Post-Traumatic Ectopic Nail: A Case Report and Review of Literature
Susanta Meher1, Tushar Subhadarshan Mishra2, Prakash Kumar Sasmal3, Bikram Rout4, Rakesh Sharma5
1 Senior Resident, Department of Surgery, AIIMS, Bhubaneswar, Odisha, India.
2 Associate Professor, Department of Surgery, AIIMS, Bhubaneswar, Odisha, India.
3 Assitant Professor, Department of Surgery, AIIMS, Bhubaneswar, Odisha, India.
4 Senior Resident, Department of Surgery, AIIMS, Bhubaneswar, Odisha, India.
5 Senior Resident, Department of Surgery, AIIMS, Bhubaneswar, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Susanta Meher, Senior Resident, Department of Surgery, AIIMS, Bhubaneswar-751019, Odisha, India.
E-mail: chikusus@gmail.com
Ectopic nail or Onychoheterotopia is an uncommon clinical entity. They are usually congenital; the acquired variety is very rare. The exact pathogenesis of the disease is not clear. They present as a nail like outgrowth, distinct from the classic nail units which is usually asymptomatic. The dorsal aspect of fingers and toes are mostly affected. We present a case of a 24-year-old male with post-traumatic ectopic nail of right middle finger. Complete surgical excision of the ectopic nail was done with its germinal matrix. The patient didn’t have any evidence of recurrence after one year of follow-up, with satisfactory cosmetic outcome. This article highlights the classic presentation of a case of ectopic nail with its surgical management and brief review of literature.
Germinal matrix, Onychoheterotopia, Recurrence, Surgical excision
Case Report
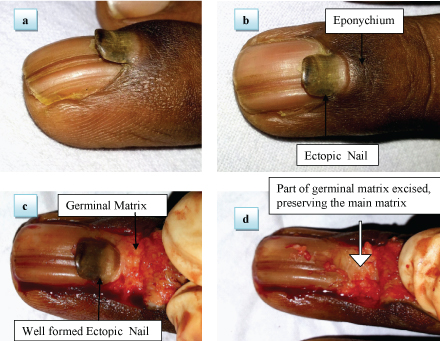
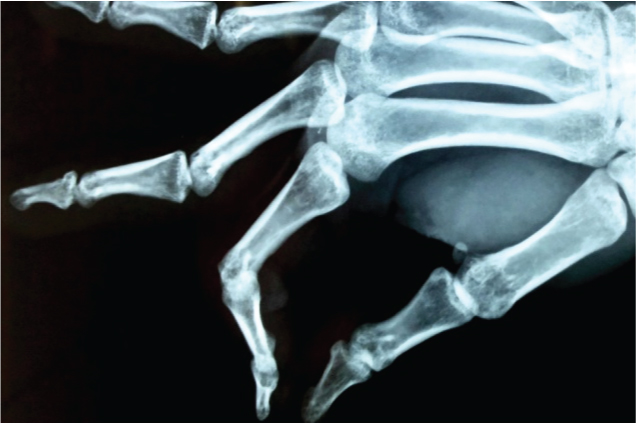
A 24-year-old gentleman presented to us with complaint of an ectopic nail over the right middle finger. He sustained an injury to the same site two years before, while playing basketball. Three months following an injury he noticed a nail like outgrowth projecting over the nail of the right middle finger [Table/Fig-1a,b], which was growing at the same speed as that of the underlying nail. He trimmed the nail thrice, but it reappeared every time. The ectopic nail was not associated with pain, swelling, itching or any bony deformity. On physical examination a solitary well defined nail of size 8mm x 7mm found on the top of the normal nail arising from the eponychium [Table/Fig-1a,b]. The ectopic nail was darker than the underlying nail. No other obvious abnormality was found on examination except a vertical groove on the underlying nail. X-ray of the affected finger didn’t reveal polydactyly or any bony abnormality [Table/Fig-2]. With a diagnosis of ectopic nail complete excision of the nail with its germinal matrix was planned.
(a) Post traumatic ectopic nail right middle finger (lateral view) with a well formed ectopic nail; (b) Ectopic nail arising from the eponychium; (c) Ectopic nail after exposure of the rectangular skin flap showing a well formed ectopic nail; (d) Ectopic nail excised with a part of the germinal matrix.
X-Ray right hand (Lateral view) with no evidence of bony changes.
Under strict aseptic condition, local anaesthesia (1% lignocaine) was infiltrated at the base of the finger and ring block was given. A vertical skin incision was made from the proximal nail fold up to 1cm proximally on either side of the ectopic nail. A rectangular skin flap was raised. A well defined square shaped solitary ectopic nail was identified, arising from the germinal matrix, without any adherence to the underlying nail [Table/Fig-1c]. The ectopic nail was excised along with a part of the germinal matrix from which it was arising [Table/Fig-1d]. The wound was then covered with the raised skin flap and a dressing was done. No suturing of the flap was done. The wound healed normally within 7 days of surgery. Excision of the ectopic nail with a part of the germinal matrix is essential to prevent recurrence after excision. Histopathological examination revealed a well formed nail with germinal matrix without a granular layer.
After one year of follow-up, the patient did not have any evidence of recurrence of the ectopic nail and the patient had cosmetically acceptable result [Table/Fig-3a,b].
(a) Follow-up photograph after one month of operation; (b) Photogragh after one year follow up with improved and satisfactory cosmetic outcome.

Discussion
Developement of nail tissue in a location other than the usual nail unit is termed as ectopic nail or onychoheterotopia. Ohya et al., (1931) were the first to describe ectopic nail [1]. Since then only few cases have been reported [2–11] [Table/Fig-4].
Published literature on post-traumatic ectopic nail till 2016 literature searched on PubMed.
| Sl. No | References | Year of Publication | Number of Cases | Site of Involvement | Management |
|---|
| Present case | 2016 | 1 (24-year-old male) | right middle finger | Excision, rectangular skin flap |
| 1 | Greywal T et al., [2] | 2015 | 1 (six-year-old girl) | Finger (dorsum) | Excision |
| 2 | Khurana A et al., [3] | 2015 | 1 (50-year-old, Male/ Farmer) | Finger (dorsum) | Excision |
| 3 | Thakur BK et al., [4] | 2016 | 1 | Finger | Excision |
| 4 | Sharma R et al., [5] | 2015 | 2 (35-year-old/ Male) | Finger(Palmar) | Not Excised |
| 5 | Sehgal VN et al., [6] | 2014 | 1 | Finger | Excision |
| 6 | Caliskan E et al., [7] | 2014 | 1 (21-year-old male) | Finger, dorsum bipartite nail | Excision done with two incision |
| 7 | Hwang SM et al., [8] | 2013 | 1 (eight-year-old girl) | Finger (left thumb/ dorsum) | Excision with matrix |
| 8 | Rajasekhar M et al., [9] | 2006 | 1 (19-year-old manual labourer) | Finger | Excision |
| 9 | Goikoetxea X et al., [10] | 2006 | 1 | Finger | Excision |
| 10 | Sasmaz S et al., [11] | 2004 | 1 (32-year-old male) | Finger (dorsum) | Excision |
Most of them are congenital and the acquired variety is less commonly seen [7]. The exact pathogenesis of the disease is unknown, although various hypotheses have been proposed, which include ectopic existence of germ cells, the nail of a rudimentary or hidden polydactyly and traumatic transfer and inoculation of onycocytes [12]. Many reports show the association of ectopic nail with congenital disease like congenital palmar nail syndrome, Pierre Robin syndrome and patients having aberration of the long arm of chromosome 6 [1,13], which opens up a possibility of a familial tendency or genetic inheritence. Post traumatic ectopic nail may occur because of acute injury (defined as a single overhelming injury) or chronic injury (described as repeated minor injuries) which leads to splitting of germinal matrix and implantation into the skin [1,9].
Ectopic nail may present as a small outgrowth of a deviant nail or complete double finger nail malformation. They are usually asymptomatic but it can be associated with pain, pruritus and swelling. The congenital variety commonly affect the palmar aspect of 5th finger. Other fingers are less commonly affected [8]. Post- traumatic ectopic nail mostly affects dorsal aspect of finger and toe. Various pattern growth has been described for ectopic nail including vertical, horizontal and circumferrential growth [9]. Sometimes bony deformity can be found associated with this condition because of contact of the ectopic nail matrix to the periosteum which impedes intramembranous ossification leading to hypoplasia and thinning of the underlying bone [8,9].
Other conditions which can be confused with ectopic nail includes rudimentary polydactyly, foreign body, hamartoma, slit nail deformity and cutaneous horn etc., [1,8]. Histopathological diagnosis is based upon the presence of a fully developed nail unit, including a corneous nail plate and nail matrix. An ectopic nail must have the nail matrix but does not necessarily require a nail bed [8]. Regardless of the type, the standard treatment of ectopic nail is total surgical excision of the nail unit including the nail matrix. Partial excision frequently leads to reccurence of the same [9].
Conclusion
Complete excision of the ectopic nail with its matrix, preserving the matrix of the normal nail is important for prevention of recurrence and maintaining cosmesis. The presence of a rudimentary polydactyly should be ruled out by an X-ray before embarking upon the treatment of an ectopic nail. Both oblique incision and rectangular skin flap can be used for complete exposure of the nail matrix depending on the site of presentation of the ectopic nail.
Author’s contribution: Dr Susanta and Dr Bikram prepared the manuscript. Dr Tushar and Dr Prakash critically revised the article.
[1]. Riaz F, Rashid RM, Khachemoune A, Onychoheterotopia: Pathogenesis, presentation, and management of ectopic nailJ Am Acad Dermatol 2011 64(1):161-66. [Google Scholar]
[2]. Greywal T, Maronas-Jimenez L, Friedlander SF, Onychoheterotopia Due to a Traumatically Transplanted Nail in a ChildPediatr Dermatol 2015 32(6):e305-06. [Google Scholar]
[3]. Khurana A, Sehgal VN, Aquired ectopic nail or onychoheterotopiaIndian J Dermatol 2015 60(6):621-22. [Google Scholar]
[4]. Thakur BK, Verma S, Jitani A, Post-traumatic ectopic nailIndian J Dermatol Venereol Leprol 2016 82:416 [Google Scholar]
[5]. Sharma R, Verma P, Singal A, Yadav P, Posttraumatic onychoheterotopia: a report of two casesSkinmed 2015 13(6):483-84. [Google Scholar]
[6]. Sehgal VN, Chatterjee K, Chaudhuri A, Chatterjee G, Acquired/post-traumatic ectopic nail: onychoheterotopiaSkinmed 2014 12(5):306-07. [Google Scholar]
[7]. Caliskan E, Dincer D, Acikgoz G, Koc E, Post-traumatic ectopic nail: a usual manifestation and treatment of an unusual anomalyAnn Dermatol 2014 26(6):768-69. [Google Scholar]
[8]. Hwang S-M, Cho K-H, Kim H-D, Jung Y-H, Kim H-I, Post-traumatic ectopic nailArch Plast Surg 2013 40(6):793-94. [Google Scholar]
[9]. Rajashekar M, Bhandary S, Shenoy M, Sali AR, Post-traumatic ectopic nailJ Postgrad Med 2006 52(3):218 [Google Scholar]
[10]. Goikoetxea X, Etxebarria I, Careaga M, Post-traumatic ectopic nail: case reportJ Hand Surg Am 2006 31(5):819-21. [Google Scholar]
[11]. Sasmaz S, Coban YK, Gumusalan Y, Boran C, Post-traumatic ectopic nailJournal of the American Academy of Dermatology 2004 :323-24. [Google Scholar]
[12]. Ena P, Ena L, Ferrari M, Mazzarello V, Ectopic foot nails: clinical and dermoscopic features, treatment and outcome in 20 casesDermatology 2015 231(4):298-303. [Google Scholar]
[13]. Narang T, Kanwar AJ, Ectopic nail with polydactylyJournal of the American Academy of Dermatology 2005 :1092-93. [Google Scholar]