Aging in humans portray the dynamic nature of it being a species and could be defined as a multi-dimensional change in growth and development over a period of time [1]. The care of the geriatric population have assumed utmost importance as aging is unavoidable. The geriatric population in Kerala holds the highest of 12.6% [2] against of national average of 8%. In India, any person of age 60 years and above is referred to as an elderly or senior citizen [2]. Of this population, 80% reside in rural areas, 40% below the poverty line and 73% being illiterate [3]. There is a need to highlight the medical and socio-economic problems that are being faced by the elderly people in India and strategies for bringing about an improvement in their quality of life also need to be explored.
Oral health has a strong biological, psychological and social consequence as it affects aesthetics, communication and quality of life. The various oral health problems affecting the elderly in India include dental caries, periodontal problems, tooth loss and oral cancer [3]. Complete tooth loss or being completely edentulous signifies death in dental well-being [4] and it constitutes a common and irreversible health problem in the elderly.
Quality of Life is a multi-dimensional and subjective construct which is anchored in an individual’s internal frame of reference. The perceptions of their position in life in the context of culture and value systems in which they live and in relation to their goals, expectations, standards and concerns, is now recognized as a valid parameter in patient assessment in all areas of physical and mental healthcare, including oral health [5].
Most of the gerontological studies have been concentrated on the institutionalised elderly population taken care of by old age homes and similar institutions [6,7]. There are no available studies reporting the prosthetic status and needs in correlation with oral health quality life in elderly non institutional population. The present study was conducted to assess the prosthetic status and needs for the home-borne elderly in the central part of Kerala, India for policy planning and implementation in the geriatric population of Kerala. Along with this, the facet of quality of life being highly impaired by edentulouness was ascertained.
Materials and Methods
This cross-sectional study was conducted in Aluva taluk of Ernakulum District (Cochin) Kerala Indian between from June 2014 to April 2015.
Ethical considerations: The scientific and ethical aspects of the protocol were reviewed and approved by the review board of the Amrita Institute of Medical Sciences, Kochi, Kerala, India. Written Informed consent was obtained from all the participants.
Study population: A study was conducted among the elderly people aged 60 years and above residing in the municipal boundaries of Aluva, Kochi, India.
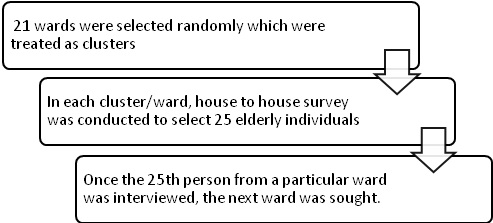
Selection of study subjects: Sampling unit consisted of municipal wards of Aluva Municipality, 21 wards were selected randomly which were treated as clusters. In each cluster i.e., ward, house to house survey was conducted to select 25 elderly individuals. Only those residents with names enlisted in the electoral list were recruited for the study confirming their residence. The elderly population was calculated from the existing electoral list procured from the municipality. Once the 25th person from a particular ward was interviewed, the next ward was sought [Table/Fig-1]. Kudumbashree is a female-oriented, community-based, poverty reduction project of Government of Kerala aiming at women empowerment. The Kudumbasree workers of the Aluva municipality were selected and initial training was given the questionnaire. This was done for a better house-to-house approach and assistance in recording.
Selection of study subjects.
Data collection: Information was collected and clinical examination was done by means of personal interviews administered by the qualified examiner and assisted by the Kudumbasree worker. The Oral Health Related Quality of Life (OHRQOL) was assessed by the local language (Malayalam) version of the Oral Health Impact Profile (OHIP-14) questionnaire and the prosthetic status and needs were recorded using the WHO Oral Health Assessment form (1997) [8].
Training and calibration: All the examinations were carried out by a single qualified examiner. The examiner was calibrated to senior expert for assessing the prosthetic status and needs and the intra-examiner was found to be 93%.
Study variables
Independent variables- These included socio-demographic variables like age, gender, education, occupation, place, diet etc., the reasons and duration of tooth loss and denture-wearing. The number of decayed, missing and filled teeth was also computed along with the existing prosthetic status and prosthetic needs.
Dependent variable- OHRQOL was measured by the Malayalam translation of the shorter version of the OHIP-14. This questionnaire consists of 14 items which are rated with options of never, sometimes and always. Also, the scores for the seven subscales of the OHIP-14 (functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability and handicap) were calculated.
Sample size estimation: The sample size was estimated to around 457 using following parameters expected proportion of 0.61%, precision of 5%, design effect of 1.25 at alpha error of 5%. The sample size was rounded off to 540 to cover the additional variables.
Pilot study: A pilot study was conducted in comparable age groups to see the feasibility of the study and to deduce the sample size. The sample size was calculated using the required formulae.
Statistical Analysis
The obtained data was coded and entered into the excel sheet. This was later transferred to the SPSS (Statistical Package for Social Sciences) software version 17, which was used for statistical analysis. ANOVA was used to find association between the different domains of the OHIP and prosthetic status and need.
Results
In the present study, a total of 539 study subjects were selected, of which 39.5% were males. Majority of the study population were from urban areas (97.8%) and were retired from service (work) (92.9%). Systemic illness was present in 70.1% of the study participants. The characteristics of study population are described in [Table/Fig-2].
Socio demographic characteristics of the study population.
| Demographic variables | Gender |
|---|
| Male | Female |
|---|
| n | % | n | % |
|---|
| Age | 60 - 69 years | 124 | 37.5 | 207 | 62.5 |
| 70 - 79 years | 70 | 46.4 | 81 | 53.6 |
| 80- 89 years | 17 | 34.7 | 32 | 65.3 |
| 90- 99 years | 2 | 25.0 | 6 | 75.0 |
| Place | Rural | 3 | 25.0 | 9 | 75.0 |
| Urban | 210 | 39.8 | 317 | 60.2 |
| Education | No formal education | 7 | 13.0 | 47 | 87.0 |
| Primary education | 38 | 27.9 | 98 | 72.1 |
| Secondary | 98 | 42.4 | 133 | 57.6 |
| Graduation | 5 | 55.4 | 45 | 44.6 |
| Post-graduation | 14 | 82.4 | 3 | 17.6 |
| Occupation | Present | 33 | 86.8 | 5 | 13.2 |
| No occupation/Retired | 180 | 35.9 | 321 | 64.1 |
| Diet | Vegetarian | 43 | 44.3 | 54 | 55.7 |
| Mixed diet | 170 | 38.5 | 272 | 61.5 |
| Systemic Illness | Present | 136 | 36.0 | 242 | 64.0 |
| Absent | 66 | 52.8 | 59 | 47.2 |
| Not aware | 11 | 30.6 | 25 | 69.4 |
Of the total 83.6% males and 80.7% females had no prosthesis of upper arch, as compared to 88.3% males and 83.4% females who did not have prosthesis in the lower arch. The prosthetic status has been described in [Table/Fig-3]. Prosthetic treatment need was also compared between upper and lower jaws and the findings showed that 37.3% of the study participants did not require any prosthesis, 41.0% required combination of one and or multi-unit prosthesis and 5.4% needed full prosthesis in upper arch. In the lower arch 39.7% of participants did not require any prosthesis and 39.5% required combination of one and or multi-unit prosthesis. Statistically significant difference was also found in between different sexes and prosthetic treatment needs in lower jaw (p=0.057) [Table/Fig-4].
Prosthetic status in upper and lower jaws among study subjects.
| Prosthetic status | Male | Female | Total |
|---|
| n | % | n | % | n | % |
|---|
| Prosthetic status-upper jaw | No prosthesis present | 178 | 83.6 | 263 | 80.7 | 441 | 81.8 |
| Any prosthesis present | 35 | 16.4 | 63 | 19.3 | 98 | 18.2 |
| Prosthetic status- lower jaw | No prosthesis present | 188 | 88.3 | 272 | 83.4 | 460 | 85.3 |
| Any prosthesis present | 25 | 11.7 | 54 | 16.6 | 79 | 14.7 |
Prosthetic need in upper and lower jaw among study subjects.
| Prosthetic status | Gender | Total |
|---|
| Male | Female |
|---|
| n | % | n | % | n | % |
|---|
| Prosthetic needs-upper jaw | No prosthesis needed | 90 | 42.3 | 111 | 34.0 | 201 | 37.3 |
| Need for one unit prosthesis | 25 | 11.7 | 27 | 8.3 | 52 | 9.6 |
| Need for multi-unit prosthesis | 12 | 5.6 | 17 | 5.2 | 29 | 5.4 |
| Need for combination of one and or multi-unit prosthesis | 75 | 35.2 | 146 | 44.8 | 221 | 41.0 |
| Need for full prosthesis | 9 | 4.2 | 20 | 6.1 | 29 | 5.4 |
| Not recorded | 2 | 0.9 | 5 | 1.5 | 7 | 1.3 |
| Prosthetic needs –lower jaw | No prosthesis needed | 90 | 42.3 | 124 | 38.0 | 214 | 39.7 |
| Need for one unit prosthesis | 28 | 13.1 | 26 | 8.0 | 54 | 10.0 |
| Need for multi-unit prosthesis | 8 | 3.8 | 11 | 3.4 | 19 | 3.5 |
| Need for combination of one and or multi-unit prosthesis | 79 | 37.1 | 134 | 41.1 | 213 | 39.5 |
| Need for full prosthesis | 6 | 2.8 | 26 | 8.0 | 32 | 5.9 |
| Not recorded | 2 | 0.9 | 5 | 1.5 | 7 | 3 |
The OHIP -14 was assessed among the study subjects and overall mean of 0.86 and standard deviation of 0.34 was found. Majority of the study subjects never had much of impact due to oral health problems on the quality of life [Table/Fig-5]. The OHIP scores for the prosthetic needs of upper and lower jaw were statistically analysed and found that there was a statistically significant difference between various OHIP components along with the prosthetic needs of both jaws (p=0.001) [Table/Fig-6,7].
Distribution of study subjects using OHIP-14.
| OHIP-14 Items | Distribution of responses (%) | Mean | Std. Deviation |
|---|
| Always | Sometimes | Never |
|---|
| Have you had trouble pronouncing any words because of problems with your teeth, mouth or dentures? | 1.9 | 10.8 | 87.4 | 0.86 | 0.401 |
| Have you felt that your sense of taste has worsened because of problems with your teeth, mouth or dentures? | 2.0 | 23.4 | 74.6 | 0.73 | 0.490 |
| Have you had any painful aching in your mouth? | 3.0 | 35.1 | 61.8 | 0.59 | 0.552 |
| Have you found it uncomfortable to eat any foods because of problems with your teeth, mouth or dentures? | 3.0 | 25.8 | 71.2 | 0.68 | 0.526 |
| Have you felt self-conscious because of problems with your teeth, mouth or dentures? | 1.1 | 8.7 | 90.2 | 0.89 | 0.346 |
| Have you felt tense because of problems with your teeth, mouth or dentures? | 0.2 | 8.7 | 91.1 | 0.91 | 0.294 |
| Has your diet been unsatisfactory because of problems with your teeth, mouth or dentures? | 0.9 | 14.1 | 85.0 | 0.84 | 0.391 |
| Have you had to interrupt meals because of problems with your teeth, mouth or dentures? | 1.3 | 11.1 | 87.6 | 0.86 | 0.380 |
| Have you found it difficult to relax because of problems with your teeth, mouth or dentures? | 0.4 | 5.9 | 93.7 | 0.93 | 0.264 |
| Have you been a bit embarrassed because of problems with your teeth, mouth or dentures? | 0.6 | 1.9 | 97.6 | 0.97 | 0.200 |
| Have you been a bit irritable with other people because of problems with your teeth, mouth or dentures? | 0.0 | 3.0 | 97.0 | 0.97 | 0.170 |
| Have you had difficulty doing your usual jobs because of problems with your teeth, mouth or dentures? | 0.9 | 3.0 | 96.1 | 0.95 | 0.254 |
| Have you been totally unable to function because of problems with your teeth, mouth or dentures? | 0.9 | 4.1 | 95.0 | 0.94 | 0.273 |
| Have you felt that life in general was less satisfying because of problems with your teeth, mouth or dentures? | 0.7 | 2.4 | 96.8 | 0.96 | 0.229 |
Multiple comparison of of OHIP-14 and upper prosthetic need of study subjects.
| OHIP-14 components | Upper prosthetic need | Mean | Std. Deviation |
|---|
| Functional Limitation | No prosthesis | 0.80 | 0.05 |
| One unit prosthesis | 0.83 | 0.02 |
| Multi-unit prosthesis | 0.88 | 0.02 |
| Combination of one and multi-unit prosthesis | 0.72 | 0.19 |
| Full prosthesis | 0.59 | 0.02 |
| Total | 0.76 | 0.12 |
| Physical pain | No prosthesis | 0.74 | 0.00 |
| One unit prosthesis | 0.63 | 0.07 |
| Multi-unit prosthesis | 0.69 | 0.00 |
| Combination of one and multi-unit prosthesis | 0.49 | 0.14 |
| Full prosthesis | 0.44 | 0.02 |
| Total | 0.60 | 0.13 |
| Psychological discomfort | No prosthesis | 0.90 | 0.02 |
| One unit prosthesis | 0.96 | 0.00 |
| Multi-unit prosthesis | 0.88 | 0.07 |
| Combination of one and multi-unit prosthesis | 0.87 | 0.00 |
| Full prosthesis | 0.85 | 0.04 |
| Total | 0.89 | 0.04 |
| Physical disability | No prosthesis | 0.85 | 0.00 |
| One unit prosthesis | 0.89 | 0.01 |
| Multi-unit prosthesis | 0.76 | 0.00 |
| Combination of one and multi-unit prosthesis | 0.83 | 0.02 |
| Full prosthesis | 0.75 | 0.00 |
| Total | 0.81 | 0.05 |
| Psychological disability | No prosthesis | 0.94 | 0.03 |
| One unit prosthesis | 0.97 | 0.01 |
| Multi-unit prosthesis | 1.00 | 0.00 |
| Combination of one and multi-unit prosthesis | 0.94 | 0.05 |
| Full prosthesis | 0.93 | 0.00 |
| Total | 0.95 | 0.03 |
| Social handicap | No prosthesis | 0.94 | 0.00 |
| One unit prosthesis | 0.98 | 0.02 |
| Multi-unit prosthesis | 1.00 | 0.00 |
| Combination of one and multi-unit prosthesis | 0.96 | 0.02 |
| Full prosthesis | 0.89 | 0.09 |
| Total | 0.95 | 0.05 |
| Handicap | No prosthesis | 0.92 | 0.00 |
| One unit prosthesis | 0.98 | 0.00 |
| Multi-unit prosthesis | 0.97 | 0.00 |
| Combination of one and multi-unit prosthesis | 0.96 | 0.02 |
| Full prosthesis | 0.87 | 0.07 |
| Total | 0.94 | 0.04 |
ANOVA between groups p =0.001
Multiple comparison of OHIP-14 and lower prosthetic need of study subjects.
| OHIP-14 components | Lower prosthetic need | Mean | Std. Deviation |
|---|
| Functional Limitation | No prosthesis | 0.80 | 0.05 |
| One unit prosthesis | 0.83 | 0.02 |
| Multi-unit prosthesis | 0.88 | 0.02 |
| Combination of one and multi-unit prosthesis | 0.72 | 0.19 |
| Full prosthesis | 0.59 | 0.02 |
| Total | 0.76 | 0.12 |
| Physical pain | No prosthesis | 0.74 | 0.00 |
| One unit prosthesis | 0.63 | 0.07 |
| Multi-unit prosthesis | 0.69 | 0.00 |
| Combination of one and multi-unit prosthesis | 0.49 | 0.14 |
| Full prosthesis | 0.44 | 0.02 |
| Total | 0.60 | 0.13 |
| Psychological discomfort | No prosthesis | 0.90 | 0.02 |
| One unit prosthesis | 0.96 | 0.00 |
| Multi-unit prosthesis | 0.88 | 0.07 |
| Combination of one and multi-unit prosthesis | 0.87 | 0.00 |
| Full prosthesis | 0.85 | 0.04 |
| Total | 0.89 | 0.04 |
| Physical disability | No prosthesis | 0.85 | 0.00 |
| One unit prosthesis | 0.89 | 0.01 |
| Multi-unit prosthesis | 0.76 | 0.00 |
| Combination of one and multi-unit prosthesis | 0.83 | 0.02 |
| Full prosthesis | 0.75 | 0.00 |
| Total | 0.81 | 0.05 |
| Psychological disability | No prosthesis | 0.94 | 0.03 |
| One unit prosthesis | 0.97 | 0.01 |
| Multi-unit prosthesis | 1.00 | 0.00 |
| Combination of one and multi-unit prosthesis | 0.94 | 0.05 |
| Full prosthesis | 0.93 | 0.00 |
| Total | 0.95 | 0.03 |
| Social handicap | No prosthesis | 0.94 | 0.00 |
| One unit prosthesis | 0.98 | 0.02 |
| Multi-unit prosthesis | 1.00 | 0.00 |
| Combination of one and multi-unit prosthesis | 0.96 | 0.02 |
| Full prosthesis | 0.89 | 0.09 |
| Total | 0.95 | 0.05 |
| Handicap | No prosthesis | 0.92 | 0.00 |
| One unit prosthesis | 0.98 | 0.00 |
| Multi-unit prosthesis | 0.97 | 0.00 |
| Combination of one and multi-unit prosthesis | 0.96 | 0.02 |
| Full prosthesis | 0.87 | 0.07 |
| Total | 0.94 | 0.04 |
ANOVA between groups p= 0.001
Discussion
Of the total 16.5% of the subjects (18.2% and 14.7% respectively in the upper and lower jaws) presented with one prosthesis or the other, which was better compared to the value of 15.6% [6]. The prevalence of bridge prosthesis in the upper and lower arches was 2% and 0.5% respectively in the study population, which could be directly reflected in the values by Luan WM [7] and Prasad KVV [8]. However, complete denture wearers comprised 11.1% of the edentulous population.
The prosthetic need of the upper jaw was slightly more (62.7%) compared to that of the lower jaw (60.3%), which was contrary to the DCI National Oral Health survey conducted in 2004 [9]. However, the total prosthetic needs were on par with those obtained in the studies of Mann J [10] and Shetty VD et al., [11]. The high prosthetic need among these elderly may be attributed to their old age. Reduced salivary flow rate, fluctuations in its quality and quantity, impaired immunity and thus, the reduced ability of the body to repair itself may aggravate the processes of degradation of the oral tissues resulting in edentulous individuals.
We observed that the prosthetic need was huge and this was a consequence of lack of primary and secondary dental care. Prosthetic rehabilitation is expensive and unaffordable for the geriatric population. Prosthetic needs add burden on the already existing health burden on them. Therefore, government policies should be in place to provide rehabilitative care for the elderly.
OHRQOL: The various domains of the prosthetic need, being a part of normative need expressed an impact on the OHRQOL. Of all the domains, the domain of physical pain was most affected by the non-usage of dentures. Values of pain and discomfort were evident due to the lack of dentures. The various questions measuring OHRQOL, including the OHIP-14, provides an insight into the patient perceived outcomes. The prosthetic needs of the population contradict their perceived needs obtained by OHRQOL. This arises due to the lack of awareness about the importance of teeth in oral functions and other issues related to general health. Special emphasis lies on health education of the elderly public regarding the importance of prosthodontic rehabilitation.
On the nutritional aspect, as tooth loss occurs, the masticatory efficiency declines, and alteration in dietary intake happens to compensate for the greater difficulty of eating certain foods. Dietary fibres are being replaced by processed food items leading to deleterious effects on the body [12]. The increase in cholesterol levels and decrease in vitamins and minerals in the edentulous elderly has been well established [13].
The posterior edentulous conditions resulting from the loss of posterior teeth could result in alterations in the vertical dimension. A positive correlation between tooth loss and the loss of upper airway space has been established, resulting in edentulism being a prime reason for obstructive sleep apnea [14]. In addition, edentulism has also been associated with disturbances in the TMJ [15], as well as acceleration of age-related hearing loss [16].
The OHIP-14 questionnaire, being more psychologically directed measures less of oral functional needs. The questions are also considered to be more complex as far as the oral health scenario is expected. The tendency of giving nil values by the study population is another direct effect of this particular questionnaire.
Limitation
The aspect of socio-economic status was not considered in this study. Moreover, the significance of anterior and posterior edentulous spaces and aesthetics has not been established.
There in huge unmet prosthetic need in these elderly populations, which is similar elsewhere in India. The economic burden of the prosthetic need is enormous since the lack of social security measures. Moreover, there is also lack of the appreciation of the OHRQOL with existing prosthetic status may also impede to seek care. The programs and polices should be place for geriatric dental care. Prosthetic needs add burden on the already existing health burden on them. Therefore, government policies should be in place to provide rehabilitative care for the elderly.
Conclusion
The prosthetic status of the upper and lower jaws were 18.2% and 14.7% respectively for the study population and the prosthetic needs of the upper and lower jaws were 62.7% and 60.3% respectively for the study population. The prosthetic status had no impact on the OHRQOL of the study population. However, the maxillary and mandibular prosthetic need was significantly related to the individual domains of OHRQOL of the study population and of all the domains in OHRQOL, physical pain was the most affected in the study population. The prosthetic need deciphered was huge and this was a consequence of lack of primary and secondary dental care. Prosthetic rehabilitation is expensive and unaffordable for the geriatric population.
Funding: This research was supported by the research funding of Amrita Vishwa Vidyapeetham University, India.
ANOVA between groups p =0.001
ANOVA between groups p= 0.001