CD34 immunoreactivity and occurrence in the orbitAm J Surg Pathol 1994 18(10):992-98. [Google Scholar]
[2]. Krishnakumar S, Subramanian N, Mohan E, Mahesh L, Biswas J, Rao N, Solitary fibrous tumour of the orbit: a clinicopathologic study of six cases with review of the literatureSurv Ophthalmol 2003 48(5):544-54. [Google Scholar]
[3]. Tam E, Chen E, Nijhawan N, Harvey J, Howarth D, Oestreicher J, Solitary fibrous tumour of the orbit: A case seriesOrbit 2008 27(6):426-31. [Google Scholar]
[4]. Dorfman D, To K, Dickersin G, Rosenberg A, Pilch B, Solitary fibrous tumour of the orbitAm J Surg Pathol 1994 18(3):281-87. [Google Scholar]
[5]. Gupta S, Verma R, Sen R, Singh I, Marwah N, Kohli R, Solitary fibrous tumour of the orbitAsian J Neurosurg 2016 11(1):78 [Google Scholar]
[6]. Bernardini FP, de Conciliis C, Schneider S, Kersten RC, Kulwin DR, Solitary fibrous tumour of the orbit: is it rare? Report of a case series and review of the literatureOphthalmology 2003 110(7):1442-48. [Google Scholar]
[7]. Goldsmith J, van de Rijn M, Syed N, Orbital haemangiopericytoma and solitary fibrous tumour: A morphologic continuumInt J Surg Pathol 2001 9(4):295-302. [Google Scholar]
[8]. Ali MJ, Honavar SG, Naik MN, Vemuganti GK, Orbital solitary fibrous tumour: A rare clinicopathologic correlation and review of literatureJ Res Med Sci 2013 18(6):529 [Google Scholar]
[9]. Vallat-Decouvelaere A, Dry S, Fletcher C, Atypical and malignant solitary fibrous tumours in extrathoracic locationsAm J Surg Pathol 1998 22(12):1501-11. [Google Scholar]
[10]. Furusato E, Valenzuela I, Fanburg-Smith J, Auerbach A, Furusato B, Cameron J, Orbital solitary fibrous tumour: encompassing terminology for haemangiopericytoma, giant cell angiofibroma, and fibrous histiocytoma of the orbit: reappraisal of 41 casesHum Pathol 2011 42(1):120-28. [Google Scholar]
[11]. Suster S, Fisher C, Moran C, Expression of bcl-2 oncoprotein in benign and malignant spindle cell tumours of soft tissue, skin, serosal surfaces, and gastrointestinal tractAm J Surg Pathol 1998 22(7):863-72. [Google Scholar]
[12]. Tihan T, Viglione M, Rosenblum MK, Olivi A, Burger PC, Solitary fibrous tumours in the central nervous system: a clinicopathologic review of 18 cases and comparison to meningeal haemangiopericytomasArch Pathol Lab Med 2003 127(4):432-39. [Google Scholar]
[13]. Polito E, Tosi G, Toti P, Schürfeld K, Caporossi A, Orbital solitary fibrous tumour with aggressive behaviorGraefe’s Arch Clin Exp Ophthalmol 2002 240(7):570-74. [Google Scholar]
[14]. Young TK, Hardy TG, Solitary fibrous tumour of the orbit with intracranial involvementOphthal Plast Reconstr Surg 2011 27(3):e74-76. [Google Scholar]