High speed vehicular accidents are responsible for distal femur fractures commonly observed in the young and middle aged. Low energy mechanisms such as fall at home may be responsible for producing fractures of distal femur in the elderly osteoporotic population especially women [1]. Fractures of the distal part of the femur are difficult to treat and present considerable challenges in management. Pain, decreased range of motion and compromised function of the knee joint is a common problem arising out of articular incongruity and improper fixation of articular fragments in such fractures [2].
The use of fixed angle devices such as the condylar blade plate and the Dynamic Condylar Screw (DCS) requires certain amount of bone stock which limits their use in comminuted fractures. This led to development of condylar buttress plate for comminuted femoral fractures. However, with standard condylar buttress plate, these fractures often have a tendency to fall into a varus collapse because of toggle at the screw- plate interface. Retrograde nails have proved to be very useful in extra-articular and partial articular distal femur fractures, but fixation of comminuted articular fractures is still a grey area with such an implant. To address these issues, locking condylar plate was designed. A locking condylar plate decreases screw- plate toggle and provides more stable fixation which is one of the key factor in the successful treatment of these fractures. These devices create a fixed angle at each screw hole where the individual screw head is secured to the plate by a locking mechanism [3–5]. Since, the plate does not depend on the friction created at the bone-plate interface to provide stability, the plate does not have to contact the bone directly which helps in preserving the periosteal blood supply [6,7]. Locked implants are typically indicated in patients with osteoporosis, fractures with metaphyseal comminution where the medial cortex cannot be restored, or with a short articular segment [8]. Comminuted articular fractures can also be addressed more conveniently with the use of additional screws such as partially- threaded cancellous screws, herbert screws and other varieties of smaller screws. By making use of the technique of counter- sinking, the screw heads can be adjusted to seat the distal femur locking plate in a proper fashion. It also provides another useful choice for extra-articular fractures of distal femur [8]. Thus, the flexibility of locking condylar plate with its fixed angle properties appears to offer an effective alternative to implants like DCS, condylar buttress plate and a supra- condylar or a distal femur retrograde nail. This study was done to study the functional and radiological outcome of distal femoral fractures in skeletally mature patients treated by open reduction and internal fixation with distal femur locking plate.
Materials and Methods
This was a prospective study conducted from January 2012 to March 2014 at Government Medical College and Hospital (GMCH), Chandigarh with a 2 year follow-up. The study was approved by Institutional Ethical Committee and informed consent was taken from all the patients included in the study. Twenty five skeletally mature patients with distal femur fractures were included in the study. Patients with open grade 3B and 3C distal femur fractures, according to the Gustilo- Anderson classification [9] were excluded from the study. Patients with any fracture other than the distal femur in the ipsilateral limb were excluded from the study.
Initial resuscitation of patients was done in emergency department, limb splinted, appropriate radiographs and CT scan as per requirements was done. Intra-venous (IV) antibiotics (2nd generation cephalospoprins, gentamycin) were administered at admission in case of open fractures which continued post-operatively depending on the requirement. I.V metronidazole was administered in open fractures where anaerobic contamination was suspected. Pre-operative investigations were done consisting of haemoglobin level, platelet count, serum electrolytes and renal function tests, coagulogram, fasting or random blood sugar levels and viral markers consisting of Hepatitis B, C and HIV. A blood group cross-match of the patient was sent to the transfusion medicine department of the hospital prior to surgery. A chest X-ray and ECG were done in those patients as required by the anaesthetic team.
In the operating room after induction of the patient by the anaesthetic team, pre-operative preparations like shaving and scrubbing of part, betadine paint and draping were done. Standard lateral approach by developing the plane between vastus lateralis muscle and lateral intermuscular septum was used for closed fractures of distal femur. In case of open fractures incision was tailored in such a way to include the pre- existing wound to facilitate debridement which was carried out as per standard protocol. Lateral para- patellar arthrotomy by using the Swash- buckler approach or its modifications were used to address the articular involvement of the lateral femoral condyle or the inter- condylar notch. A dual incision (standard lateral plus a medial subvastus incision) was also done in cases where a Hoffa’s fracture or articular fracture of the medial femoral condyle had to be addressed in cases where access via the lateral approach was not possible. We always strived for obtaining anatomical reduction and good solid fixation in the articular area of the distal femur even at the cost of spending an extra amount of time, rather than giving the patient an incongruous joint. Distal femur locking condylar plate was used for fracture fixation using locking, 4.5mm cortical screws and partially- threaded cancellous screws of diameter 4.5mm, Herbert screws for smaller articular fragments and 6.5mm for articular reduction of condyles. Technique of counter sinking for screws heads was used when proper seating of the plate had to be obtained. Length of the plate used was judged based on the extent of fracture of distal femur. In cases of fractures with metaphyseal-comminution with no bony reference point along the lateral cortex for direct fracture reduction the shaft of femur was aligned in the center of the condyles and it was ensured to prevent lateralization of the shaft at time of plate application [10]. Primary bone grafting was done in closed cases where the demand for such a procedure was gauged by the operating surgeon. On an average, operating time varied from 2 to 3 hours in majority of the cases with certain comminuted fractures of type C3 even requiring 4 to 5 hours. The average blood loss was 300- 400ml in each case. No use of tourniquets was done in any of the case.
Post-operatively suction drain was removed after 48 hours and first wound inspection was done on 3rd post-operative day. Intra-venous antibiotics were continued for 24 hours in closed fractures and 72 hours in case of open fractures. Post-operative physiotherapy regime was tailored according to the fracture pattern and fixation achieved. In cases where ever possible, knee bending was started on post-operative day 3. On post-operative day 3, active and assisted knee Range Of Motion (ROM) exercises were initiated. Patients were mobilized based on the degree of bone quality, severity of injuries, and pattern of fractures. At post-operative day 5 to 6, the patients were mobilized with crutches/walker until 6 weeks. Full weight-bearing ambulation without any aids was started at approximately 3 months in majority of the cases with radiographic evidence of fracture union. Patients were discharged at post-operative day 12 with stitch removal being done at the time of discharge, making it convenient for the patient to take bath and maintain good body hygiene. The first follow- up was at 6 weeks and subsequent follow-ups were done at 3 months, 6 months and at 1 year and 2 years. No patients were lost to follow-up.
Statistical Analysis
The statistical data analysis was carried out using a computer based statistical analysis programme, SPSS version 20 (IBM, Chicago, USA). For the statistical data analysis, paired t-test was used between two correlated groups while for uncorrelated groups; means were compared using independent t-test. A p-value <0.05 has been considered significant.
Results
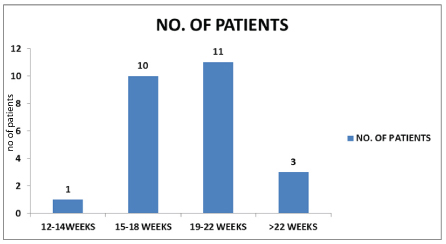
Out of the 25 cases in our study, the mean age of cases in our study was 36.64 years. The youngest patient was of 21 years and oldest patient of 70 years. Most of the cases (80%) were affected by road traffic accident in our study while rest (20%) suffered the fracture from a fall. Out of total 25 cases, 11 cases were extra-articular and rest 14 cases were intra-articular. Further, AO classification of fractures was used in our study. Most of the cases, 11 out of total 25 (44%) were of C2 type [Table/Fig-1]. Thirteen out of total 25 cases had open fracture, and rest 12 cases had closed fracture. Six cases out of total 13 open fractures, (46%) needed initial debridement and temporary stabilisation in the form of external fixator of their distal femur fracture, before putting locking plate. In our study, two patients had early post-operative complication in the form of superficial infection. These were then treated with culture sensitive parenteral antibiotics and antiseptic dressing, which resulted in satisfactory healing of the fracture. One case was found to have late complication in the form of mal-union of the distal femur fracture [Table/Fig-2]. Radiological union was achieved in all the cases. Most of the cases (44%) attained radiological union in 19-22 weeks. The mean time for radiological union was 19 weeks [Table/Fig-3]. Our study had nine cases which required additional surgeries. Out of these all nine cases required bone grafting out of which three required antibiotic cement bead insertion initially. Out of total, 25 patients, four patients (16%) achieved full flexion of 130 degrees or more. Better outcome was observed in terms of range of motion at knee joint in extra-articular fractures (81%) than intra- articular fractures (71%) treated with distal femur locking plate. The mean ROM in all 25 patients was 109 degrees [Table/Fig-1,4,5].
| Knee Movements | A1 | A2 | A3 | C1 | C2 | Total |
|---|
| FULL (130 OR ABOVE) | 2 | | | | 2 | 4 |
| 100-129 | 3 | 1 | 3 | 3 | 5 | 15 |
| 80-99 | | | 1 | | 3 | 4 |
| 60-79 | | | 1 | | 1 | 2 |
| <60 | | | | | | |
Distribution of cases on the basis of early and late post-operative complications.
| Early Post-Operative Complications | No. of Cases | % |
|---|
| Neurovascular Injury | - | - |
| Superficial Infection | 2 | 8% |
| Deep Infection | - | - |
| Failure of Reduction | - | - |
| Thromboembolic Complications | - | - |
| Total | 2 | 8% |
| Late Post-Operative Complications | No. of Cases | % |
| Late Infection | - | - |
| Implant Failure | - | - |
| Mal-Union | 1 | 4% |
| Delayed-Union | - | - |
| Non-Union | - | - |
| Total | 1 | 4% |
Time to radiological union.
Knee rom at end of 6 months follow-up for a patient with extra- articular distal femur fracture (Ao Type A1) fixed with locking plate.
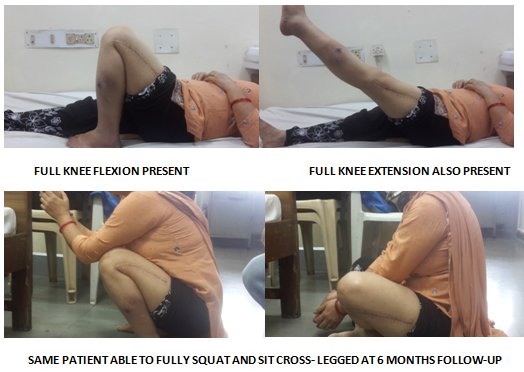
Knee ROM at the end of 6 months follow-up in a patient with intra- articular fracture of distal femur (Ao Type C2) fixed with locking plate.

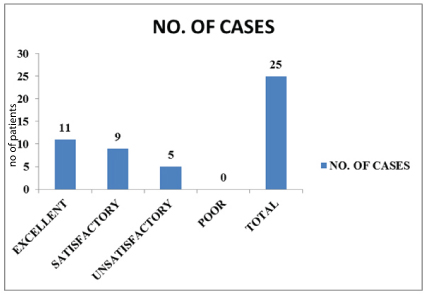
According to Neer’s criteria which included evaluation in terms of pain, range of motion, walking and work capacity, anatomy and X-ray findings score at 6 months was calculated and it was used to compare the results between open and closed fractures [11]. It was observed that clinically ROM at knee joint and score at 6 months was better in closed fractures than open, although statistically insignificant (p-value = 0.6359). Similarly, results were compared in case of intra- and extra-articular fractures, clinically ROM at knee joint and score at 6 months was better in extra-articular fractures than intra-articular, although statistically insignificant (p-value = 0.3075) in this situation as well. In the present study, results were tabulated into 4 groups i.e., excellent, satisfactory, unsatisfactory and poor according to criteria laid down by Neer et al., [11]. Knee score was calculated based on the Neer criteria. Out of 25 cases, 20 cases were graded to be excellent to satisfactory. No case had score less than 55 or graded as poor [Table/Fig-6].
Discussion
With locking condylar plate, we were able to achieve fracture union in all the cases along with good ROM at knee joint (mean ROM being 109 degrees). Similar results were obtained by Rademakers et al., in their study on 67 patients and at 1-year follow-up mean knee range of motion of 111 degrees with excellent Neer score. Study concluded that surgical treatment of mono and bicondylar femoral fractures shows good long-term result after open reduction and internal fixation and knee function increases through time, though the ROM does not increase after 1- year [12].
The mechanical advantage of screw head getting locked in the plate which converts the whole implant into one single solid angular stable construct makes it very useful in comminuted fractures and also in elderly patients with osteoporotic bone. The “combi hole” in the plate offers the dual advantage of applying normal screws in a compression mode as well locking screws in fractures where traditional screw purchase is compromised. This function of locked fixation and its angular stability helps in sparing periosteal blood supply. Also, since no contouring of the plate is required and toggle at the screw- plate interface is minimized the holding power of the implant is increased [13].
The mean age in our study was 36.64 years with positive results obtained in both old as well as young patients. A study published by Charles N. Cornell et al., on use of distal femur locking plate in peri-prosthetic distal femur fractures with average age of patients being 69.4 to 76.7 was able to obtain 77.6% union rate with very few malunions, thus, making it the implant of choice for distal femur fractures across all age groups [14]. Scope of distal femur locking plate is limited not only to isolated distal femur fractures but also in the use of peri-prosthetic distal femur fractures in patients of Total Hip Replacement (THR) [15] and Total Knee Replacement (TKR). Even extreme distal peri-prosthetic supracondylar fractures can be managed with lateral locked plate with predictable results similar to those seen in more proximal fractures [16].
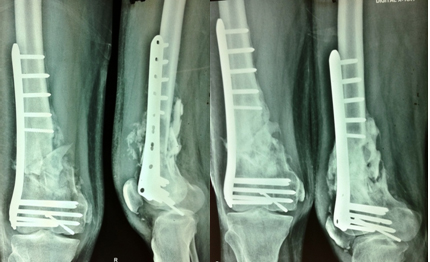
The material of implant was stainless steel in all our cases with union being achieved with good amount of callus [Table/Fig-7]. In sharp contradiction to this a study conducted by Henderson et al., found less callus formed in patients treated with stainless steel plates in comparison to titanium plates [17]. Most studies have achieved positive results with both types of implants and have not made a clear distinction regarding the nature of implant to be used for obtaining good results.
Anteroposterior view and laterals view X-rays showing good callus formation at end of six months in an extra-articular distal femur fracture.

The technique used for fixation was open in all our cases and did not use the technique of Less Invasive Stabilization System (LISS), although positive results have been obtained by many studies by the LISS method [18–21]. A study published recently supported our cause. The study showed post-operative infection and non-union rates to be comparable between LISS and LCP (Locking Compression Plate) for both open and closed distal femoral fracture fixation. The study concluded that either may be used to treat distal femur fractures as no difference was detected between the two plates [22].
Average duration of union in all our cases was 19 to 22 weeks. In isolation for closed fractures the average duration of union was 19 weeks with only one case requiring secondary bone grafting. For open fractures the average duration of union increased to 20 to 22 week, thus, making open fractures a risk factor for delayed union in such fractures. The same concern was voiced by Ricci et al., in their study on open fractures acting as a risk factor for longer duration of union. Besides this they also found diabetes, smoking and increased body mass index as independent risk factors affecting fracture union and out of surgeon’s control. One risk factor within surgeon’s control affecting fracture union and possible cause of failure was use of shorter plate length. Use of longer plates and the technique of spanning comminuted fractures can be detrimental in obtaining positive results and avoiding failure [23]. In all our cases we paid special attention to this particular factor [Table/Fig-8].
The technique of spanning and lagging of distal femur fractures with metaphyseal comminution second figure showing union with callus at end of three months.

The requirement for additional surgeries in open distal femur fractures with excessive soft tissue damage in the form of muscle contusion and contamination was carried out by performing debridement, antibiotic beads insertion and temporary external fixator in the 1st stage. The 2nd stage involved removal of external fixator, beads and definitive fixation in the form of locked plating and bone grafting. The second stage was undertaken only once the wound and soft tissues had healed with no biochemical and clinical features of infection. The average duration for the same being 2 to 3 weeks post the initial surgery.
Out of the 9 cases in our study which required bone grafting 8 cases were open with certain amount of bone loss with only one closed fracture of C2 variety requiring bone grafting [Table/Fig-9]. Distal femur locking plate has decreased the requirement for bone grafting in distal femur fractures especially with metaphyseal comminution [24]. Locked plates thus reduce the complications associated with an additional surgery like bone grafting and donor site morbidity making it a useful implant in distal femur fractures with metaphyseal comminution.
Bone grafting done in a comminuted distal femoral fracture (aO type c2) second figure showing good graft uptake and union at the end of three months.
Fixation of distal femoral fractures with locked plates is still a challenging technique with majority of the failures being with application of surgical techniques rather than the fault of the implant itself. In our study one case developed varusmalunion with bending of plate which could be attributed to the early weight bearing by the patient himself and non-compliance with our physiotherapy regime. A retrospective study conducted by Toro et al., from 2011 to 2014 noted that the various reasons for failure are inadequate plate length, insufficient fracture bridging and inadequate number of locking screws used for fracture fixation. They concluded that locking plate is still an emerging technique with lack of literature [25].
Limitation
The requirement for more number of patients was felt during the conduct of our study but with a longer follow-up of 2 years it was reasonable to restrict ourselves to a follow-up compliant group. The need for further studies and multicenter randomized trials was similarly noted by Griffin et al., in their study [26].
Conclusion
Distal femur locking plate is still the way forward for treating distal femur fractures. Positive results have been published by researchers with implants such as distal femur nail, dynamic condylar screw and even addition of a medial plate to a distal femur locking plate for treating distal femur fractures. By conducting this study we can put forward the assumption with some degree of confidence that fractures of the distal femur of all varieties extra-articular, partial articular and intra-articular non-comminuted as well as comminuted ones, if fixed in a proper fashion following all the basic principles of fracture fixation, good results can be obtained by using a distal femur locking plate alone as the main implant of choice for such fractures. It has also reduced the requirement of secondary procedures such as bone grafting especially in fractures with metaphyseal comminution.