A Case of Sialolithiasis in a Minor Salivary Gland of the Buccal Mucosa
Masashi Kimura1, Atsushi Enomoto2, Akio Shibata3, Shusuke Nishiwaki4, Masahiro Umemura5
1 Attending Staff, Department of Oral and Maxillofacial Surgery, Ogaki Municipal Hospital, Ogaki, Gifu, Japan.
2 Associate Professor, Department of Pathology, Nagoya University Graduate School of Medicine, Showa-ku, Nagoya, Japan.
3 Attending Staff, Department of Oral and Maxillofacial Surgery, Ogaki Municipal Hospital, Ogaki, Gifu, Japan.
4 Senior Resident, Department of Oral and Maxillofacial Surgery, Ogaki Municipal Hospital, Ogaki, Gifu, Japan.
5 Director, Department of Oral and Maxillofacial Surgery, Ogaki Municipal Hospital, Ogaki, Gifu, Japan.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Masashi Kimura, Department of Oral and Maxillofacial Surgery, Ogaki Municipal Hospital, 4-86 Minaminokawa, Ogaki, Gifu 503-8502, Japan.
E-mail: masashi.kimura009@gmail.com, masashi9@dpc.agu.ac.jp
Sialolithiasis is a common disease of the major salivary glands. In contrast, Sialolithiasis of Minor Salivary Glands (SMSG) is very rare. Only 2% of all cases of sialolithiasis develop in minor salivary glands and sublingual glands. Furthermore, the clinical and imaging features of SMSG frequently differ from those encountered in major salivary glands thus, hindering proper clinical diagnosis of SMSG. Histologically, SMSG is characterized by ductal ectasia (sometimes with deep cystic dilatation), acinar atrophy and periductal inflammation. Herein, we describe a patient suffering from SMSG in the left buccal region. Based on the clinicopathological findings of this case and a review of the literature, we propose that this entity should be included in the differential diagnosis of intra-mucosal nodules.
Diagnosis, Pathology, Salivary gland calculi
Case Report
A 60-year-old Japanese male presented to Department of Oral and Maxillofacial Surgery, complaining of a mass on the left side of the buccal mucosa. He first noticed the painless mass a week ago. Intra-oral examination revealed a well-circumscribed mass (30mm×15mm) on the left buccal region, covered by a slightly reddish mucosa containing a small fistula. The lesion did not involve the parotid papilla. On palpation, the lesion was hard, non-tender and immobile. Computed Tomography (CT) revealed a well-defined mass of soft tissue in the left buccal region, with no apparent calcification [Table/Fig-1a]. Fine-Needle Aspiration Cytology (FNAC) of the lesion was performed to yield cellular smears. Papanicolaou and May Giemsa smear staining revealed a cystic background with mixed inflammatory cells. The volume of the lesion decreased after fine needle aspiration. Ultrasonography (USG) examination of the left buccal region indicated a hypoechoic mass (12mm×12mm×5mm) with heterogeneous internal echoes. The border was irregular, and no calcification was observed [Table/Fig-1b]. A provisional diagnosis of a minor salivary gland tumour was established, which warranted an excisional biopsy of the lesion under local anaesthesia [Table/Fig-1c]. There was no evidence of recurrent disease during the follow-up period.
(a) Computed tomography showing a well-defined soft tissue mass (arrowhead) without calcification; (b) Ultrasound observations revealed a hypoechoic mass (12mm×12mm×5mm) with heterogeneous internal echoes. The border was irregular and without calcification; (c) Pre-operative view. The arrowheads indicate the mass and the arrow indicate the small fistula; (d) Histopathological examination revealed heterogeneous lamellated calculi (asterisk) within the lumen of a dilated minor salivary duct (arrowhead) (H&E, 40×). Part of the epithelial lining of the dilated duct revealed squamous metaplasia; (e) The duct exhibits squamous metaplasia (H&E, 200×); (f) The cyst-like lumen contained mucin and was obstructed by a sialolith. The epithelial lining of the dilated duct had papillary projections towards the duct lumen (H&E, 40×).
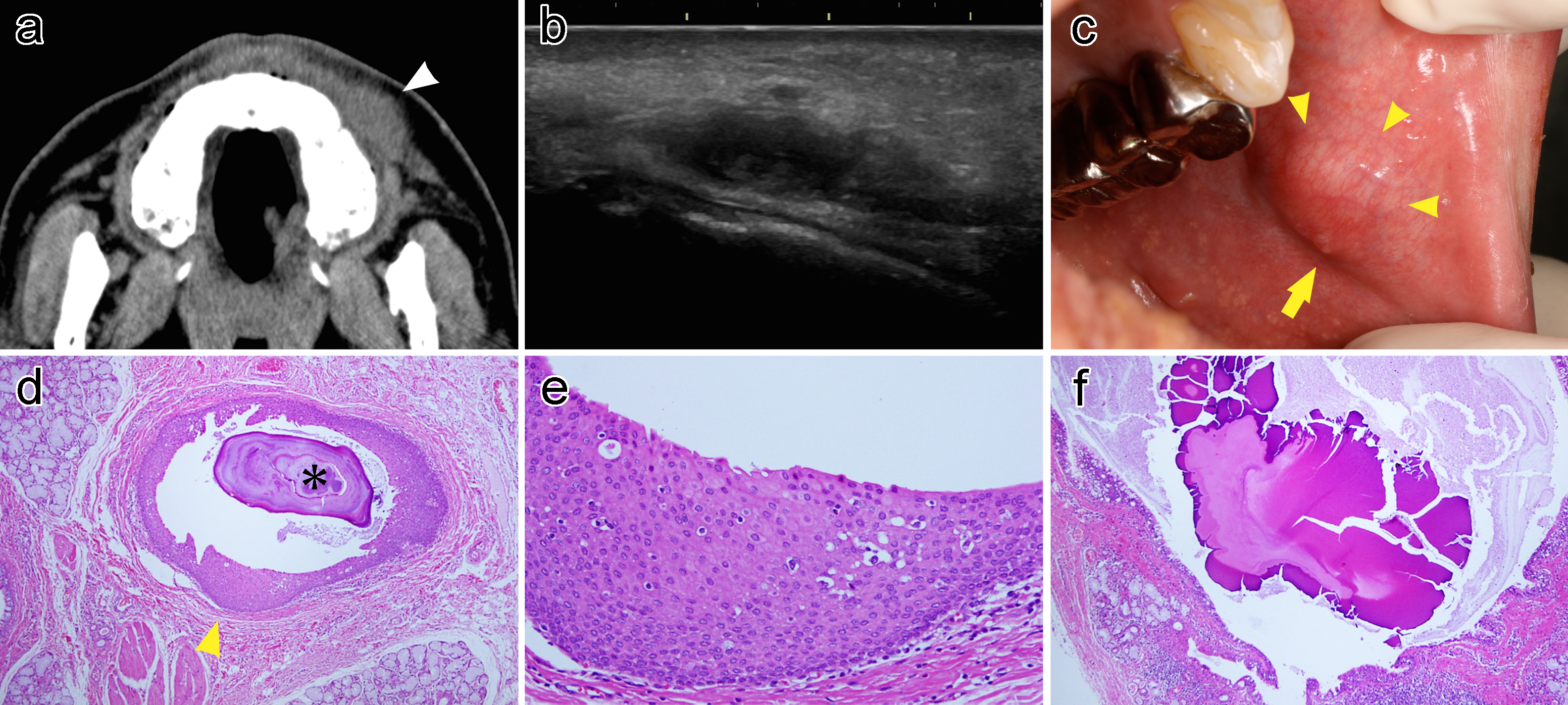
Histopathological examination revealed heterogeneous lamellated calculi within the lumen of a dilated minor salivary duct [Table/Fig-1d]. Part of the epithelial lining of the dilated duct revealed squamous metaplasia and papillary projections towards the duct lumen [Table/Fig-1e,f]. The cyst-like lumen contained mucin and was obstructed by a sialolith [Table/Fig-1f]. Based on these findings, the patient was diagnosed with mucous retention cysts due to ductal obstruction by sialolithiasis.
Discussion
Sialolithiasis is a common disease of the major salivary glands leading to duct obstruction, inflammation and/or painful infection. On the other hand, Sialolithiasis of Minor Salivary Gland (SMSG) is rare [1]. Ben Lagha et al., reported that only 2% of the cases of sialolithiasis develop in minor salivary glands and sublingual glands [2]. The most frequent sites for SMSG are the buccal mucosa and upper lip [3]; followed by the lower lip, vestibule, retromolar space, palate, tongue and floor of mouth [3–5]. Most reported cases were on average older than 45 years old [3,4,6,7], suggesting that ageing-related metaplastic changes in ductal cells and saliva may contribute to sialolith formation. However, the aetiology of sialoliths remains unclear and may be multifactorial [1,4]. The formation of sialoliths was suggested to involve two distinct phases [2]. During the first phase, irritant factors, such as inflammation of the inner layer of the canaliculi, saliva acidosis or hypoptyalism would trigger spasmodic contractions of the canaliculi and salivary stasis. The second phase is physicochemical, which leads to the development of calculus [2].
Clinically, SMSG typically appears as a single, small, round, submucosal asymptomatic nodule, which is hard or firm and moves freely in the surrounding tissue [1–3,6,8]. A sialolith-associated fistula is not uncommon [8]. But contrary to sialolithiasis of major salivary glands, the clinical features of SMSG have considerable variability. For instance, some sialoliths may be invisible on X-ray photographs [2]. In addition, spontaneous avulsion of the calculus has been reported. Therefore, an accurate clinical diagnosis of SMSG is difficult. Previous studies indicated that the rate of consistency between clinical and histopathological diagnosis is 0%–20% [3,4,6,7]. The most frequent misdiagnoses are fibroma, mucocele, tumour of the salivary gland, non-specific sialadenitis, oral cancer and oral pre-cancerous lesions [3,4]. During X-rays, low-dose intra-oral radiography may improve the detection of possible radiopaque lesions [1–3]. Although a previous study suggested that CT and USG might play a role in identifying sialoliths [1], these imaging modalities could not detect the calcification in the present case. If sialoliths in minor salivary glands cannot be detected by imaging, surgical excision is the preferred option to confirm the diagnosis. Nonetheless, a differential diagnosis of the radiopaque lesion should be performed to rule out calcified lymph nodes, phleboliths, tuberculosis of lymph nodes and other vascular calcifications [1].
Histologically, SMSG is characterized by ductal ectasia (sometimes with deep cystic dilatation), acinar atrophy and periductal inflammation. These histological findings must be considered in distinguishing cases of mucous metaplasia from low-grade mucoepidermoid carcinoma or cases of cystic dilatation due to a cystadenoma [4]. Thus, alterations surrounding ductal epithelium are significant factors to be considered in the diagnosis. Therefore, the first-line treatment of SMSG should be complete surgical excision, including that of the sialolith and the gland involved, after which recurrence is rarely reported [4,6].
Conclusion
In conclusion, the frequency of SMSG may be under-estimated because this lesion is often clinically misdiagnosed. The clinical and histopathological SMSG presented herein suggest that this entity should be included in the differential diagnosis of intra-mucosal nodules.
[1]. Lee LT, Wong YK, Pathogenesis and diverse histologic findings of sialolithiasis in minor salivary glandsJ Oral Maxillofac Surg 2010 68:465-70. [Google Scholar]
[2]. Ben Lagha N, Alantar A, Samson J, Chapireau D, Maman L, Lithiasis of minor salivary glands: Current dataOral Surg Oral Med Oral Pathol Oral Radiol Endod 2005 100:345-48. [Google Scholar]
[3]. Wang W-C, Chen C-Y, Hsu H-J, Kuo J-H, Lin L-M, Chen Y-K, Sialolithiasis of minor salivary glands: A review of 17 casesJ Dent Sci 2016 11:152-55. [Google Scholar]
[4]. Brazao-Silva MT, Prosdocimi FC, Lemos-Junior CA, de Sousa S, Clinicopathological aspects of 25 cases of sialolithiasis of minor salivary glandsGen Dent 2015 63:e22-26. [Google Scholar]
[5]. Jain A, Bohara P, Gandhi R, Dawer M, Jain CD, An unusual and rare presentation of sialolith on inferolateral part of soft palateInt J Adv Health Sci 2015 2:5-8. [Google Scholar]
[6]. Anneroth G, Hansen LS, Minor salivary gland calculi. A clinical and histopathological study of 49 casesInt J Oral Surg 1983 12:80-89. [Google Scholar]
[7]. Pullon PA, Miller AS, Sialolithiasis of accessory salivary glands: Review of 55 casesJ Oral Surg 1972 30:832-34. [Google Scholar]
[8]. Souza IF, Kawatake MM, Soares AB, Moraes PdC, Araújo VCD, Passador-santos F, Sialolithiasis of minor salivary glandsRev Gaúch Odontol 2015 63:63-68. [Google Scholar]