Choriocarcinoma in Ongoing Pregnancy Presenting with Intracranial Metastasis
Sujata Siwatch1, Vanita Suri2, Pooja Sikka3, Neelam Aggarwal4, Seema Chopra5
1 Assistant Professor, Department of Obstetrics and Gynecology, PGIMER, Chandigarh, India.
2 Professor, Department of Obstetrics and Gynecology, PGIMER, Chandigarh, India.
3 Associate Professor, Department of Obstetrics and Gynecology, PGIMER, Chandigarh, India.
4 Additional Professor, Department of Obstetrics and Gynecology, PGIMER, Chandigarh, India.
5 Associate Professor, Department of Obstetrics and Gynecology, PGIMER, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sujata Siwatch, Department of Obstetrics and Gynecology, PGIMER, Sector-12, Chandigarh, India.
E-mail: siwatch1@yahoo.com
Choriocarcinoma presents usually as persistent trophoblastic disease, with prognosis worsening with duration from antecedent pregnancy. We present a unique case of a woman with choriocarcinoma who presented in the third trimester of pregnancy with eclampsia. She was managed with magnesium sulphate and underwent a caesarean section. However, she developed seizures in the post-partum period that were further investigated and attributed to intracranial metastatic lesions of Gestational Trophoblastic Neoplasia (GTN). We discussed the diagnostic challenge in this rare case of GTN and the grave potential it can have in such a presentation, as in our patient.
Eclampsia, Gestational trophoblastic disease, Magnesium sulphate
Case Report
A 24–year-old lady presented to the labour room, referred at 35 weeks 6 days period of gestation in her second pregnancy in view of eclampsia. In her first pregnancy, she had undergone an elective caesarean section at term for transverse lie. In the index pregnancy, her antenatal period was uneventful and blood pressure records were within normal limits. She complained of headache for the last few days and suffered a generalised tonic clonic seizure 4 days back at home. Thereafter, she was admitted to a local hospital where her vitals were monitored. Here, again she suffered another seizure. Fundus examination showed blurring of disc margins. An ultrasound revealed oligohydramnios and poor fetal movements and tone. She received diazepam and was referred to our tertiary care institute for better maternal and neonatal care.
At presentation, the patient had 2 episodes of vomiting. She was drowsy, oriented with a pulse of 120/minute and a blood pressure of 130/80- 140/94 mmHg. Spot urine albumin was 1+. She received Magnesium sulphate in view of eclampsia. Bishop’s score was 1. Fetal tone was sluggish and liqor reduced on biophysical profile. Her blood counts revealed haemoglobin of 7.6g/dl and a platelet count of 2.02 lacs/cc. She underwent an emergency caesarean section under spinal anaesthesia in view of previous caesarean section with poor Bishops score, poor biophysical profile and eclampsia. She delivered a live born girl, 2.1 kg with an Apgar score of 8 and 9 with no congenital malformations. Her blood pressure records remained normal post-operatively and received Mgso4 for 24 hours post-operatively. On post-operative day 2, she suffered another generalised tonic clonic seizure. She was dilantinized. The lady complained of unilateral upper limb weakness and pain but it slowly reversed over 4 days.
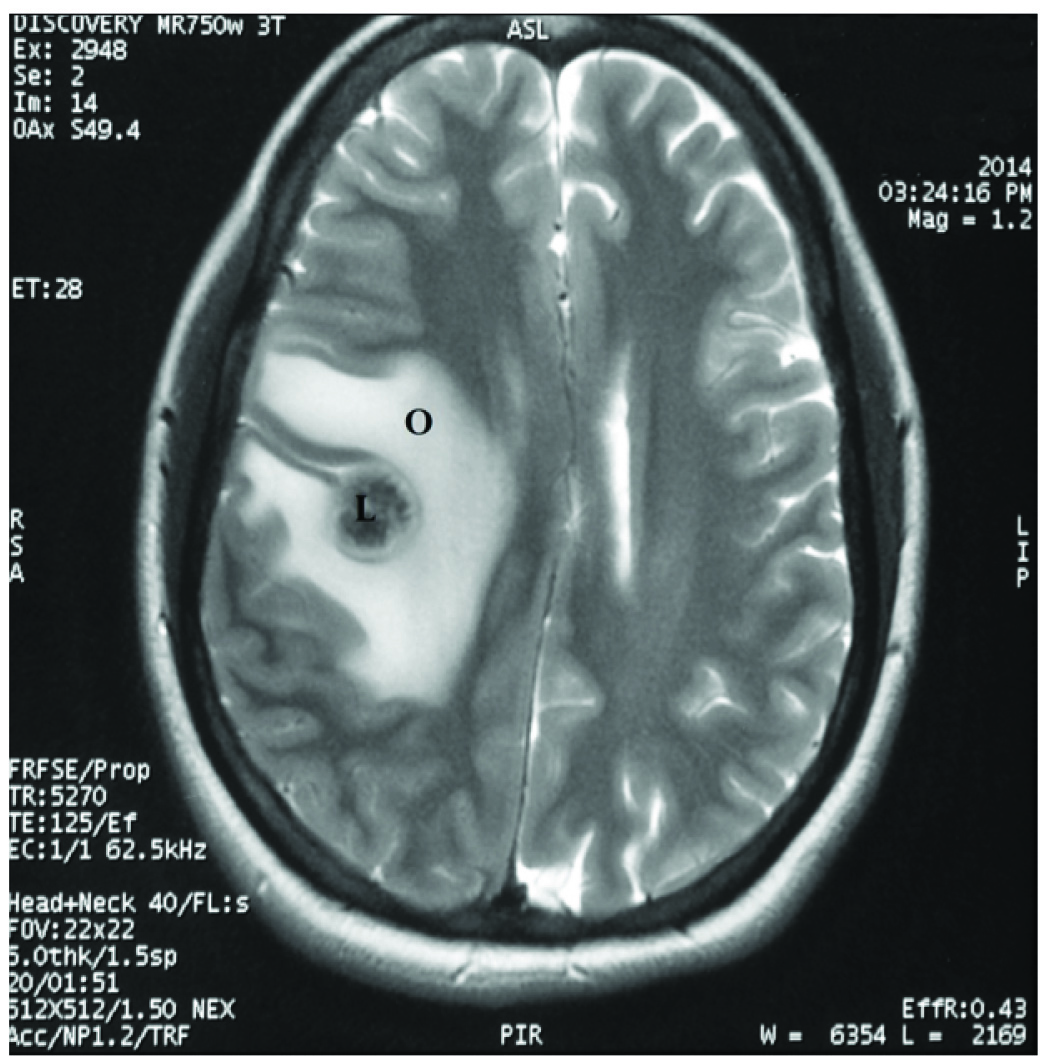
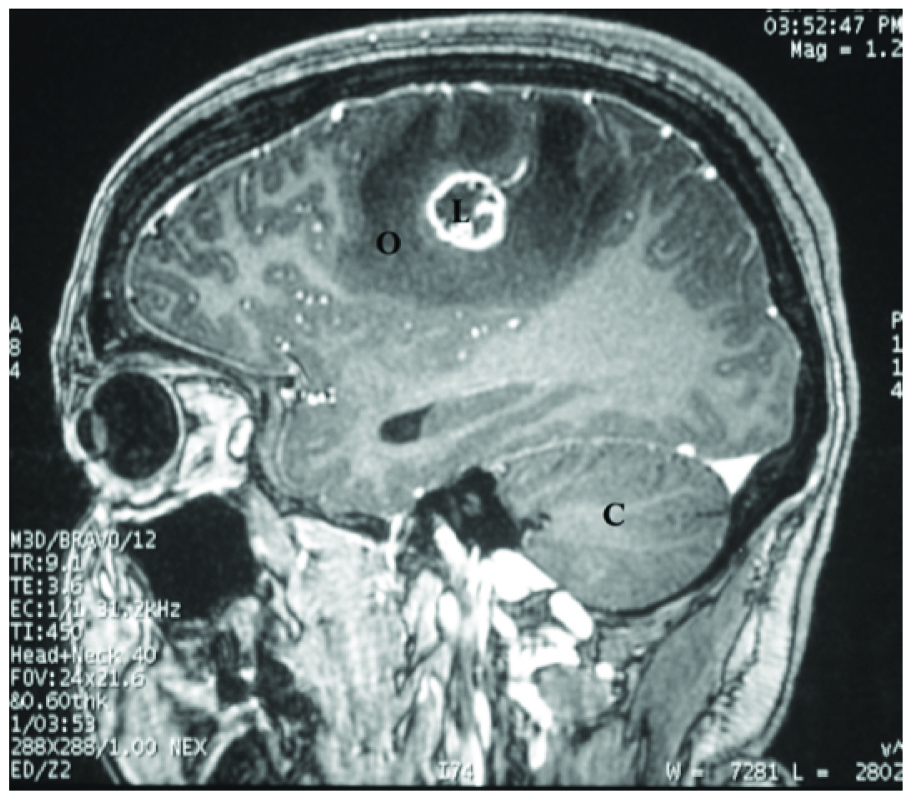
A fundus examination showed bilateral medial grade 1 retinal disc oedema. Non Contrast Computerised Tomography (NCCT) and Contrast Enhanced Computerised Tomography (CECT) with venography and Magnetic Resonance Imaging (MRI) were done which showed a ring enhancing lesion in the fronto-parietal lobe with peri-lesional oedema and another smaller nodular lesion in the right cerebellum [Table/Fig-1,2 and 3].
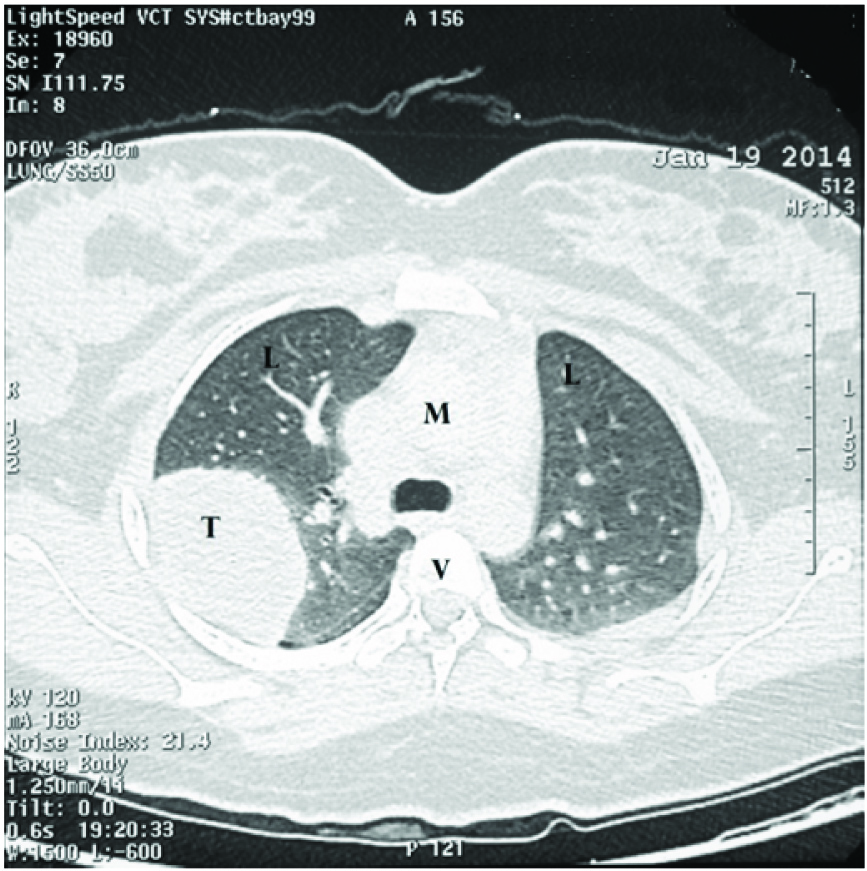
CT film of the chest showing metastasis in the lung. L-lung, M-mediastinum, T- tumour metastasis, V- vertebra.
An MRI film showing the lesion in the parietal lobe of the brain with peri-lesional odema. L-intracranial space occupying lesion (metastasis), O-peri-lesional odema.
An MRI film of the head (sagittal view) showing metastatic lesion in the parietal lobe with perilesional odema. L- intracranial space occupying lesion (metastasis), O- peri-lesional odema.
A provisional diagnosis of tuberculoma/ haemorrhage/ metastatic lesions was made and intravenous mannitol, acetazolamide and dexamethasone were initiated. She also received eptoin and levipil for seizure control and prophylaxis. A chest X-ray and CT of the chest and abdomen revealed multiple coin lesions in the chest and a large 4x5 centimetres mass in the right middle lobe. Ultrasound of the thyroid and breast was normal. A serum Beta-Human Chorionic Gonadotropin (HCG) was 30,000IU/ml (chemiluminescent assay) on day 5 which showed no fall after 2 days. A provisional diagnosis of Gestational Trophoblastic Neoplasia (GTN) was made. The patient underwent a guarded lumbar puncture. Cerebrospinal (CSF) Fluid Beta-HCG (CSF) of 1706 IU/ml. The blood: CSF Beta-HCG was 17.58 which confirmed the diagnosis of GTN with intracranial metastasis.
With a Féderation Internationale de Gynécologie et d’Obstétrique (FIGO) score of 10, she was started Etoposide, Methotrexate, Actinomycin D, Cyclosphosphamide, Vincristine (EMACO) chemotherapy. The intracranial lesions were vascular and intracranial irradiation was used in place of intrathecal chemotherapy due to raised intracranial hypertension. She received 11 cycles of EMACO therapy, 4 cycles of EMA- EP regimen and radiation to the brain during the fourth, for the CNS metastatic lesions. Chemotherapy was complicated with three fold rise in liver function tests after the first cycle and neutropenia after chemotherapy cycles, which improved with Filgrastin. Dexamethasone was gradually tapered. However, Beta-HCG started rising again after the fourth cycle of EMA EP regimen during the two month time she failed to follow-up due to social reasons. Fresh metastases were seen in the occipital lobe, cerebellum and chest. Chemotherapy was changed to cisplatin, paclitaxel and ifosfamide. She received 3 cycles of the same but continued to deteriorate with onset of headache, seizures, cranial nerve palsies, blurring of vision, chest pain and breathlessness. During this stormy period, she received analgesia, blood transfusions, filgastrin, broad spectrum antibiotics, mannitol, dexamethasone, anticonvulsants and even required intubation for altered mentation and seizures. Neurosurgery for acute neurological deterioration was refused by the patient. She finally succumbed to febrile neutropenia and acute kidney injury one and a half years after her initial presentation. However, she did not undergo autopsy.
Discussion
Choriocarcinoma is a complication of pregnancy found after 1:50,000 term pregnancies [1]. The early diagnosis of GTN within 4 months of the antecedent pregnancy is thought to carry a good prognostic value in the FIGO classification for the management of GTN. However, our case offers an exception to the above with the patient having wide spread metastasis to the lung and brain, even before the termination of the antecedent pregnancy in the third trimester.
There are few cases reported with widespread metastasis of choriocarcinoma reported during pregnancy [2–6]. In a queer case reported in 1990, Chandra et al., reported a neonatal death due to extensive intracranial bleed secondary to brain metastasis during pregnancy of placental choriocarcinoma [2]! The baby delivered to our patient was normal and asymptomatic. Baby was discharged and taken home by the family but died at 3 months of age due to acute gastroenteritis. Mamelak in 2002 reported a woman with choriocarcinoma who presented with significant neurological deficit at 30 weeks period of gestation secondary to brain metastasis [3]. She was managed initially with steroids, neurosurgery for mass removal and chemotherapy and radiation. In another case reported by Pinoce et al., in 2003, the patient had presented with headaches at 28 weeks pregnancy and was diagnosed due to the pulmonary and cerebral metastasis and high Beta-HCG values [4]. Early termination of pregnancy was done to expedite chemotherapy but still resulted in paraplegia for the patient. In our case too, the patient developed motor weakness which however, recovered over a short period of time, thus emphasizing the early diagnosis and management of the patient before life threatening intracerebral bleeding occurs.
The diagnosis of site of primary also poses a diagnostic dilemma. During pregnancy, placental tissue cannot be obtained till delivery. In our patient, the placenta was not saved for histopathology after the caesarean as the diagnosis was not suspected before the caesarean section. In our patient, the diagnosis of eclampsia was made due to the presence of urine albumin and a high blood pressure record. Again, with eclampsia presenting with no or few high blood pressure records [7], the need for pre-operative radiological examination seems important.
Beta-HCG is the marker used to diagnose and manage the treatment of GTN. Beta-HCG in pregnancy is raised and variable. This makes the diagnosis of choriocarcinoma difficult. According to Braunstein et al., Beta-HCG values plateau at about 10,000IU/ml after about 10 weeks period of gestation [8]. During early post-partum period, the Beta-HCG values fall exponentially [9]. However, in case of GTN, due to the persistent syncitiotrophoblastic tissue, rising values of HCG on serial blood draws every 48 hours may help in making the diagnosis of GTN. The serum to cerebrospinal fluid HCG ratio of less than 60 is thought to be indicative of brain metastasis of choriocarcinoma [1].
Different managements of brain metastasis of choriocarcinoma have included surgery, intrathecal methotrexate and radiation [10]. In our patient, we used cranial radiation therapy with chemotherapy. According to Evans et al., radiation with chemotherapy and intrathecal methotrexate offer a similar survival rates [10]. The role of surgery is limited to decompression of masses of haemorrhage or tumour causing increased intracranial hypertension and neurological worsening. CT scan did not show any evidence of haemorrhage in our patient, even at later neurological worsening. Multiple sites of metastasis made surgery a difficult option which the patient refused. She developed chemo resistance and developed new brain metastasis while receiving chemotherapy which has poor prognosis [10]. Even salvage chemotherapy could not benefit her. High risk score, intracranial metastasis at presentation in late gestation and delay in receiving the third cycle of EMA EP seemed to have resulted in the chemo resistance of the tumour in our patient.
Conclusion
One should think and rule out intracranial pathology in cases presenting with seizures in post-partum period in spite of intrapartum magnesium sulphate therapy and prompt delivery. Brain metastasis of choriocarcinoma should be considered a possibility in women with reproductive age group with haemorrhagic intracranial lesions of the brain. Furthermore, multidisciplinary involvement, early diagnosis and early termination of pregnancy followed by chemotherapy would go a long way to help avoid adverse serious life threatening complications associated with choriocarcinoma in pregnancy.
[1]. Athanassiou A, Begent RH, Newlands ES, Parker D, Rustin GJ, Bagshawe KD, Central nervous system metastases of choriocarcinoma. 23 years’ experience at Charing Cross HospitalCancer 1983 52(9):1728-35. [Google Scholar]
[2]. Chandra SA, Gilbert EF, Viseskul C, Strother CM, Haning RV, Javid MJ, Neonatal intracranial choriocarcinomaArch Pathol Lab Med 1990 114(10):1079-82. [Google Scholar]
[3]. Mamelak AN, Withers GJ, Wang X, Choriocarcinoma brain metastasis in a patient with viable intrauterine pregnancy. Case reportJ Neurosurg 2002 97(2):477-81. [Google Scholar]
[4]. Picone O, Castaigne V, Ede C, Fernandez H, Cerebral / of a choriocarcinoma during pregnancyObstet Gynecol 2003 102(6):1380-83. [Google Scholar]
[5]. McCue SA, Greene JB, Metastatic cerebral choriocarcinoma during pregnancyMinn Med 1980 63(3):164-66. [Google Scholar]
[6]. Dana A, Saldanha GJ, Doshi R, Rustin GJ, Metastatic cerebral choriocarcinoma coexistent with a viable pregnancyGynecol Oncol 1996 61(1):147-49. [Google Scholar]
[7]. Sibai BM, Stella CL, Diagnosis and management of atypical preeclampsia-eclampsiaAm J Obstet Gynecol 2009 200(5):481.e1-7. [Google Scholar]
[8]. Braunstein GD, Rasor J, Danzer H, Adler D, Wade ME, Serum human chorionic gonadotropin levels throughout normal pregnancyAm J Obstet Gynecol 1976 126(6):678-81. [Google Scholar]
[9]. Faiman C, Ryan RJ, Zwirek SJ, Rubin ME, Serum FSH and HCG during human pregnancy and puerperiumJ Clin Endocrinol Metab 1968 28(9):1323-29. [Google Scholar]
[10]. Evans AC Jr, Soper JT, Clarke-Pearson DL, Berchuck A, Rodriguez GC, Hammond CB, Gestational trophoblastic disease metastatic to the central nervous systemGynecol Oncol 1995 59(2):226-30. [Google Scholar]