Job’s syndrome or Hyperimmunoglobulin E Syndrome (HIES) is a rare primary immunodeficiency with marked increase in serum immunoglobulin E (IgE) levels and eczematous dermatitis. Individuals with HIES share characteristic facial features, with many oral manifestations like retained deciduous teeth, fissured tongue, missing permanent tooth buds, recurrent oral candidiasis, oral mucosal and gingival lesions. Two forms of disease have been identified based on the defective gene as autosomal dominant form and autosomal recessive form. The therapeutic strategies are usually directed towards prevention and management of recurrent infections which are refractory to the conventional strategies. About 200 cases of HIES have been reported so far, in the present case report authors present the oral manifestations of a paediatric dental patient affected with HIES.
Hyperimmunoglobulin E syndrome, Immunoglobulin E, Recurrent infections
Case Report
A 12-year-old boy was referred to the Department of Pedodontics, with the chief complaint of multiple decayed teeth. Detailed physical examination by the Paediatrician revealed numerous skin abscesses and pruritic dermatitis on scalp, face, limbs and trunk. The nails were showing definitive koilonychia with no evidence of icterus, cyanosis, lymphadenopathy and pedal oedema.
Medical history revealed episodes of recurrent abscesses in different parts of the body, associated with recurrent fever, cough and episodes of haemoptysis with the pus culture showing positivity for Staphylococcus aureus. Computed Tomography (CT) scan report of thorax showed thick walled bronchiectatic cavities with air fluid level in outer segments of right upper lobe and post-basal segment of right lower lobe. Haematological examination revealed that the white blood cell count was 19240 cells/μL with 71% neutrophils, and an elevated eosinophils level at 12%. Haemoglobin level was at 8.9 gram% with haematocrit at 28.9%. The serum Immunoglobulin E (IgE) level showed elevation to 16,025 IU/ml with the other immunoglobulins at normal range except for the reduction in IgM level.
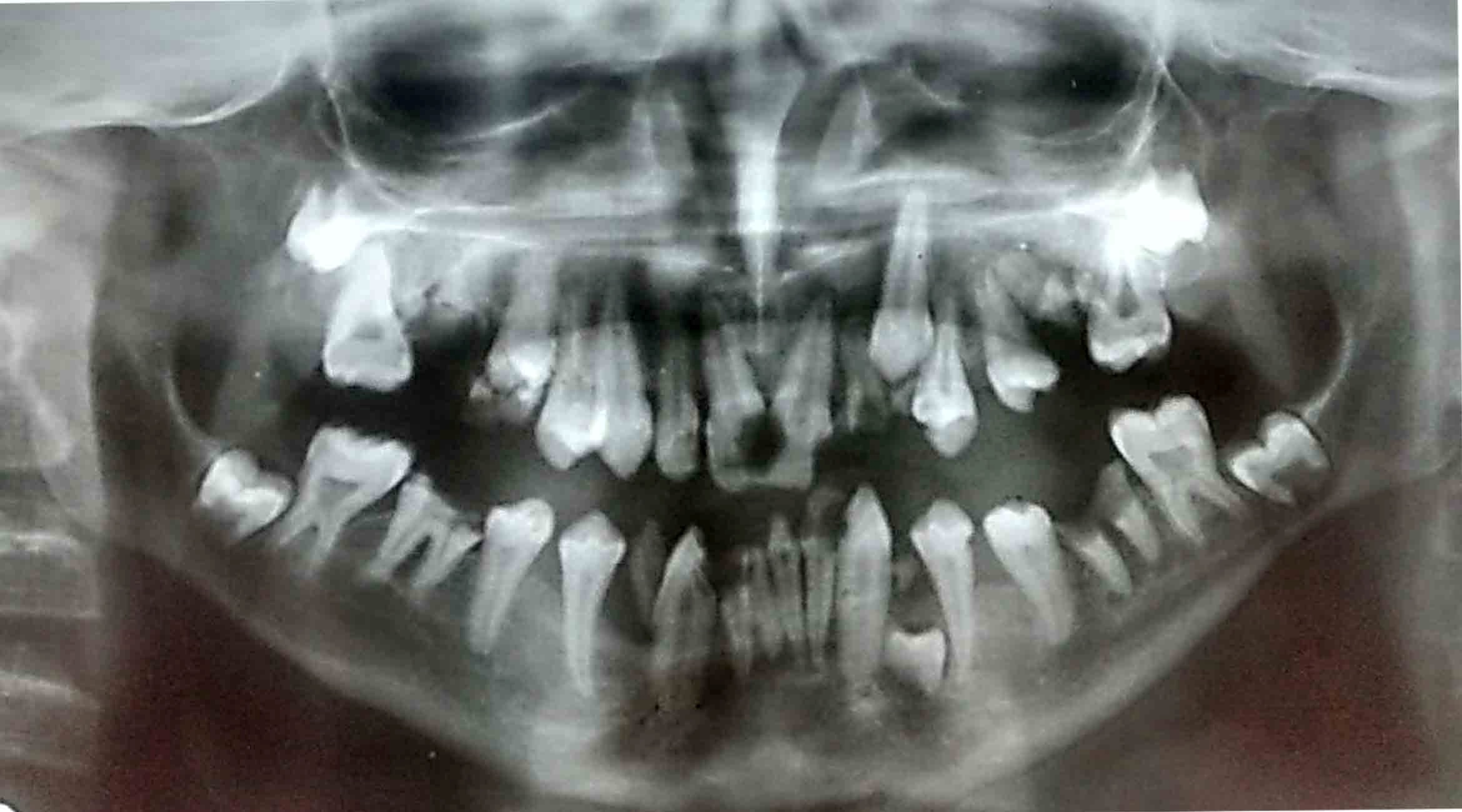
Facial and intra-oral examination revealed the characteristic coarse facial form, prominent forehead, rough facial skin, deep set wide spaced eyes, broad nasal bridge, wide fleshy nasal tip, Class III skeletal pattern, mild facial asymmetry with an old man appearance [Table/Fig-1]. Mild cervical lymphadenopathy, angular cheilitis, depapillation and fissuring of the tongue [Table/Fig-2], high arched palate, multiple keratotic/erosive areas on tongue and buccal mucosa, multiple non-specific ulcers on gingiva and poor oral hygiene were also noted. Dental examination revealed multiple carious lesions and root stumps of teeth # 52, 62, 71, 72, 81 and 82 with poor oral hygiene. Orthopantomogram (OPG) revealed absence of permanent tooth buds of teeth # 12, 22, 31, 32, 41, 42 and a supernumerary tooth in relation to tooth # 34 [Table/Fig-3]. Extraction of root stumps and necessary restorations were done to eliminate all infectious foci. The patient was referred back to the Department of Paediatrics for further evaluation.
Characteristic facial features, old man appearance with Class III skeletal pattern.

Angular cheilitis, depapillation and fissuring of tongue.

Orthopantamograph showing multiple carious lesions with absence of permanent succedaneous tooth buds of tooth number 12, 22, 31, 32, 41, 42 and a supernumerary tooth in relation to tooth number 34.
Discussion
The Hyperimmunoglobulin E Syndrome (HIES)/Job’s syndrome comprises of a group of primary immunodeficiency disorders mainly consisting of the classic triad of high serum IgE levels, eczema, skin and pulmonary infections [1]. Job’s syndrome was first described by Davis and colleagues (1966) in two sisters with a triad of eczematous dermatitis, recurrent sinopulmonary and staphylococcal skin infections that distinctly lacked warmth, erythema and tenderness [2]. In 1972, Buckley and colleagues further characterized this syndrome, reported distinctive facial features and an elevated levels of IgE and they termed the condition as Buckley’s syndrome [1,3].
Until 2007, till the drawing of two distinctive clinical patterns of the disease as Autosomal Dominant (AD) and Autosomal Recessive (AR) and their definitive aetiological patterns, this syndrome was remaining as a major immune deficiency of unknown genetic aetiology which leads to the associated immune dysfunction [3–5].
The AD form is found to be due to missense or in-frame deletions resulting in one amino acid change or loss in Signal Transducer and Activator of Transcription 3 (STAT3). In contrast to the aetiology of AD form, the occurrence of AR form is due to (Dedicator of Cytokinesis 8) DOCK 8 mutation [3].
It is clear that most of the patients affected with Job’s syndrome are having mutation in STAT 3 gene, even though not all, but in cases of AD disease pattern [4,5].
Although the initial presentation of the patients affected with AD pattern is high IgE levels, eczema and recurrent skin and lung infections, other immunologic and non-immunologic manifestations follows in the later span of life [1]. Various immunologic manifestations include; new born rash, eczema, boils, recurrent pneumonias, pneumatocoeles, mucocutaneous candidiasis, peak serum IgE, eosinophilia and an increased risk of lymphoma. Other non-immunologic manifestations include; retention of primary tooth, coarse facial features, minimal trauma fractures, scoliosis (>10 degrees), hyper-extensibility, oral mucosal and gingival abnormalities, hyper-intensities on brain Magnetic Resonance Imaging (MRI), Chiari I malformations, craniosynostosis and arterial aneurysms [3,6,7].
Patients affected with Job’s syndrome usually present with definitive oral manifestations including the failure of exfoliation of the primary tooth which in turn prevent the eruption of the succedaneous tooth. This can lead to impaction of the succedaneous tooth, or in case if the succedaneous tooth erupts lingual to the deciduous tooth it may result in the presence of double rows of teeth leading to subsequent malocclusion. Majority of the patients show a midline fibrotic bridge on the palate and a deep midline cleft anterior to the circumvallate papillae. The lips and cheek may show mucosal lesions consisting of surface fissures and non-scrapable keratotic striations, patches or plaques resembling lichenoid lesions. Oral candidiasis (pseudomembranous, erythematous, median rhomboid glossitis and angular cheilitis) is also a common manifestation [1,8,9]. This patient was presenting with the dental and oral mucosal abnormalities like retained primary teeth, tongue fissures, multiple ulcerative and keratotic lesions on the buccal mucosa, and most of the facial and morphological features which are associated with Job’s syndrome.
The initial treatment of HIES should focus on adequate skin care for controlling skin infections and eczema. It can be done with bleach bath and swimming in chlorinated pools, with topical corticosteroids, antibiotics and hydrating agents for eczema, which is coupled with antimicrobial prophylaxis against Staphylococcus aureus. In case of infections, intensive treatment must be administered against the organism cultured (most commonly Staphylococcus aureus). Other complications such as pulmonary empyema are common and if present are to be drained under proper antibiotic coverage. In patients with other rare severe complications, hematopoietic stem cell transplantation, administration of immunomodulators and plasma pheresis are used [1,3,10].
Conclusion
The oral manifestations of HIES are asymptomatic and non-immunologic which does not require an immediate intervention. The role of a dental specialist especially a Paediatric dentist is important in dealing with the oral lesions as they represent the early signs of the syndrome well ahead of the characteristic facial features and other immunologic manifestations. The prognosis of HIES patients depends on the early diagnosis and prompt management of the complications; hence, thorough knowledge about identifying the early oral manifestations of the disease is mandatory.
Declaration of the patient consent: The authors declare that they have obtained all necessary consent for using the patient images and details without revealing their identity for the publication process.
[1]. Freeman AF, Domingo DL, Holland SM, Hyper IgE (Job’s) syndrome: A primary immune deficiency with oral manifestationsOral Diseases 2009 15:2-7. [Google Scholar]
[2]. Davis SD, Schaller J, Wedgewood RJ, Job’s syndrome. Recurrent, “cold”, staphylococcal abscessesLancet 1966 1:1013-15. [Google Scholar]
[3]. Freeman AF, Holland SM, The hyper IgE syndromeImmunol Allergy Clin North Am 2008 28:277 [Google Scholar]
[4]. Holland SM, DeLeo FR, Elloumi HZ, Hsu AP, Uzel G, Broadsky N, STAT3 mutations in the hyper IgE syndromeNew England Journal of Medicine 2007 18:1608-19. [Google Scholar]
[5]. Minegishi Y, Saito M, Tsuchiya S, Tsuge I, Takada H, Hara T, Dominant negative mutations in DNA – binding domain of STAT3 cause hyper IgE syndromeNature 2007 448:1058-62. [Google Scholar]
[6]. Grimbacher B, Holland SM, Gallin JI, Greenberg F, Hill SC, Malech HL, Hyper IgE syndrome with recurrent infections-An autosomal dominant multisystem disorderN Engl J Med 1999 340:692-702. [Google Scholar]
[7]. Smithwick EM, Finelt M, Pahwa S, Good RA, Naspitz CK, Mendes NF, Cranial synostosis in Job’s syndromeLancet 1978 15:826 [Google Scholar]
[8]. Domingo DL, Freeman AF, Davis J, Puck JM, Tianxia W, Holland SM, Novel intraoral phenotypes in hyerimmunoglobulin E syndromeOral Diseases 2008 14:73-81. [Google Scholar]
[9]. O’Connell AC, Puck JM, Grimbacher B, Facchetti F, Majorana A, Gallin JI, Delayed eruption of permanent teeth in hyperimmunoglobulinemia E recurrent infection syndromeOral Surg Oral Med Oral Pathol Oral Radiol Endod 2000 89:177-85. [Google Scholar]
[10]. Cruz-Portelles A, Estopinan-Zuniga D, A new case of Job’s syndrome at the clinic: A diagnostic challengeRev Port Pneumol 2014 20(2):107-10. [Google Scholar]