Neuropathic ulcers or trophic ulcers results due to an injury to an area which is compromised due to disease, vascular insufficiency or sensory loss. In leprosy, it occurs due to breakdown of tissue from within, on account of intrinsic muscle paralysis or trauma from outside or fissure foot due to autonomic imbalances. Management of trophic ulcers poses a tremendous challenge to health care due to their poor response to treatment. The search for therapeutic options enhancing quicker healing of trophic ulcers continues. Various methods of treatment in practice are total plaster cast immobilization, saline or collagen dressings, topical phenytoin [1] or metronidazole [2] application, topical growth factors like platelet derived growth factor [3] (becalpermin), epidermal growth factor and other reconstructive surgical procedures. Most of the treatments mentioned above have been used for years. There is need to find simpler, safer and effective means to add to this treatment to reduce the duration of treatment, by decreasing the number of dressings and hence shortening the inpatient hospital stay and thus improves the patients’ quality of life. One such treatment is the use of Platelet Rich Plasma (PRP). The autologous PRP is prepared from one’s own blood by the process of centrifugation and platelet activation. On application to the wound, it directly introduces growth factors and cytokines, thereby normalizing the metabolic process, promoting neoangiogenesis, improving cellular metabolism and activating local immunity [4].
To determine the role and effectiveness of PRP in the healing of trophic ulcers and study the rapidity of healing with respect to the ulcer site, size, duration, type of leprosy and associated motor deformities.
Materials and Methods
A prospective interventional study conducted in Govt. Stanley Medical College and hospital from August 2014 to August 2015. Around 50 leprosy patients with trophic ulcer were included after obtaining the Institutional Ethical board Clearance and written informed consent from the patients, based on the inclusion criteria : both sexes, grade II of Wagner’s ulcer classification, ulcer area > 1cm x 1cm and <6cm x 6cm, negativity for organisms on pus culture and sensitivity, negativity for HIV, HBV and HCV serology. The exclusion criteria was: ulcer with underlying osteomyelitis or deeper ulcers with tendons and/or bones exposed, haemoglobin <11g%, platelet count <1.5 lacs/mm3, ankle brachial index <0.9, patients on anticoagulants or therapies hindering wound healing, patients with bleeding tendencies, lepra reaction, uncontrolled diabetes mellitus, malignancies and other major systemic diseases, pregnancy, lactation and patients not willing for the procedure or for follow-up. Detailed history taking and meticulous clinical examination was done with reference to the ulcer and activity of Hansen’s disease. All patients were subjected to routine blood and urine examination, peripheral smear, swab for pus culture and sensitivity, serology for HIV, HBV, HCV, and X-ray and Doppler study of affected limb.
PRP Preparation
Ten ml of blood withdrawn from the median cubital vein was used for preparation of PRP. Under strict aseptic precautions, the process was carried out with temperature maintained at 22–260C by manual double spin method [5]. A 10ml of venous blood was collected from the patient in centrifuge test tubes labeled with identification data (name and age) and mixed with anticoagulant Acid Citrate Dextrose (ACD) in the ratio of 10:1.5. The tube was then placed for first centrifugation at the rate of 2000 rpm for 10 minutes when plasma separated; plasma, buffy coat and upper layers of RBCs were pipetted into another test tube. This was subjected to second centrifugation at the rate of 3000 rpm for ten minutes. Platelets settled down, upper 3/4th supernatant was discarded and the lower PRP was obtained. It was activated just before application by adding 10% calcium chloride in the ratio of 1: 10 and agitating it with vigorous shaking.
Measurement of Ulcer by Clock-face Method
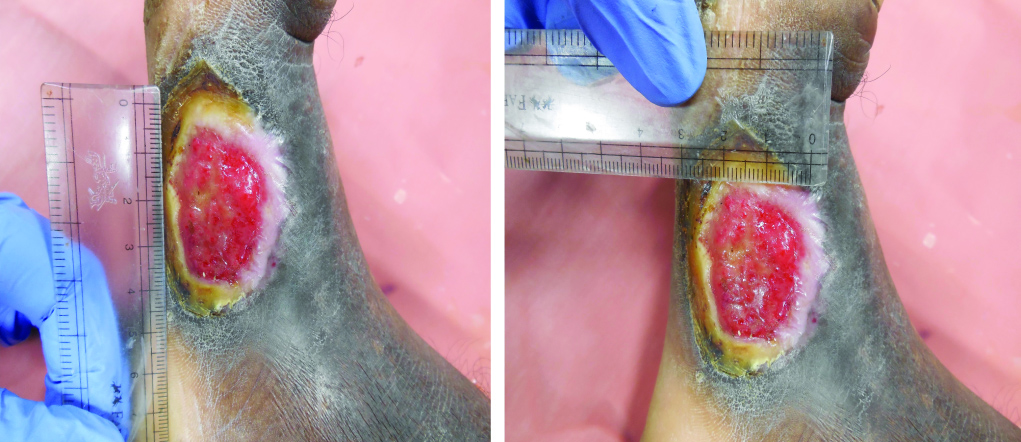
Cotton-tipped applicators and disposable scales were used to measure length, width, and depth of the visible wound. Sussman described the way of measuring ulcer by using clock face method [6,7], in which length was 12:00 to 6:00 with 12:00 toward the head; width was 3:00 to 9:00 side by side. Depth was taken from the deepest point of the wound bed to the level of normal skin surface Wound volume was calculated using the formula for an ellipse [8]: length × width × 0.7854 x depth (an ellipse is closer to a wound shape than a square or rectangle that would be described by simple length × width) [Table/Fig-1].
Face clock method of ulcer measurement.
Ulcer volume reduction was assessed based on reduction rate at the end of 6th week.
Procedure Proper
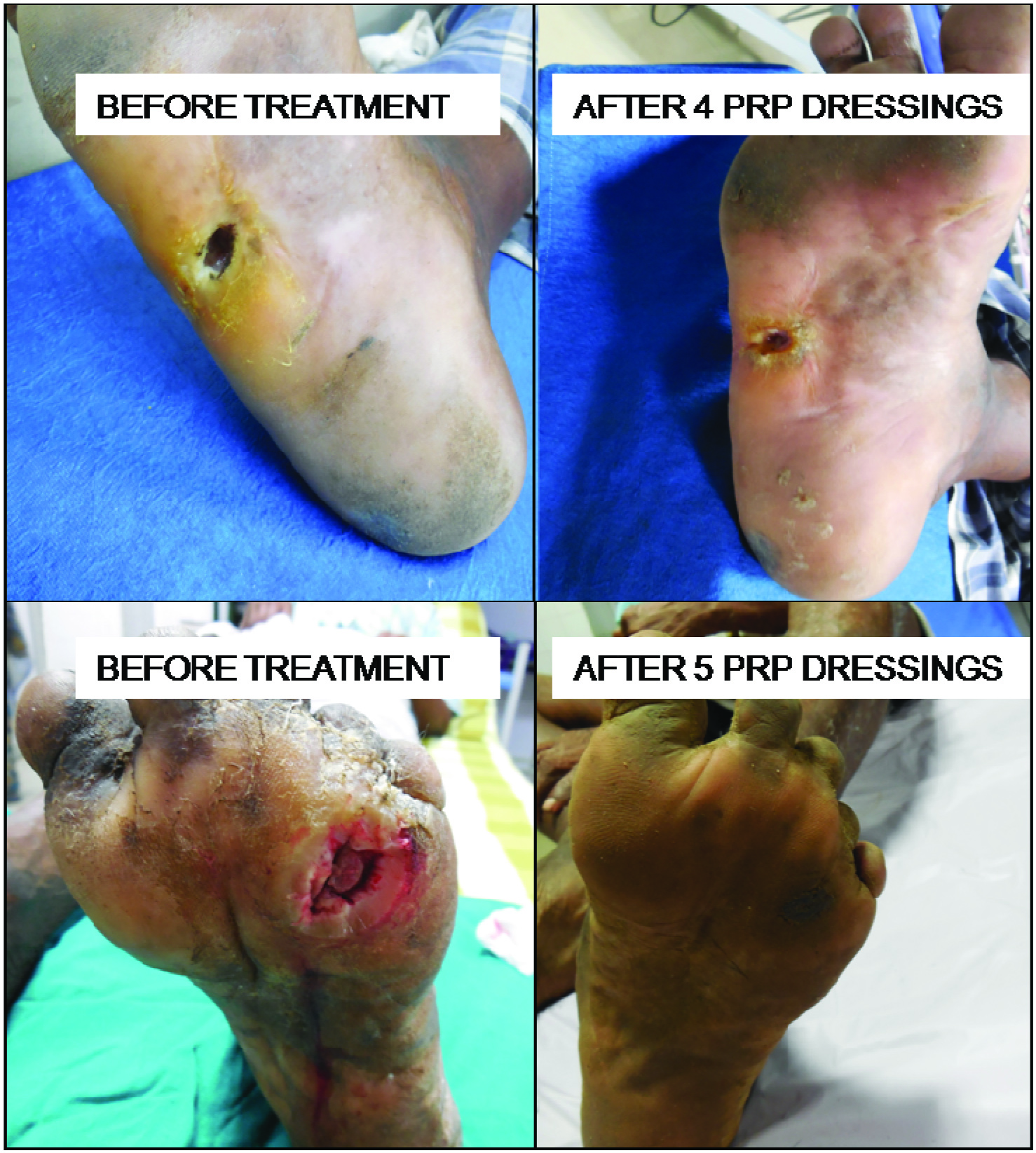
After wound debridement, the surface was irrigated with normal saline; activated PRP was applied over the ulcer by spraying and occlusive dressing was done with sterile gauze and pads. At every visit, serial photograph were taken and compared [Table/Fig-2].

Post-Procedure Advice
Patients were advised to avoid prolonged standing, to use appropriate off-loading Microcellular rubber footwear while walking and to leave the dressing in-situ till follow-up after one week. In the intervening period patients were given multivitamin supplements and if on multidrug therapy, were asked to continue it. Patients with ulcers over lateral malleoli were advised to avoid crossed leg sitting position.
Follow-up
All the patients were followed-up every week. The same procedure was repeated until either complete ulcer healing or up to maximum of 6 sittings, whichever occurred first. At each visit, wound area and volume was measured and serial photographs were taken.
Results
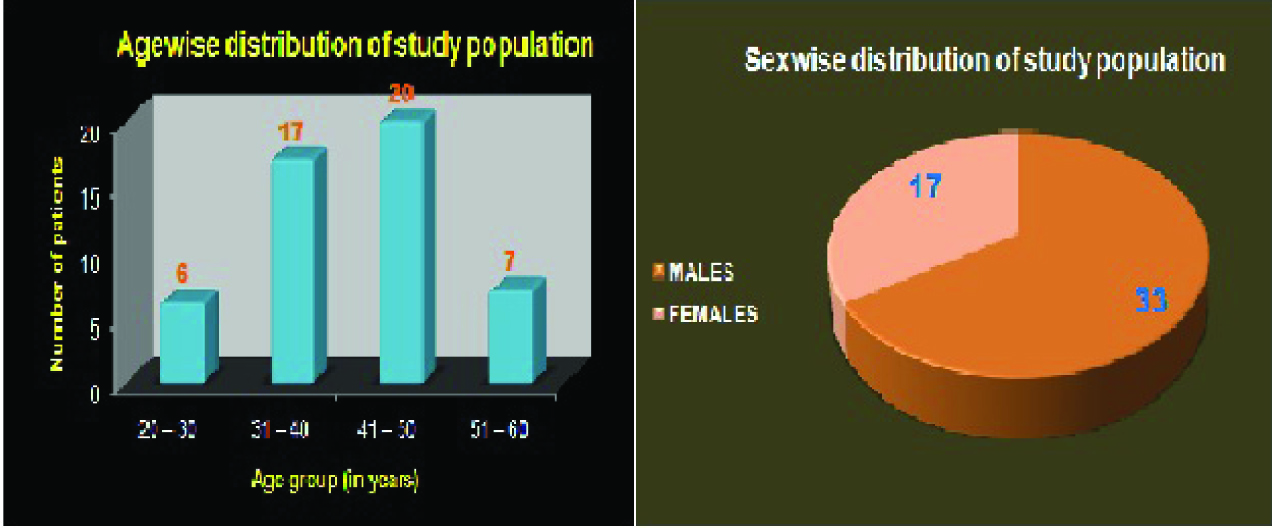
Out of 50 patients of Hansen disease with trophic ulcer, 33 patients (66%) were males and 17(34%) females with mean age of the patients were 41.9% [Table/Fig-3].
Age and sex wise distribution of study population
Most common cause for trophic ulcer was breakdown of substandard foot with normal or excessive walking as evidenced in our study with 34% patients being farmers and 14% manual labourers.
In our study, 24% patients were on Multibacillary Multidrug Therapy (MBMDT) and 38 patients (76%) completed MBMDT. Our study showed treatment with MBMDT did not influence wound healing.
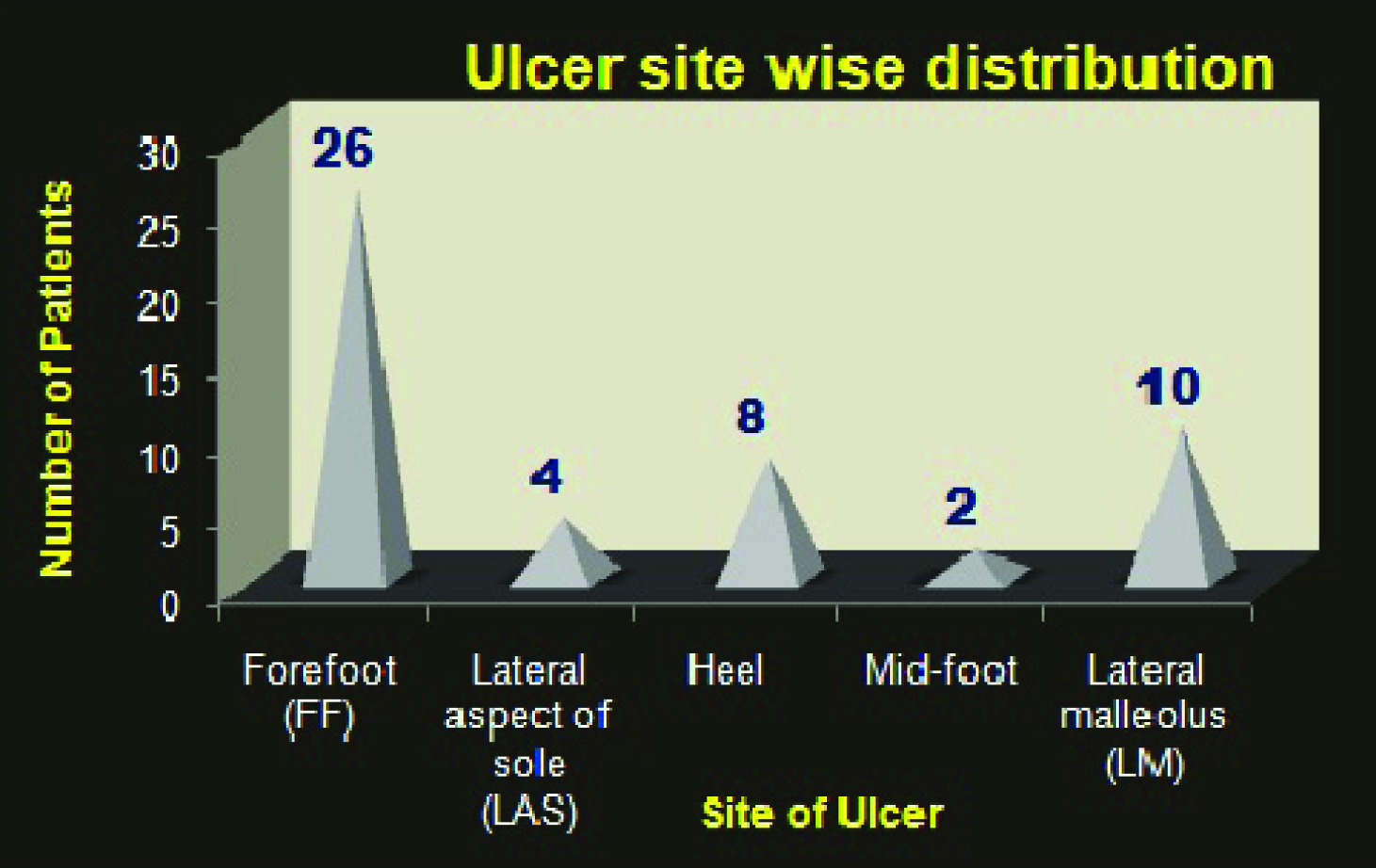
In our study, 52% of ulcers were over forefoot, 20% over lateral malleolus and 16% over heel. Whatever may be the site of ulcer, it showed no statistical significance on ulcer healing with PRP therapy [Table/Fig-4].
Ulcer site wise distribution.
In our study, 42% patients had motor deformities confined to the intrinsic muscles of the foot. It did not show any statistical significance on ulcer healing.
Mean ulcer duration was 11.62 weeks and duration of ulcer had no statistical significance on healing with PRP therapy.
In our study, 46 patients (92%) showed complete healing with PRP. In 4 patients (8%) there is marked reduction in wound size but only near complete re-epithelization [Table/Fig-5,6]. Among the patients who showed complete healing, 88% patients achieved this after 4th sitting, 8% showed improvement in the third sitting [Table/Fig-7].
Ulcer volume reduction rate.
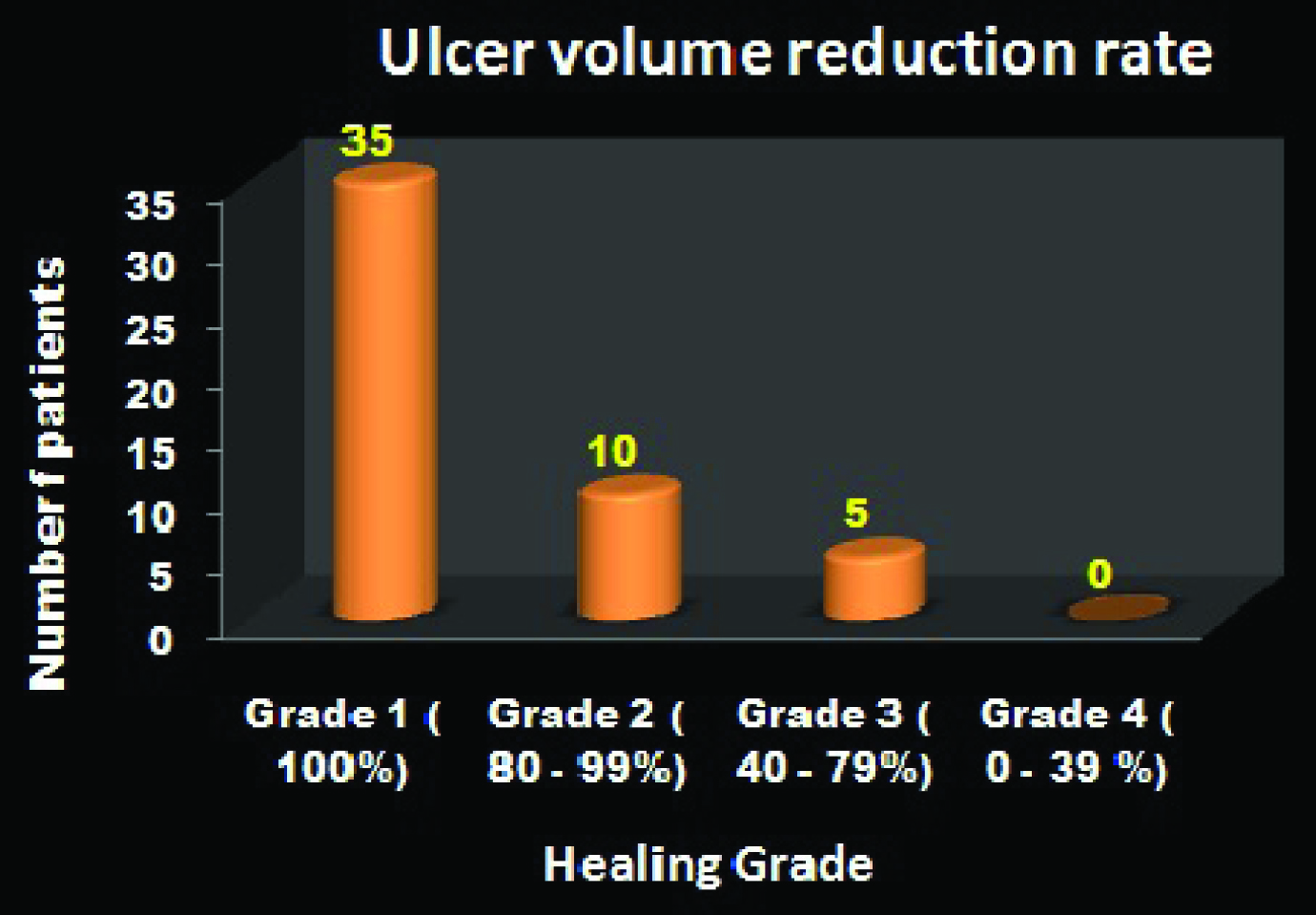
Healing grade and percentage of improvement.
| Healing Grade | Baseline | End of 5th Week |
|---|
| Grade 1 [100%] | 0 | 35 |
| Grade 2 [80-99%] | 11 | 10 |
| Grade 3 [40-79%] | 33 | 5 |
| Grade 4 [0-39%] | 6 | 0 |
No. of sittings for ulcer healing.
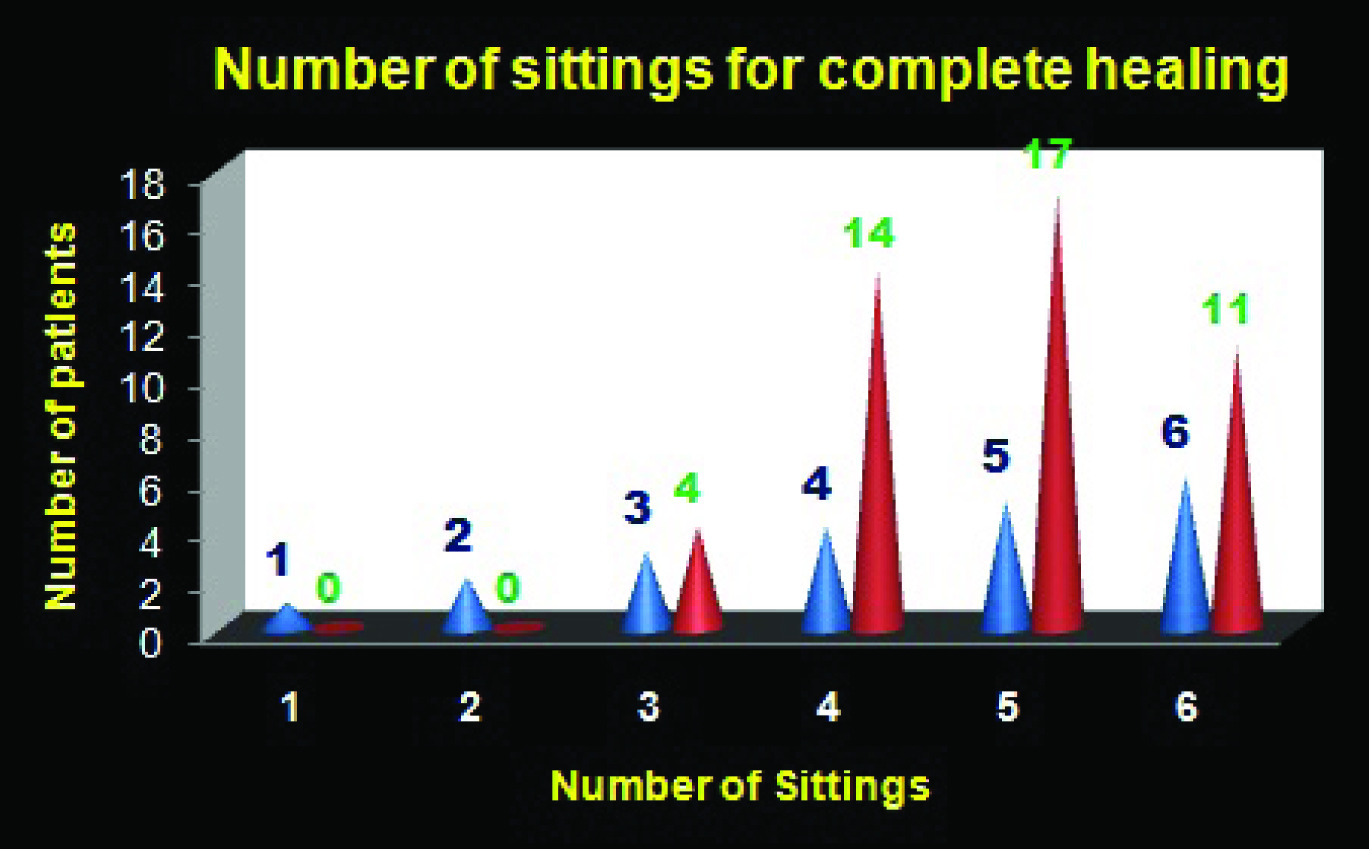
Mean time for ulcer healing with PRP was around 4.38 weeks and 92% patients showed complete re-epithelization within 6 sittings of PRP treatment without any complications or dropouts during the study period [Table/Fig-8,9].
Before and after treatment response with no. of sittings.
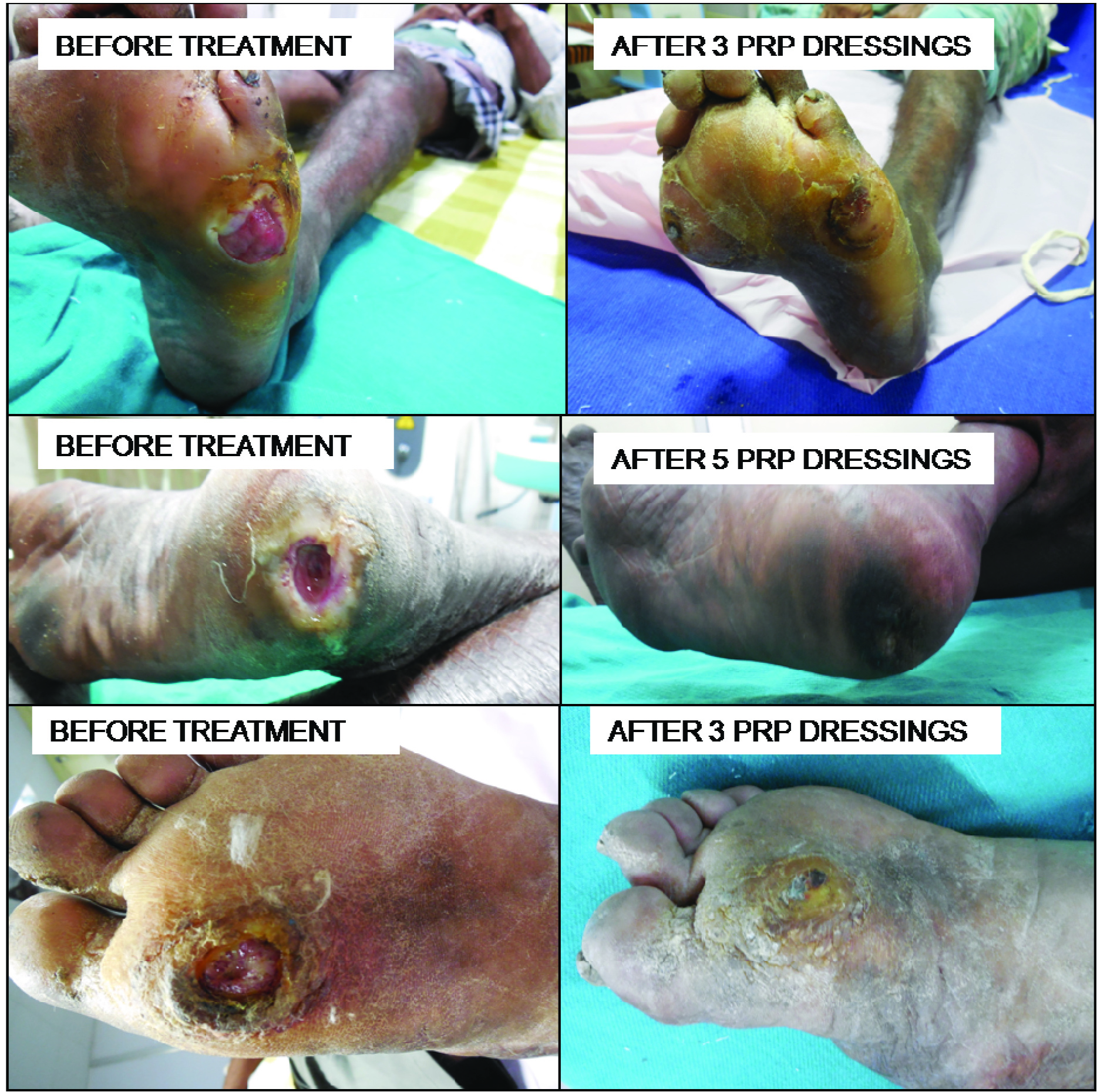
Before and after treatment response with no. of sittings.
Discussion
In 1959, Price introduced the term trophic ulcer. Trophe means nutrition. It is characterized by chronic ulceration of the anesthetic foot, overlying the bony prominences with increased tendency to recur [9]. The moment ulceration occurs, the foot becomes ‘ulcer prone’ and a vicious cycle of scar-ulcer-scar takes place. In 2013, 126,913 new cases of Hansen’s disease were recorded in India with 3.4% having grade 2 deformities. It is associated with morbidity, psychosocial stigma and it finally cripples the patient. The management of patients with trophic ulcers is difficult, as it is a recurrent and recalcitrant problem.
Plantar ulcers in leprosy differ from traumatic ulcers as the pathological process begins with loss of sensation and autonomic imbalances superimposed on intrinsic muscle paralysis. Ulcers which have been treated by conservative methods like plaster cast immobilization recurs soon, as some inflammation still persist with friable adhesions.
The process of wound healing is complex, requiring cellular events brought about by various mediators. PRP (autologous platelet gel, plasma rich growth factor and platelet concentrated plasma) provide abundant platelets that are concentrated into a small volume of plasma [10]. The growth factors released from the α-granules of the activated platelets, along with plasma proteins namely fibrin, fibronectin and vitronectin play a pivotal role in modulation of tissue repair and regeneration.
Platelets trigger biological effects including directed chemotaxis, angiogenesis and cell proliferation and differentiation, which play a key role in the process of tissue repair and regeneration. They contain a large number of growth factors and cytokines which play a key role in inflammation and tissue repair. These characteristics of platelets have led to the idea of using platelets as a therapeutic tool to promote wound healing, particularly in patients in whom tissue repair is compromised.
Initially PRP was used as a gel in dentistry by Robert E. Marx in 1990 [11]. Autologous PRP is prepared from the patient’s blood, by using the principle that on centrifugation, different components of the blood get separated based on their specific gravity. The advantage of autologous PRP is the avoidance of risk of disease transmission. Around three to eight times the normal platelet levels are concentrated in PRP. Apart from the growth factors, activated platelets release large amounts of substances that contribute to primary homeostasis, including serotonin, catecholamines, fibrinogen, fibronectin, factor V, factor VIII (Von Willebrand factor), thromboxane A2 and calcium. Qualitatively altered platelets i.e., damaged /non-viable platelets do not secrete growth factors and may give suboptimal results.
In this study on Hansen’s disease with trophic ulcers, male patients outnumbered female patients around fourth decade, in the productive period of life. Our study goes in concordance with literature that Hansen’s disease and deformities are more common and severe in males. Even though females are more prone for reactions, early treatment and restricted outdoor activities prevent them from grade 2 deformities. In elderly patients, wound healing is slow with reduced inflammatory response and altered cytokine profile but our study showed that ageing had no statistical significance in ulcer healing with PRP treatment.
Host immunity determines the spectrum of leprosy. Borderline patients are more prone for reactions because of immunological instability that leads to frank neuritis or silent paralysis and muscle weakness, promoting trophic ulcer formation. Our study correlates with literature that 58% patients were in borderline tuberculoid spectrum of disease. Spectrum of disease did not show any statistical significance on ulcer healing when treated with PRP.
Plantar ulcers are not distributed evenly in the sole and more common over the forefoot and lateral malleolus especially in Indians because of cultural habits; our study is in concordance with literature; associated motor deformities with loss of arch of foot can predispose to unusual ulcer sites and increased recurrence.
A study conducted by Frykberg et al., on 49 patients with 65 nonhealing ulcers showed a mean healing time of 2.8 weeks [12]. Suryanarayanan S et al., showed a mean duration of healing of 5.6 weeks (SD 3.23) among 24 patients [8]. Above mentioned studies were done in chronic leg ulcers due to various causes including only a few patients with trophic ulcer secondary to Hansen disease.
Limitation
Our study has not compared with other traditional methods used to treat trophic ulcers. Patients were followed up for only 3 months.
Conclusion
The use of PRP has greatly reduced the duration of treatment, thus shortening the inpatient hospital stay and improving the patient’s quality of life. PRP therapy is the preferable treatment option in leprosy patients with chronic non-healing ulcers and should be included in treatment armamentarium of all Hansen’s disease patients with chronic trophic ulcers. It is a simple, safe and cost effective in-office procedure, albeit requiring an optimal set-up and expertise.