Retroperitoneal Haematoma in a Patient with Dengue Haemorrhagic Fever: A Rare Case Report
Jasminder Singh1, Harpreet Singh2, Gagandeep Sukhija3, Ruchi Jagota4, Saroj Bala5
1 Assistant Professor, Department of Medicine, Pt. BD Sharma PGIMS, Rohtak, Haryana, India.
2 Senior Professor, Department of Medicine, Pt. BD Sharma PGIMS, Rohtak, Haryana, India.
3 Senior Resident, Department of Medicine, Pt. BD Sharma PGIMS, Rohtak, Haryana, India.
4 Postgraduate Resident, Department of Medicine, Pt. BD Sharma PGIMS, Rohtak, Haryana, India.
5 Postgraduate Resident, Department of Medicine, Pt. BD Sharma PGIMS, Rohtak, Haryana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gagandeep Sukhija, 529, A Model Town, Karnal, Haryana, India.
E-mail: gagan43@gmail.com
Dengue Haemorrhagic Fever (DHF) has diverse manifestations ranging from asymptomatic petechial skin haemorrhages to life threatening cerebral, pulmonary, gastrointestinal and genitourinary haemorrhages. However, the association of spontaneous retroperitoneal haematomas with DHF is not well documented in literature. We report a rare case of spontaneous retroperitoneal haematoma complicating DHF.
Complications, Dengue fever, Non specific antigen-1
Case Report
A 30-year-old male diagnosed as a case of dengue fever, presented to the emergency department with high grade fever of two days duration with marked weakness in both the legs (unable to stand) and bleeding from oral and nasal cavities. The patient was febrile, vitals were stable and physical examination revealed evidence of hepatomegaly. His initial investigations showed Non-Structural Protein 1 (NS1) Antigen positive, Hemoglobin 14.6gm%, Total Leucocyte Count (TLC)-4500/cumm, Differential Leucocyte Count (DLC)-80% polymorphs, 15% lymphocytes, 3% monocytes and 2% eosinophils; platelet count of 50,000/cumm with a normocytic normochromic blood picture and International Normalized Ratio (INR)-1.29. Ultrasound showed liver of size 17.2cm with fatty infiltration, gallbladder slightly oedematous whereas, size of spleen, kidneys and pancreas was within normal limits. Patient was treated symptomatically with intravenous fluids, platelet transfusions and anti-pyretics and his general condition improved and he became afebrile, although his platelet count was consistently between 30,000 and 60,000/cumm. But on fourth day of admission patient developed intense pain in the right iliac fossa referred to back. The pain was of continuous type, associated with marked nausea, and not relieved by medication. Additionally he had developed breathlessness and abdominal distension. Physical examination revealed he was afebrile, had developed pallor, mild icterus and a distended abdomen with marked tenderness; bowel sounds were sluggish and air entry was decreased in bilateral lung fields.
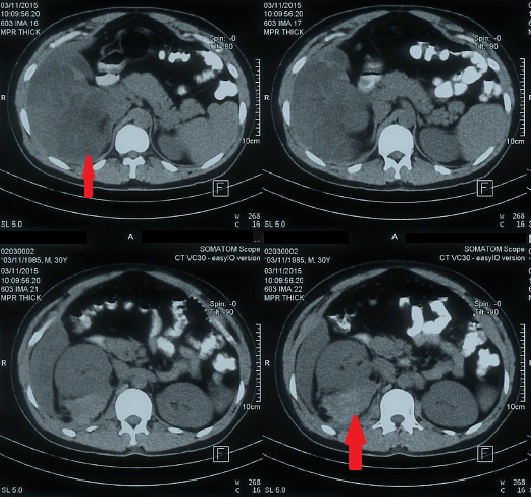
Laboratory investigations revealed a complete haemogram of Hemoglobin (Hb)-3.5gm%; TLC-10,000/cumm, with predominant neutrophilia and platelet count of 20,000/cumm, serum bilirubin-3.9mg%; SGOT/SGPT were 95/90 IU; serum alkaline phosphatase-132 IU; serum proteins-4.9gm%; Prothrombin Time Index (PTI)-1.2; and serum creatinine-1.1mg%. Serology was negative for HIV, HBsAg and anti-HCV. The second ultrasound showed free fluid in the abdomen, bilateral pleural effusion and alteration in the echotexture of liver and kidneys and a hypoechoic lesion of 14cm by 6cm size lateral to right kidney in the right pararenal space extending along right psoas muscle; possibly retroperitoneal haematoma. Follow-up CT abdomen showed possibility of an intra-parenchymal haematoma in the liver with extension to right peritoneum and right psoas muscle haematoma. Active extravasation of contrast on CT scan suggestive of active bleeding was not found [Table/Fig-1]. Surgeon opined for conservative management. Patient was given prophylactic antibiotics, multiple blood transfusions including platelet transfusions and other supportive care. His symptoms and platelet count slowly improved to normal in a week. He was discharged in stable condition with advice to follow-up especially for sonography of the intra-abdominal collection. His thrombophilia profile done after 6 weeks of discharge from the hospital was reported normal.
CT scan abdomen showing intra-parenchymal haematoma in the liver with extension to right peritoneum and right psoas muscle haematoma.
Discussion
Although spontaneous hematomas have been described in the retroperitoneum along with other sites like thorax and abdomen; they are often shown to be associated with some or the other predisposing factors like aneurysms, anticoagulation or bleeding diathesis in the patient [1]. The common causes of retroperitoneal haematoma are trauma to the lower back, pelvis or abdomen, anticoagulation, rupture of aortic/renal aneurysm, acute pancreatitis, malignancy especially renal or adrenal, injury during procedures like aortography/cardiac catheterization or femoral cannulation, polyarteritis nodosa, renal abscess, rupture of renal cysts, pyelonephritis, adrenal haemorrhage in sepsis, burns or trauma, phaeochromocytoma, adrenal carcinoma/adenoma, use of antithrombotic agents like aspirin or clopidogrel. In our patient there was no history of trauma/procedures/use of implicated drugs; no evidence of a mass/cyst/aneurysm/inflammatory conditions like abscess /pyelonephritis/ polyarteritis nodosa. Although DHF has been reported to be associated with atypical manifestations like encephalitis/encephalopathy, myocarditis, hepatitis, cholecystitis, muscle haematomas etc., the association of spontaneous retroperitoneal haematoma with DHF without any other underlying cause is very uncommon [2,3]. A few case reports of DHF with retroperitoneal haematoma have been reported [4–6]. These could be massive leading to shock [6], or may present as compression syndrome. The pathogenesis of bleeding in dengue fever is thought to be due to exaggerated immune response of the host to the dengue virus (generally a secondary infection, when the host’s immune system has been primed by a primary dengue virus infection). This hyper immune response of the host then causes endothelial dysfunction, increased vascular permeability and thrombocytopenia with or without platelet dysfunction [7].
Conclusion
DHF is becoming more and more common now-a-days due to increasing prevalence, the world over and clinicians must be vigilant to its rare but life threatening manifestations like spontaneous retroperitoneal haematomas; which like haemorrhages in other major organs or body cavities need prompt diagnosis and management with intravenous fluids and platelet transfusions and timely surgical intervention in case of complications like compartment syndrome/ increasing haematoma size due to active bleeding indicated by CT examination showing active extravasation of contrast.
[1]. Koshy JM, John M, Rathore S, George UB, Spontaneous muscle hematomas in a patient with dengue hemorrhagic feverCHRISMED J Health Res 2014 1:201-02. [Google Scholar]
[2]. http://www.apiindia.org/pdf/medicine_update_2010/infectious_disease_01.pdf: Dengue fever in India: an overview [Google Scholar]
[3]. Chaturvedi U C, Nagar R, Dengue and dengue haemorrhagic fever: Indian perspectiveJ Biosci 2008 33:429-41. [Google Scholar]
[4]. Ameer AM, Arachchi W, Jayasingha PA, Psoas haematoma complicating dengue haemorrhagic fever: a case reportGalle Med J 2009 14(1):83-84. [Google Scholar]
[5]. Chan KP, Lau GK, Doraisingham S, Chan YC, Adult dengue deaths in SingaporeClin Diagn Virol 1995 4(3):213-22. [Google Scholar]
[6]. Mathew A, Rothman AL, Understanding the contribution of cellular immunity to dengue disease pathogenesisImmunol Rev 2008 225:300-13. [Google Scholar]
[7]. Ganu S, Mehta Y, Femoral compressive neuropathy from iliopsoas haematoma complicating dengue haemorrhagic feverAsian Pac J Trop Med 2013 6(5):419-20. [Google Scholar]