Non-Surgical Management of Teeth with Wide Open Apices and Large Periapical Lesions: A Conservative Reality
Sarang Sharma1, Shibani Grover2, Pooja Dudeja3, Vivek Sharma4, Deepak Passi5
1 Associate Professor, Department of Conservative Dentistry and Endodontics, ESIC Dental College and Hospital, Delhi, India.
2 Professor, Department of Conservative Dentistry and Endodontics, ESIC Dental College and Hospital, Rohini, Delhi, India.
3 Associate Professor, Department of Conservative Dentistry and Endodontics, ESIC Dental College and Hospital, Delhi, India.
4 Assistant Professor, Department of Conservative Dentistry and Endodontics, ESIC Dental College and Hospital, Delhi, India.
5 Tutor, Department of Oral and Maxillofacial Surgery, ESIC Dental College and Hospital, Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sarang Sharma, Associate Professor, Department of Conservative Dentistry and Endodontics, ESIC Dental College and Hospital, Rohini-110085, Delhi, India.
E-mail: sarang74in@gmail.com
Apexification, Mineral trioxide aggregate, Open apex, Periapical cyst, Platelet rich fibrin
Case-1
A 26-year-old male visited the Department of Conservative Dentistry and Endodontics after referral from Oral Surgery for opinion regarding maxillary right lateral incisor. Diagnosis established in Oral Surgery was of an infected cyst in relation to tooth #12 and the treatment suggested was enucleation and curettage. Patient’s dental history revealed anterior trauma at 10 years of age and his chief complaint was found to be recurrent swelling and pus discharge in relation to maxillary right anteriors for the past 1-2 years. Clinical examination revealed a discolored tooth #12 [Table/Fig-1a] and sinus opening within an erythematous area measuring 0.5cm on the palate [Table/Fig-1b]. On palpation, the palatal region had a paper like soft consistency. Thermal and electrical pulp testing elicited no response in tooth #12 but positive responses in both tooth #11 and tooth #13. Pre-operative radiograph revealed a large radiolucency approximately 15mmX15mm, involving tooth #12, and extending up till teeth #11 and #13 [Table/Fig-1c]. Tooth #12 showed large canal space, open root apex, and ragged irregular margins at the apex suggesting inflammatory external resorption. We decided to treat tooth #12 conservatively and include surgical intervention, only if deemed necessary.
(a) Clinical view showing discolored right lateral incisor; (b) Clinical view showing erythematous area and sinus traced with gutta percha; (c) Intra-oral periapical radiograph showing periapical radiolucency measuring approximately 15mm x 15mm and involving tooth #12 and extending up till teeth #11 and #13; (d) Post-operative periapical radiograph demonstrating complete MTA plug created after placing preliminary PRF barrier; (e) Intra-coronal bleaching performed in maxillary right lateral incisor and (f) Radiographic examination at one year revealed healing lesion with trabeculae formation seen within the lesion.
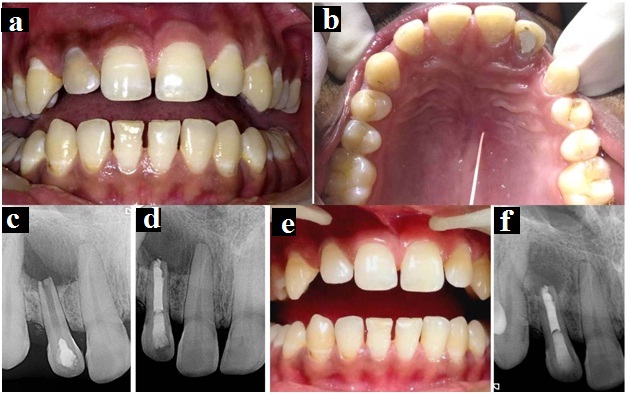
Under rubber dam isolation, access cavity was prepared in tooth # 12 and intracanal aspiration was performed, with simultaneous digital pressure being applied from the palatal side. Canal walls were lightly instrumented with No. 80 H-file under copious irrigation with 20 volumes of 3% sodium hypochlorite. No. 80 K-file was extended 1-2mm beyond the confines of the root apex during instrumentation to break the cystic lining, if any. After a final rinse with 2% chlorhexidine, the canal was dried thoroughly and an intra-canal medicament of calcium hydroxide was placed for two weeks. Subsequently, two dressings of triple antibiotic paste (ciprofloxacin 500mg, metronidazole 400mg and minocyclin 100mg mixed with normal saline) were given for 15 days each. On fourth endodontic visit, the patient was totally asymptomatic. The root canal was thoroughly irrigated and dried to receive a preliminary plug of Platelet Rich Fibrin (PRF) followed by Mineral Trioxide Aggregate (MTA) placement. A finger plugger (Dentsply Caulk, Milford, DE, USA) was selected to fit 1.5mm short of the root apex. On receiving the centrifuged blood sample, PRF gel was separated from Red Blood Cell (RBC) fraction and squeezed between layers of moist gauze to form a PRF membrane. It was cut into a size slightly larger than the size of the access cavity, introduced into the canal and carried till the apex with the selected plugger.
Following PRF barrier placement, white MTA (ProRoot, Maillefer, Dentsply, Switzerland) was mixed according to the manufacturer’s instructions and inserted into the canal using amalgam carrier. The canal was filled by incremental placement and condensation of MTA from apical to coronal end using endodontic finger pluggers [Table/Fig-1d]. Access cavity was temporarily sealed after placing moist cotton pellet over MTA. After one week, intra-coronal bleaching was performed to correct discoloration in tooth #12 [Table/Fig-1e]. Finally, the access cavity was permanently restored with bonded resin restoration. At one year, the patient continued to be asymptomatic and healing could be appreciated [Table/Fig-1f].
Case-2
Similar to Case 1, a 20-year-old female patient was referred from Department of Oral Surgery for opinion regarding maxillary left lateral incisor [Table/Fig-2a]. The patient was wearing a fixed prosthesis extending from tooth #13 till tooth #22, and for past two years was experiencing recurrent swelling and discharge in palatal region every 3-4 months.
(a) Facial clinical view showing patient wearing fixed prosthesis; (b) Intra-oral periapical radiograph demonstrating large radiolucency measuring approximately 18mm × 15 mm with respect to #22 and extending until the mesial aspect of #23; (c) Post-operative intraoral periapical radiograph immediately after preliminary PRF barrier and MTA placement and (d) At one year recall, healing lesion and a marked decrease in lesion size could be appreciated.
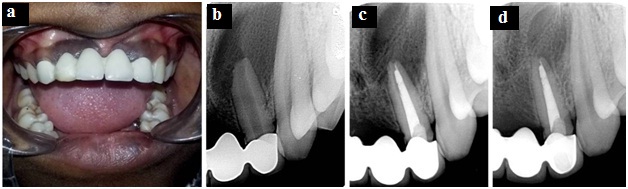
Pre-operative radiograph revealed a large radiolucency approxi-mately 18mm × 15mm with respect to tooth #22 and extending up till the mesial aspect of tooth #23 [Table/Fig-2b]. Tooth #22 showed a large canal space and an open root apex. It was decided to treat tooth #22 conservatively without removal of prosthesis. Under modified rubber dam technique, access cavity was prepared through the crown in tooth #22. Frank straw colored fluid discharge was seen from the canal. Further treatment rendered was similar to as in Case 1 [Table/Fig-2c]. At one year, patient continued to be asymptomatic and healing could be greatly appreciated [Table/Fig-2d].
Discussion
Successful use of conservative endodontic procedures while treating teeth with immature apices and cystic lesions in our patients could be explained by: (1) establishing a pathway for drainage and relief of cystic pressure; (2) thorough microbial elimination from the canal; (3) preventing microbial re-infection by ensuring three dimensional seal facilitated by PRF barrier and MTA; (4) supplementary healing by release of growth factors from PRF and (5) osteoinductive activity of MTA.
Lesions in both cases were suspected to be small radicular cysts henceforth an additional step advocated by Bhaskar was performed in which apical instrumentation exceeds 1-2mm beyond the apical foramen during root canal treatment [1]. Over instrumentation possibly relieves intra- cystic pressure by creating a pathway for drainage and simultaneously induces ulceration of the cystic epithelial lining and transient inflammation, resulting in cystic resolution [1,2]. Thorough microbial elimination is the key to any healing process. One well known reason for microbial persistence in teeth with open apices is compromised apical restorative seal when conventional endodontics is used. Apparently, in open apex canals where condensation of obturating material may not be properly achieved, establishing an artificial apical barrier against which filling material can be placed and thoroughly condensed is desirable.
Single visit apexification using calcium silicate materials for establishing an apical barrier is becoming quite popular as a conservative treatment option. Literature has invariably supported use of MTA in endodontics, owing to several desirable properties [3]. This is one material that has consistently shown overgrowth of cementoid and osteoid tissues with potential for periodontal fiber regeneration [4]. Here, MTA was used to fill the entire canal rather than limiting to formation of an apical plug. PRF, a fibrin matrix rich in platelets and cytokines served as a favourable preliminary barrier against which MTA could be contained and condensed [5]. PRF with its inherent healing potential coupled with osteoinductive property of MTA is definitely a suitable combination to generate cemental barrier and periodontal ligament attachment at the apex in addition to promoting periapical healing.
[1]. Bhaskar SN, Nonsurgical resolution of radicular cystsOral Surg Oral Med Oral Pathol 1972 34(3):458-68. [Google Scholar]
[2]. Bender IB, Commentary on General Bhaskar’s hypothesisOral Surg Oral Med Oral Pathol 1972 34:469-76. [Google Scholar]
[3]. Fernandes M, de Ataide I, Nonsurgical management of a large periapical lesion associated with an immature tooth displaying external inflammatory resorptionJ Conserv Dent 2015 18:349-53. [Google Scholar]
[4]. Torabinejad M, Pitt Ford TR, McKendry DJ, Abedi HR, Miller DA, Kariyawasam SP, Histologic assessment of mineral trioxide aggregate as a root-end filling in monkeysJ Endod 1997 23:225-28. [Google Scholar]
[5]. Dohan DM, Choukroun J, Diss A, Dohan SL, Dohan AJ, Mouhyi J, Platelet-Rich Fibrin (PRF): A second generation platelet concentrate. Part II: Platelet-related biologic featuresOral Surg Oral Med Oral Pathol Oral Radiol Endod 2006 101:e45-50. [Google Scholar]