Plasma Cell Gingivits-A Conflict of Diagnosis
Jammula Surya Prasanna1, Divya Aishwarya Mutyap2, Veerandranath Reddy Pantula3, Shilpa Akula4, Bhargavi Chinthapalli5
1 Professor, Department of Periodontics, Panineeya Institute of Dental Sciences and Research Centre, Hyderabad, Telangana, India.
2 Postgraduate Student, Department of Periodontics, Panineeya Institute of Dental Sciences and Research Centre, Hyderabad, Telangana, India.
3 Professor, Department of Periodontics, Panineeya Institute of Dental Sciences and Research Centre, Hyderabad, Telangana, India.
4 Postgraduate Student, Department of Periodontics, Panineeya Institute of Dental Sciences and Research Centre, Hyderabad, Telangana, India.
5 Postgraduate Student, Department of Periodontics, Panineeya Institute of Dental Sciences and Research Centre, Hyderabad, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Jammula Surya Prasanna, Professor, Panineeya Institute of Dental Sciences and Research Centre, Road No. 5, Kamalanagar, Dilsuck Nagar, Hyderabad-500060, Telangana, India.
E-mail: prasanna.parupalli@gmail.com
Plasma Cell Gingivitis (PCG) is a rare condition of the gingiva which is benign in nature. In this condition there is enlargement of the marginal and attached gingiva. It is not only unaesthetic in appearance but also causes difficulty in speech and mastication. Hence, it creates an area for plaque accumulation because of which there is difficulty in carrying out the routine oral hygiene procedures. The aetiology is unknown and is thought to be a hypersensitive reaction to an allergen. This condition is characterized by massive infiltration of the plasma cells into the sub-epithelial connective tissue layers. Here we are presenting two cases of PCG associated with swollen lips, which is an uncommon condition. These cases were treated by gingivectomy and followed up to six months.
Erythematous, Gingivectomy, Inflammation
Case Report
Two cases of gingival enlargement which were treated by gingi-vectomy are documented here.
Case-1
A 19-year-old female patient reported to the Department of Periodontics with a chief complaint of swollen lips and swollen gums. The patient had a Fixed Partial Denture (FPD) in relation to tooth # 11, 12, 21, 22, region which was done two years before. After two months of placing, she noticed a mild reddish discoloration involving both upper and lower lips, which progressively increased in size without any apparent discomfort but difficulty in maintaining closed lips in relaxed state. There was no association with pain but profuse bleeding on brushing was noted. Gingival swelling was also noticed at the same time. The patient had no reportable medical history. Clinically gingiva appeared fiery red in color, friable with oedematous consistency and smooth and shiny granular surface texture with exaggerated contour [Table/Fig-1]. Since all food allergens cannot be tested, suspected food allergens were tested. Investigations like skin prick test, trial elimination test was performed to rule out allergy due to food like brinjal, kenaf, cinnamon, sea foods, mushrooms and serum IgE levels were also examined. Food allergy and allergens could not be identified and hence, we thought of removing the FPD which was hindering the healing.
Case-1 pre-operative view.

Case-2
A 15-year-old male had a chief complaint of swollen gums which was unappealing and caused difficulty in speech and mastication. On conversation, patient gave history of allergy to sea food and brinjal, where the food was provoking the size of the gingival swelling but not regressing on removal of allergen. Patient also gave history of bleeding of gums on brushing. On clinical examination, enlarged marginal and attached gingiva was seen with exaggerated contour along with swollen lips [Table/Fig-2].
Case-2 pre-operative view.

The non-surgical periodontal therapy and surgical procedures like gingivectomy were described verbally to the patient and consent forms were signed. Blood investigations carried out included complete haemogram to differentiate other conditions which mimic the present condition, before surgery. Both the patients were otherwise systemically healthy. Based on clinical examination, provisional diagnosis of inflammatory gingival enlargement was given and the differential diagnosis including scorbutic gingivitis, Plasma Cell Gingivitis (PCG), acute leukaemia, plasmacytoma and myeloma were considered.
Treatment Procedure: In both the cases non-surgical periodontal therapy that is thorough oral prophylaxis with root planning was performed. Oral hygiene instructions were given and chemical plaque control was followed for 3-4 weeks until the inflammation subsided. Even after stringent elimination of possible allergens like chewing gums, cosmetics, food additives, change of regular tooth paste and known food which causes allergy there was no backsliding of the swelling. Hence, a surgical approach was planned for the gingival lesion. Biopsy specimens were sent for histopathological examination and gingivectomy was completed with electro-surgery [Table/Fig-3]. Coe-pak was placed and post- operative antibiotics and analgesics were prescribed. The cases were followed up at three months and six months which showed no signs of any recurrence of the enlargement.
Surgical excision of both cases, immediate after gingivectomy.

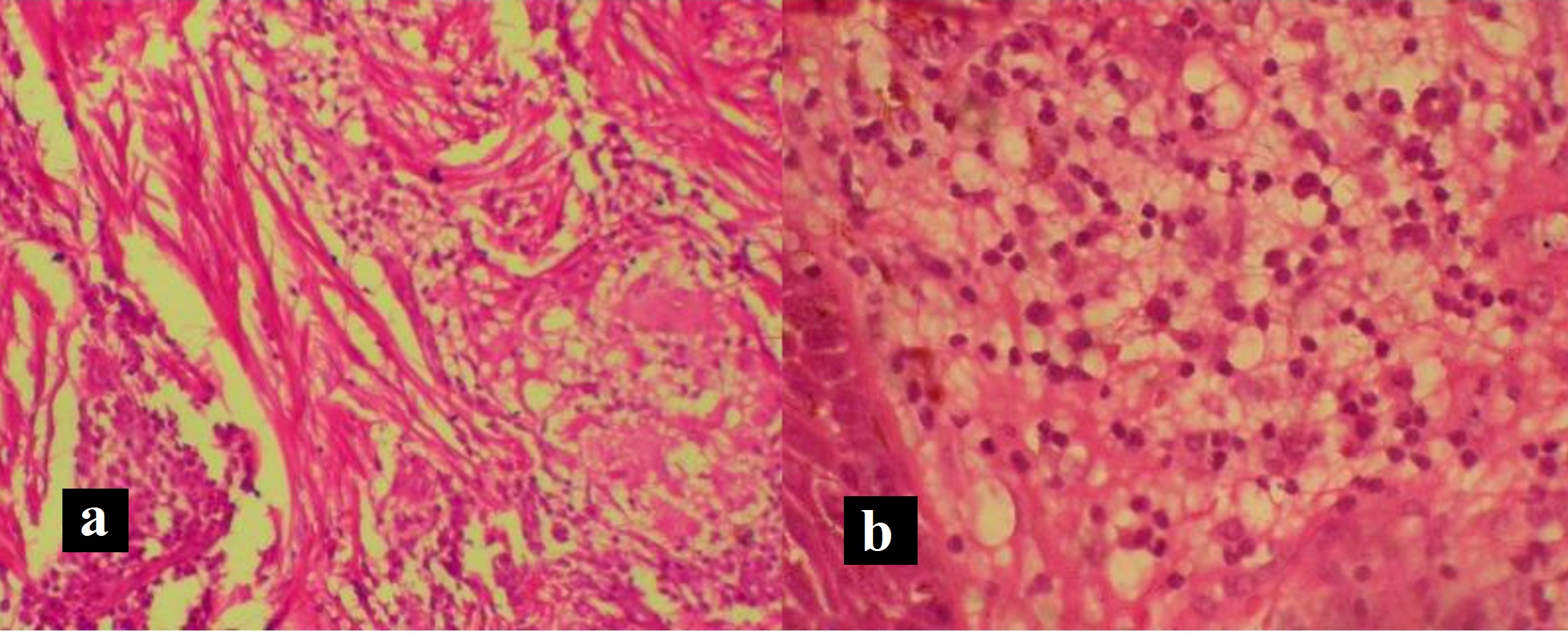
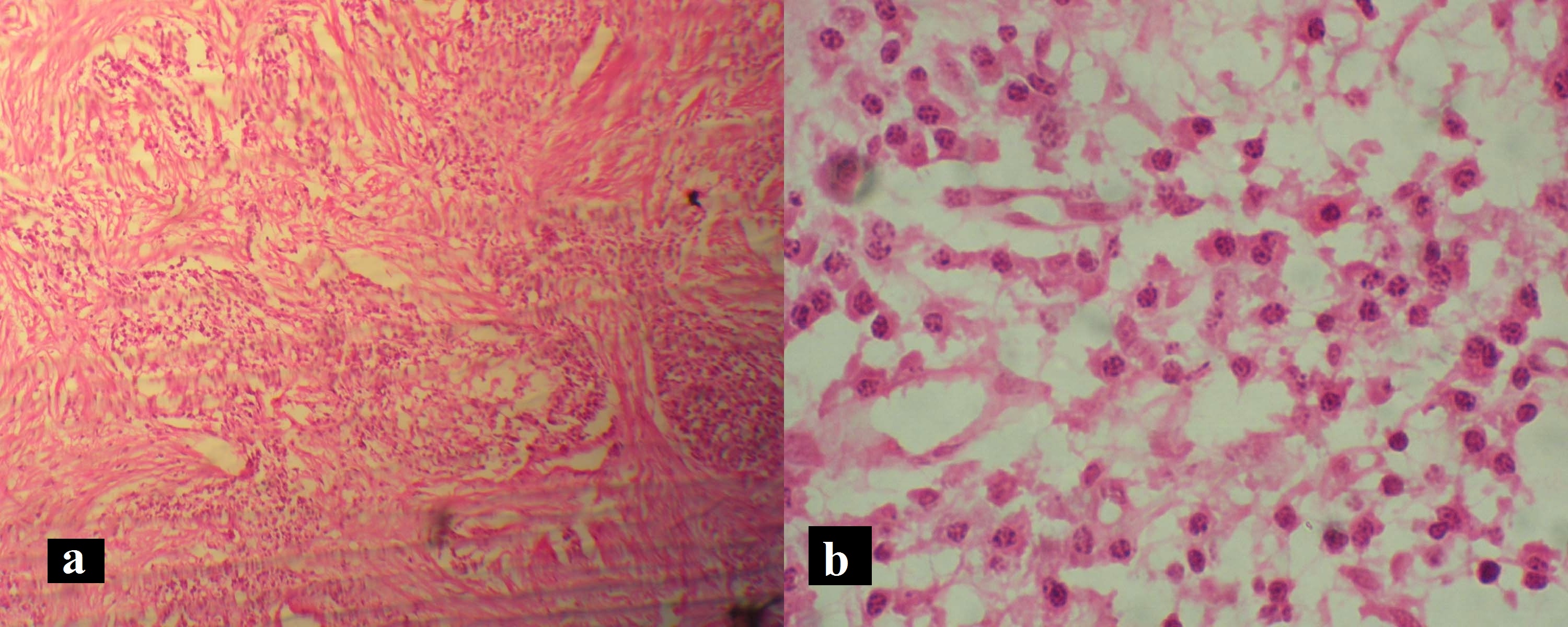
Histological Examination: Showed hyperplastic, spongiotic parakeratinized stratified squamous epithelium with areas of thin long rete ridges representing the classical psoriasiform pattern and pseudo-epitheliomatous hyperplasia. Leucocytic exocytosis and areas of neutrophilic micro-abscess were evident in the superficial layer. The lamina propria revealed extremely dense infiltration of chronic inflammatory cell infiltrate that was composed predominantly of plasma cells, few Russel bodies and numerous dilated vascular channels were consistently seen throughout the stroma [Table/Fig-4,5]. The histologic appearance was compatible with plasma cell gingivitis. Based on the histologic examination a diagnosis for PCG was made. Post-operative assessment was done after six months in both the cases [Table/Fig-6]. Excellent healing and proper contour was seen in Case-2. Post-operative results were satisfactory and there was no recurrence of the condition during follow-up period. The patient was under further follow-up care.
Case-1 (a) Biopsy comprised of dense plasma cells infiltrate in sub-epithelial connective tissue (H and E, ×100); (b) High power magnification revealing abundant plasma cells (H and E, ×400).
Case-2 (a) Biopsy comprised of leucocytic exocytosis (H and E, ×100); (b) High power magnification revealing abundant plasma cells with cart wheel appearance of the nucleus (H and E, ×400).
Case-1 post-operative view after 6 months (upper).
Case 2 post-operative view after 6 months (lower).

Discussion
There are many benign gingival disorders which involve both marginal and attached gingiva, one among them is PCG. In this condition the gingiva appears erythematous, edematous and sometimes granular. It generally does not induce loss of attachment. PCG is considered as a hypersensitive reaction to some antigen like chewing gum, dentrifices, various diet components and other foreign particles [1]. Cinnamon aldehyde and cinnamon which are used as ingredients in chewing gums and dentifrices are most commonly implicated as allergens, in which gingiva usually appears red, friable and bleeds easily.
A dense and huge infiltration of mature plasma cells in the lamina propria is the typical histopathological feature [2]. PCG is commonly known as allergic gingivostomatitis, idiopathic gingivostomatitis, plasmacytosis, and atypical gingivostomatitis [3]. It resembles histologically a multiple myeloma and plasmacytoma, clinically as acute leukemia. Antigenic identification is necessary for proper diagnosis of the condition along with clinical, histopathological and hematological screening. In contempt of imprecise allergy testing, finding exact allergen was unattainable [4].
PCG is a rare non-neoplastic condition, characterized by diffuse and massive infiltration of the plasma cells into the connective tissue. The first case was reported by Kerr et al., in 1971, where they found that gingival enlargement disappeared when gum chewers quit the habit of chewing [5].
PCG has been classified into three types in 1995 by Garguilo, as an immunological reaction to allergens, neoplasia and unknown origin [6]. Plasma cell granuloma also known as an inflammatory pseudotumor, inflammatory myofibroblastic tumor or xanthomatous pseudotumor is an uncommon non-neoplastic lesion used to describe an enlargement confined to one specific site [7]. Along with gingiva it also affects other organs like lungs, paranasal sinuses, reticuloendothelial system, orbit, ears, larynx, tonsils and lip. Apart from all these, gingiva is rarely involved [8]. Oedematous swelling with diffuse erythema clearly demarcated from mucogingival junction is a typical clinical presentation of PCG. In the present cases gingival enlargement was confined to upper and lower anterior segments which was fiery red in color, obstinate to oral prophylaxis. These findings are consistent with earlier reports [9–10]. This case is contradictory to the study by Arduino PG et al., who presented a series of PCG cases, which were downturn by oral prophylaxis [11]. PCG is seen not only in humans but also in animals like cats, dogs etc., [12]. PCG usually does not induce loss of attachment but there have been some cases which reported with severe attachment loss and bone loss [13–14]. Sometimes it may also be associated with some benign conditions like odontogenic fibroma [15] inflammatory cheilitis etc., [16]. Many authors tried different drugs to treat PCG [17–19]. These types of swellings can be treated either chemically or surgically but the ultimate goal of management is removal of the offending agent. As the name denotes PCG, shows numerous plasma cells within the tissue which can be differentiated from acute leukemia and multiple myeloma. The histological picture is characterized by cart wheel appearance of nucleus which can be differentiated from plasmoacanthoma (solitary plasma cell tumour) which is a part of the same spectrum of disease as plasma cell cheilitis. The typical differentiation is diffuse sub-epithelial plasma cell inflammatory infiltration into the connective tissue and epithelium shows spongiosis with elongation of rete ridges. PCG resembles other conditions that are aggressive in nature; hence, differentiating it from others is a prerequisite. To differentiate PCG from pemphigus, a negative Nikolsky’s sign is a prime feature [8]. For definitive identification of causative agent of PCG, various screening tests for antigens should be done.
Conclusion
There are few conditions affecting the oral cavity that present with varied features which is difficult to diagnose with only clinical parameters. Such conditions require careful history taking, biopsy examination and immunological investigations to supplement the exclusion of local manifestations of systemic diseases to arrive at a correct conclusion. Lesions associated with leukemia and myeloma resemble PCG and hence, early identification of the disease is essential to prevent the further progression.
[1]. Carranza FA, Hogan EL, Gingival enlargement. In: Fermin C, editorClinical Periodontology 2003 9th edIndiaSaunders:287-88. [Google Scholar]
[2]. Isaac-Renton M, Li MK, Parsons LM, Cinnamon spice and everything not nice: Many features of intra-oral allergy to cinnamic aldehydeDermatitis 2015 26:116-21. [Google Scholar]
[3]. Lamdari N, Pradhan S, Plasma cell gingivitis: A case reportJ Nepal Med Assoc 2012 52:85-87. [Google Scholar]
[4]. Roman CC, Yuste CM, Gonzalez MA, Gonzalez AP, Lopez G, Plasma cell gingivitisCutis 2002 69:41-45. [Google Scholar]
[5]. Donald A Kerr, Kenneth D, McClatchey Allergic gingivostomatitis (Due to gum chewing)J Periodontol 1971 42:709-12. [Google Scholar]
[6]. Gargiulo AV, Ladone JA, Ladone PA, Case Report: Plasma cell gingivitis ACDS Rev 1995 88:22-23. [Google Scholar]
[7]. Manohar B, Bhuvaneshwari S, Plasma cell granuloma of the gingivaJ Indian Soc Periodontol 2011 15:64-66. [Google Scholar]
[8]. Amita K, Vijayshankar S, Anusha K, Hemalatha AL, Diagnostic dilemma in a case of gingival lesion plasma cell granuloma versus extramedullary plasmacytoma- Resolved by immunohistochemistry: A case studyIJMRHS 2015 4:467-70. [Google Scholar]
[9]. Joshi C, Shukla P, Plasma cell gingivitisJ Indian Soc Periodontol 2015 19:221-23. [Google Scholar]
[10]. Mishra M B, Sharma S, Sharma A, Plasma cell gingivitis: An occasional case reportN Y State Dent J 2015 81:57-60. [Google Scholar]
[11]. Arduino PG, D’Aiuto F, Cavallito C, Carcieri P, Carbone M, Conrotto D, Professional oral hygiene as a therapeutic option for pediatric patients with plasma cell gingivitis: Preliminary results of a prospective case seriesJ Periodontol 2011 16:70-75. [Google Scholar]
[12]. Sims TJ, Moncla BJ, Page RC, Serum antibody response to antigens of oral gram negative bacteria by cats with plasma cell gingivitis- PharyngitisJ Dent Res 1990 69:877-82. [Google Scholar]
[13]. Parashis O, Vardas E, Tosios K, Generalized aggressive periodontitis associated with a plasma cell gingivitis lesion: A case report and non-surgical treatmentClinical Advances in Periodontics 2015 5:91-98. [Google Scholar]
[14]. Kumar V, Tripathi AK, Saimbi CS, Sinha J, Plasma cell gingivitis with severe alveolar bone lossBMJ Case Rep 2015 :piibcr2014207013 [Google Scholar]
[15]. Wood NH, Carim R, Ngwenya SP, Diffuse peripheral odontogenic fibroma with concomitant plasma cell gingivitis- A case report and literature reviewSADJ 201 67:448-51. [Google Scholar]
[16]. Abhishek K, Rashmi J, Plasma cell gingivitis associated with inflammatory chelitis: A report on a rare caseEthiop J Health Sci 2013 23:183-87. [Google Scholar]
[17]. Ranganathan AT, Chandran CR, Prabhakar P, Lakshmiganthan M, Parthasaradhi T, Plasma cell gingivitis: Treatment with chlorpheniramine maleateInt J Periodontics Restorative Dent 2015 35:411-13. [Google Scholar]
[18]. Mahler V, Hornstein OP, Kiesewetter F, Plasma cell gingivitis: Treatment with 2% fusidic acidJ Am Acad Dermatol 1996 34:145-46. [Google Scholar]
[19]. Berglundh T, Lindhe J, Tarkowski A, Effects of cyclosporine A on plasma cells in experimental gingivitis in dogsJ Clin Periodontol 1996 23:507-11. [Google Scholar]