Asymptomatic Traumatic Hepatothorax, Symptomatic Gall Stone Disease – A Rare Coincidence
Somak Das1, Dinesh Zirpe2, Chandrasekharn Valiathan Gopakumar3, Sudeepta Kumar Swain4, Rajagopal Surendran5
1 Residential Medical Officer, Surgical Gastroenterology, School of Digestive & Liver Diseases, Institute of Post Graduate Medical Education & Research, Kolkata, West Bengal, India.
2 DNB Registrar, Surgical Gastroenterology, Apollo Hospital, Chennai, Tamil Nadu, India.
3 DNB Registrar, Surgical Gastroenterology, Apollo Hospital, Chennai, Tamil Nadu, India.
4 Consultant, Surgical Gastroenterology, Apollo Hospital, Chennai, Tamil Nadu, India.
5 Consultant, Surgical Gastroenterology, Apollo Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Somak Das, 211, East Santoshpur Co-operative Housing Society, Kolkata- 700099, West Bengal, India.
E-mail: d.somak@yahoo.com
Traumatic diaphragmatic hernia rarely affects right side due to protective effect of liver. In adult it is mainly caused by blunt abdominal trauma. Acute presentations are often life threatening and usually clinch the diagnosis early. It may remain asymptomatic for many years unless being detected incidentally during investigations for some unrelated reason or getting complicated by some pathology of herniated viscera. High degree of suspicion is required to detect this delayed presentation particularly in a post-trauma patient as this condition may require modifications in management. We report a case of acute cholecystitis which revealed a rare association of traumatic right diaphragmatic hernia and hepatothorax.
Acute cholecystitis, Blunt trauma abdomen, Right diaphragmatic hernia
Case Report
A 62-year-old male paraplegic patient with 15 years history of diabetes and hypertension presented with intermittent dull aching pain in right lower chest for last 6 months. He suffered pain once in a month or once in two months with occasional radiation to back.
One week back he visited a hospital, because of severe agonising right upper abdominal pain which lasted for around 4 hours and subsided with parenteral analgesics. It was associated with vomiting and one episode of fever of 101°F without any chill or rigor, which subsided with oral antiemetic and paracetamol. The acute episode subsided within 24 hours of onset and he was having mild dull aching pain in right upper abdomen thereafter. He was discharged after 48 hours of admission with oral medications and referred to present hospital according to his preference.
Detailed history revealed that he had a high speed motor vehicle injury 24 years back causing paraplegia due to spinal injury. He was investigated with X-ray of chest and spine as well as ultrasound examination of abdomen. He was diagnosed to have a spinal injury and treated conservatively. From that incident onwards he was bedridden and required intermittent clean catheterisation for emptying urinary bladder.
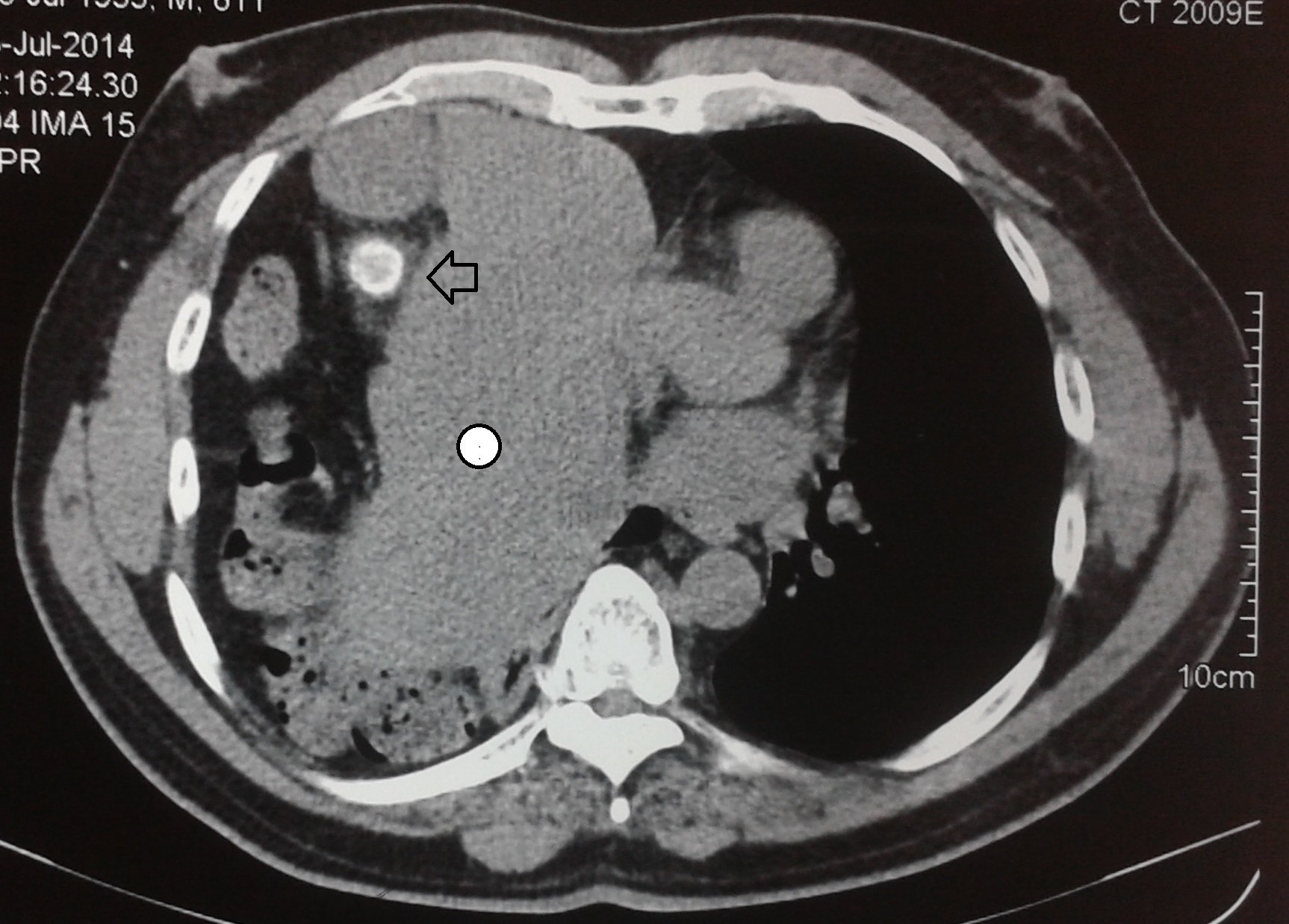
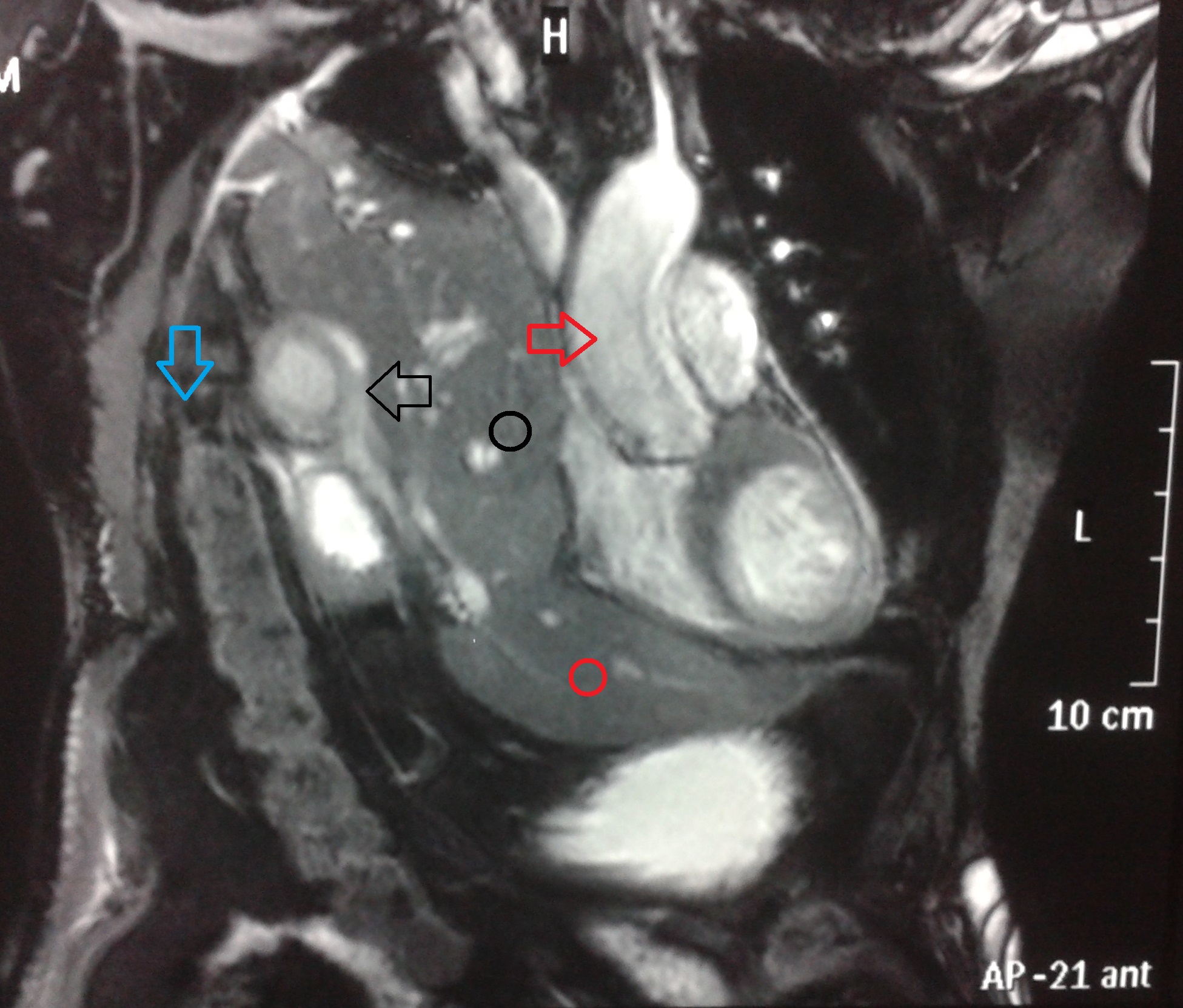
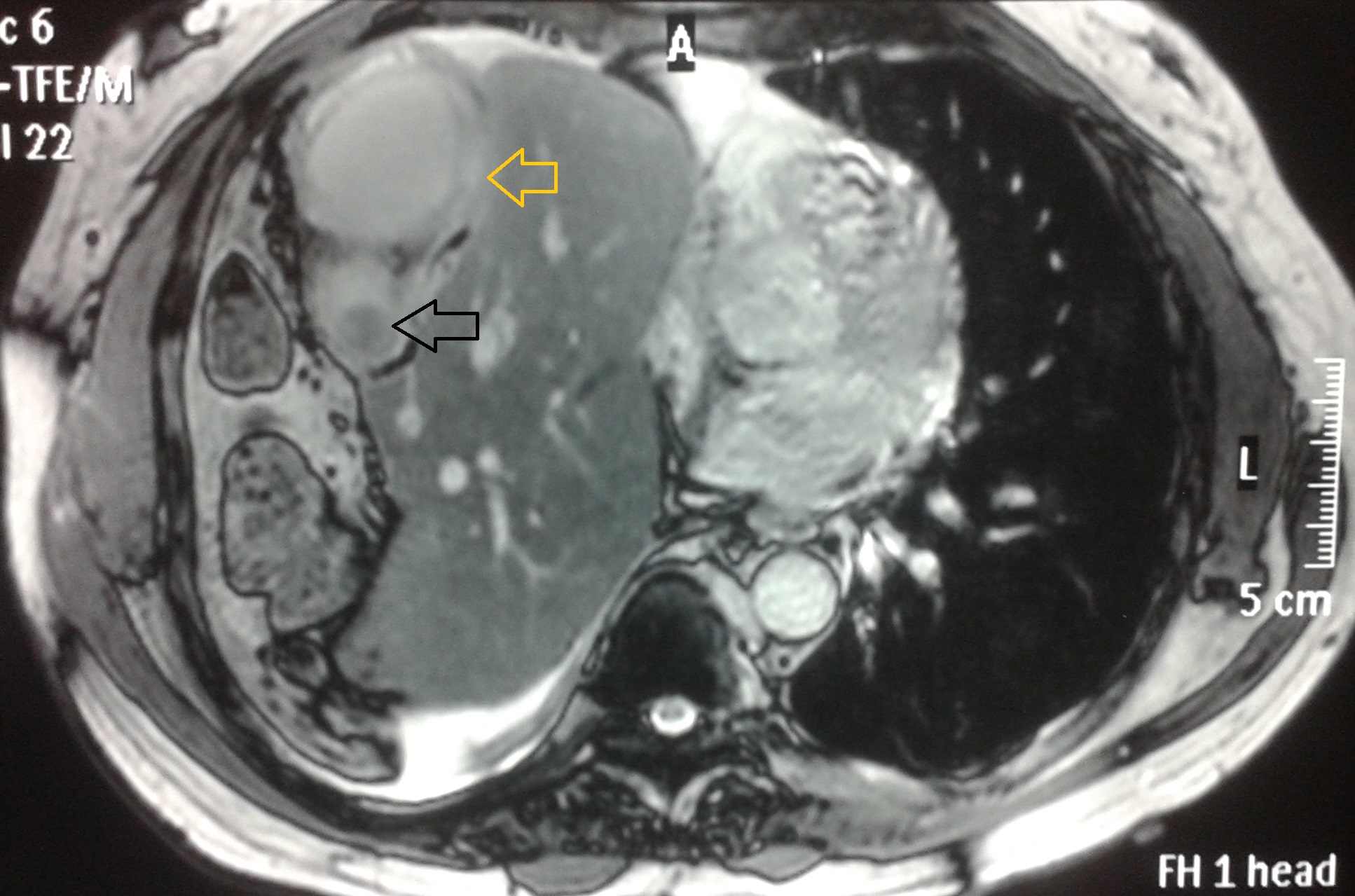
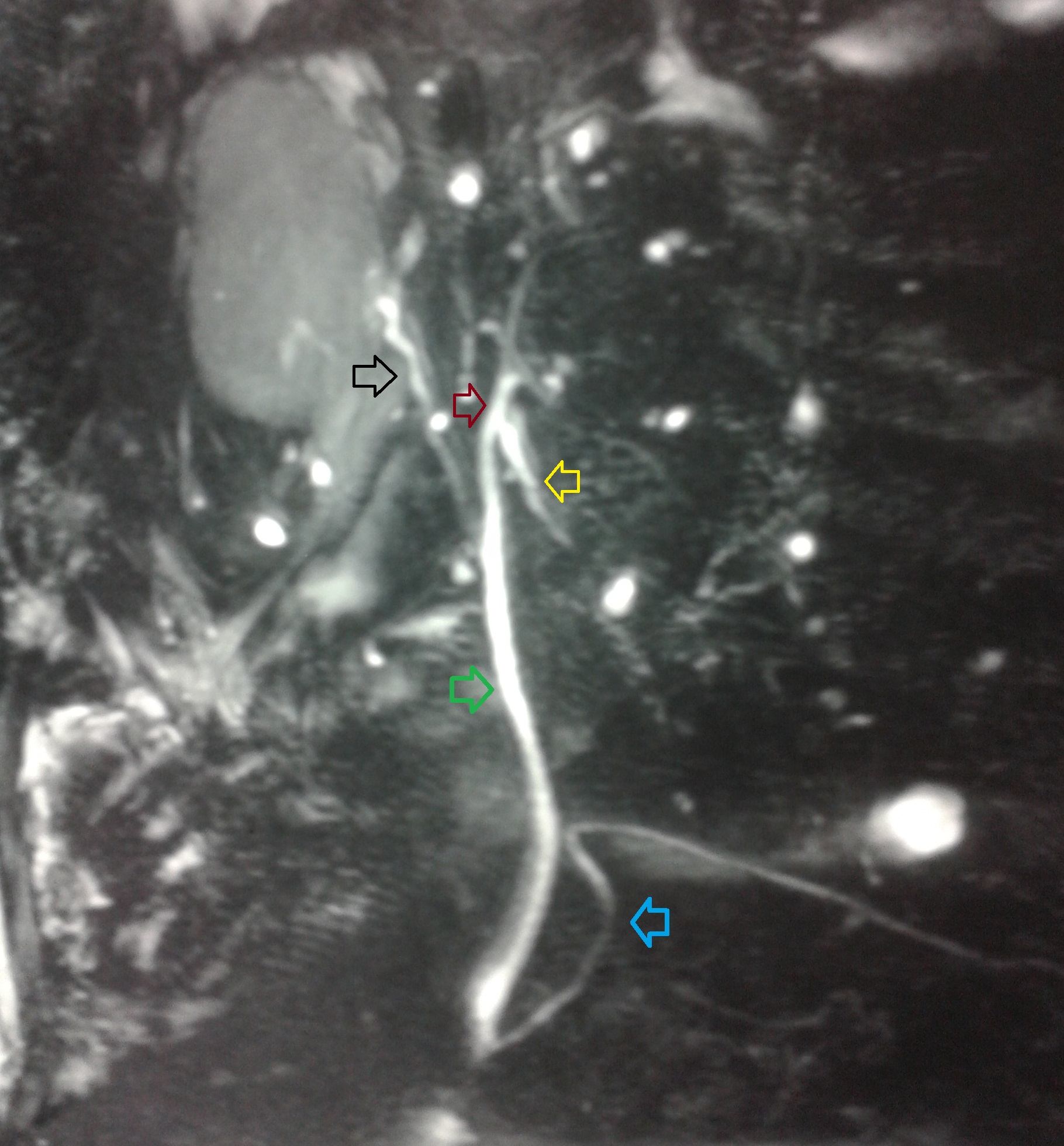
On examination he did not have pallor, icterus or pedal oedema. He had pressure sores at pressure points. Paraplegia affected him from the level of 2nd lumbar vertebra. Abdominal examinations were unremarkable except mild tenderness at right upper abdomen. On respiratory system examinations, trachea was deviated to left. Right chest was tympanic with no breath sounds. Blood investigations revealed haemoglobin of 12.5gm%, total leukocyte count of 11790/cumm, bilirubin of 0.7mg/dl, alkaline phosphatase of 204unit/lit, normal transaminase levels and normal renal function test values. Computed Tomography (CT) scan of abdomen and chest was performed with the clinical suspicion of diaphragmatic hernia. It showed right sided diaphragmatic hernia with herniated intrathoracic liver, gall bladder and colon. Gall bladder was thick walled and containing a large calculus [Table/Fig-1]. A Magnetic Resonance Imaging (MRI) with cholangiopancreaticography (MRCP) was planned to rule out any biliary obstruction as the alkaline phosphatase was high. It revealed right sided diaphragmatic dehiscence with herniation of liver and large bowel, compression of right lung and shifting of mediastinum to left. Gall bladder was distended and its wall had diffuse irregular thickening [Table/Fig-2]. On T2 weighted images gall bladder wall was heterogeneous and had areas of high T2 signal suggesting wall oedema. There was pericholecystic fat stranding. One 2 cm calculus was impacted at gall bladder neck [Table/Fig-3]. MRCP did not suggest any intrahepatic or extrahepatic biliary dilatation or luminal filling defect, but a stretched and elongated bile duct [Table/Fig-4]. He was planned for surgical management. Pre-operative pulmonary evaluation, echocardiography and arterial blood gas analysis were all normal.
CT scan axial view of thorax and upper abdomen showing right diaphragmatic hernia, hepatothorax (white circle) and large radio-opaque gall bladder calculus (arrow).
MRI chest and upper abdomen coronal view showing herniated liver, inflamed gall bladder and colon in right chest cavity with compression of right lung mediastinal shift. Black arrow shows inflamed thick walled gall bladder; red arrow shows ascending aorta; blue arrow points right colic flexure; black and red circle mark right and left lobe of liver respectively.
T2 weighted MRI axial scan showing diffuse irregular thickening of gall bladder wall with heterogeneous appearance and having areas of high T2 signal suggesting wall oedema (yellow arrow). Black arrow shows gall stone.
MRCP showing stretched and elongated bile duct and long cystic duct but no luminal filling defect. Black arrow points cystic duct; red and yellow arrow show right hepatic duct and left hepatic duct respectively; green arrow shows common bile duct and blue arrow, pancreatic duct.
As the patient had been paraplegic for last 24 years and remained asymptomatic from diaphragmatic dehiscence for the same long period before he became symptomatic one week back for acute cholecystitis, cholecystectomy alone was planned. Laparoscopic intervention was attempted. But in presence of dense pericholecystic adhesions with right intrathoracic location of liver and gall bladder it was converted to open procedure through an antero-lateral thoracoabdominal approach. Adhesions were divided. There was thick walled distended empyema gall bladder containing a 2 cm large calculus in the neck with areas of wall necrosis. Cholecystectomy was performed and wound closed keeping a tube drain in situ. Post-operative period was uneventful. Drain was removed on 2nd post-operative day and patient was discharged on 7th post-operative day. Histopathology confirmed acute cholecystitis. Patient is now doing well with 12 months follow-up.
Discussion
Traumatic diaphragmatic hernia is an uncommon condition affecting 0.8- 5.8% of blunt thoraco-abdominal trauma and 10-15% of penetrating trauma [1]. It mainly affects left side. Right sided involvement is rare because of buffering effect of liver; with an incidence of 5-19% of all traumatic diaphragmatic rupture [2]. A sudden high velocity force from high speed motor vehicle injury or fall from height increases the trans-diaphragmatic pressure gradient between the abdominal and the thoracic compartments. High abdominal positive pressure as a result of trauma pushes abdominal viscera into thoracic cavity in its negative pressure status with the phase of respiration [3]. Intrathoracic migration of abdominal viscera is observed in only 20% cases of right sided injury. Wide ranges of associated injuries involving liver, spleen, lung, kidney, pelvis or spine are quite common in high velocity injury and complicate the immediate outcome. Early mortality after right diaphragmatic injury often reaches around 30% [4]. Visceral herniation is often life threatening in acute setting due to tension viscerothorax with resultant fall in venous return to the heart and diminished cardiac output. The delayed rupture of a diaphragm may occur several days or even years after the initial injury as the devitalisation of the diaphragmatic muscle caused by the initial injury continues as a barrier until the inflammatory process weakens and ruptures it [5]. Strug et al., classified the diaphragmatic ruptures as Type I (immediate onset of clinical symptoms) and Type II (late onset of symptoms) [6]. Immediate symptoms are upper abdomen and chest pain, dyspnoea, cyanosis and hypotension [7]. Early detection in acute phase is sometimes missed or often masked by other associated injuries, which may lead to grave outcome. Few patients may go completely unnoticed and may become symptomatic after variable period of time when herniation occurs or problems arise from the hernia contents like obstruction, strangulation or inflammation [8].
A chest X-ray is usually the first investigation in suspected cases of diaphragmatic injury, but without herniation of viscera it is difficult to establish the diagnosis. X-ray has overall sensitivity and specificity of 17-40% [9]. A marked elevation of the hemidiaphragm, a distorted or obliterated diaphragmatic outline or a contra-lateral mediastinal shift on chest X-ray may suggest a diaphragmatic rupture [10]; but an intrathoracic herniation of abdominal viscera with or without the “collar sign” (focal visceral constriction at the site of tear) and demonstration of nasogastric tube above the diaphragm on left side are more specific [9]. A CT scan is of superior diagnostic value with a specificity of nearly 100% and a sensitivity of 50% for right sided ruptures [11]. In 2009 Rashid et al., performed a systematic literature review on 13 cases of reported right sided diaphragmatic injury, with herniated liver only in 6 cases [7].
The operative treatment for diaphragmatic rupture consists of hernia reduction, pleural drainage and repair of the defect in acute or symptomatic delayed cases through transabdominal or transthoracic or combined approach [8]. Particularly in cases of chronic herniation of intra-abdominal organs into the thorax an abdomino-thoracic or thoracic approach may be necessary [4].
The present patient had blunt thoracoabdominal trauma 24 years back and he was diagnosed to have right diaphragmatic hernia with herniation of liver and gall bladder during the evaluation of acute cholecystitis. CT chest and abdomen confirmed the diagnosis. Pre-operative liver function test revealed elevated alkaline phosphatase and most likely it was due to compression of bile duct by the large stone in the gall bladder neck or due to stretching of biliary tree, caused by herniation. We ruled out choledocholithiasis with the help of MRCP. Diaphragmatic hernia per say was asymptomatic in this case. Incidentally detected asymptomatic diaphragmatic hernia with wide gap may be left alone in high risk patients. So we justified our approach by doing a difficult cholecystectomy only through a thoracoabdominal approach.
Conclusion
Right sided diaphragmatic hernia is rare. Though it is a life threatening condition it can go un-noticed for variable period of time until it becomes symptomatic for hernia or for some disease process involving herniated organs or detected incidentally. High degree of suspicion is required to detect this condition which has immense importance in acute cases. CT scan is an optimum diagnostic tool. Traumatic right diaphragmatic hernia with acute cholecystitis as a fairly delayed case can be treated alone with cholecystectomy if the patient is asymptomatic for the hernia.
[1]. Reber P, Schmied B, Seiler C, Baer H, Patel A, Buchler M, Missed diaphragmatic injuries and their long-term sequelaeThe Journal of Trauma: Injury, Infection, and Critical Care 1998 44(1):183-88. [Google Scholar]
[2]. Matsevych O, Blunt diaphragmatic rupture: four year’s experienceHernia 2007 12(1):73-78. [Google Scholar]
[3]. Walchalk L, Stanfield S, Delayed presentation of traumatic diaphragmatic ruptureThe Journal of Emergency Medicine 2010 39(1):21-24. [Google Scholar]
[4]. Boulanger B, Milzman D, Rosati C, Rodriguez A, A comparison of right and left blunt traumatic diaphragmatic ruptureThe Journal of Trauma: Injury, Infection, and Critical Care 1993 35(2):255-60. [Google Scholar]
[5]. Lee H, Jeon I, Kim S, Jung Y, Delayed traumatic diaphragm hernia after thoracolumbar fracture in a patient with ankylosing spondylitisJ Korean Neurosurg Soc 2015 57(2):131 [Google Scholar]
[6]. Strug B, Noon G, Beall A, Traumatic diaphragmatic herniaThe Annals of Thoracic Surgery 1974 17(5):444-49. [Google Scholar]
[7]. Rashid F, Chakrabarty M, Singh R, Iftikhar S, A review on delayed presentation of diaphragmatic ruptureWorld J Emerg Surg 2009 4(1):32 [Google Scholar]
[8]. Vilallonga R, Pastor V, Alvarez L, Charco R, Armengol M, Navarro S, Right-sided diaphragmatic rupture after blunt trauma. An unusual entityWorld J Emerg Surg 2011 6(1):3 [Google Scholar]
[9]. Worthy S, Kang E, Hartman T, Kwong J, Mayo J, Müller N, Diaphragmatic rupture: CT findings in 11 patientsRadiology 1995 194(3):885-88. [Google Scholar]
[10]. Gelman R, Mirvis S, Gens D, Diaphragmatic rupture due to blunt trauma: sensitivity of plain chest radiographsAmerican Journal of Roentgenology 1991 156(1):51-57. [Google Scholar]
[11]. Shanmuganathan K, Killeen K, Mirvis S, White C, Imaging of diaphragmatic injuriesJournal of Thoracic Imaging 2000 15(2):104-11. [Google Scholar]