Local anaesthetic injected into the spinal subarachnoid space, acting on the spinal nerve roots is the principal site for central neuraxial blockade. Depending on the dose, concentration or volume of local anaesthetic used, posterior spinal nerve root blockade interrupt the somatic and visceral sensations, whereas anterior spinal nerve root blockade interrupt efferent motor and autonomic outflow. Spinal anaesthesia is a safe, inexpensive, reliable and effective method for providing regional anaesthesia for caesarean sections and lower abdominal surgeries [1,2]. Lumbar puncture with subarachnoid injection is a difficult medical skill to acquire, where success depends on the skill and experience of the physician, patient’s spine anatomy and patient positioning [3]. Epidural anaesthesia though widely practiced in developing countries, is costlier and requires more technical skill in comparison to spinal anaesthesia. Hence, spinal anaesthesia is ideally suited for use inresource constrained developing countries. Additional benefits with spinal anaesthesia include the preservation of spontaneous respiratory effort, eliminating unnecessary airway manipulations, risk reduction for aspiration pneumonia and surgical haemorrhage with lowered incidence of post-operative ileus. Spinal anaesthesia related complications include Post-Dural Puncture Headache (PDPH), urinary retention, lower back pain, etc [4].
An estimation of the skin to Subarachnoid Space Depth (SSD) has been shown to reduce the number of unsuccessful attempts, repeated attempts, traumatic or bloody lumbar punctures, often acting as a depth guide for proper spinal needle placement [5]. A failure in obtaining Cerebrospinal Fluid (CSF) despite proper spinal needle placement(beyond the estimated depth) would suggest an offline track, requiring needle redirection. The SSD varies considerably at different levels of the spinal column in an individual, inter-individual variation also exists at the same vertebral level [6]. So a pre-puncture estimation of the skin to the SSD may be a good guide for proper spinal needle placement [7]. Adequate knowledge of the SSD often aids in selection of an appropriate sized spinal needle.
A conventional spinal needle may often be too long for a lean patient, while it may fall short of length for an obese patient resulting in multiple unsuccessful punctures, causing patient discomfort [7]. Therefore, a co-relation might exist between physical parameters like age, sex, height, weight and Body Mass Index (BMI) with SSD. By determining this co-relation between the physical parameters (age, sex, BMI) we may successfully and precisely predict the skin to SSD. Studies estimating the skin to SSD in the adult Indian population are relatively few and have been rarely evaluated based on gender, age, BMI [8]. Therefore, we designed an observational study to evaluate the variation of SSD among male, non-pregnant female and parturient female population in a tertiary care hospital in India.
Materials and Methods
After proper approval from the institutional ethical committee this prospective, observational, analytical study was conducted under the Department of Anaesthesiology and Critical Care at Gauhati Medical College and Hospital from January to August, 2015. Convenience sampling of 300 patients aged 18 to 60years, belonging to either sex, American Society of Anaesthesiologists (ASA) physical status I and II, parturient females, scheduled to undergo elective abdominal or lower limb surgeries under spinal anaesthesia using midline approach were chosen as the sample population. Informed consent was obtained from the participants. They were further divided into three groups, GROUP M (containing 100 male patients), GROUP F (containing 100 non-pregnant female patients) and GROUP PF (containing 100 parturient female patients).
Exclusion criteria included patients with neurological disorders, seizure disorder, spinal anomaly, low back pain, prior spine surgery, skin infection at the needle puncture site, sepsis, neuraxial anaesthetic drug allergy, coagulation disorders, associated medical illness with relatively contraindication to spinal anaesthesia, pregnant patients with hypertensive disorders & patients in whom paramedian approach of spinal anaesthesia had to be used were excluded from the study population.
Pre-anaesthetic evaluation with proper explanation of the procedure to be undertaken was done. The age, height, weight of the patients was recorded pre-operatively. Body Mass Index (BMI) was calculated using Quetelet index [9] (BMI = Weight in kg/height in meter2). Patients were kept nil orally for 6 hours. On arrival at the operating room peripheral I.V. access was secured with a standard 18 gauge intravenous cannula, standard ASA monitors were attached and baseline vitals were noted. All patients were pre-medicated as per hospital protocol and received l0ml/kg of Ringer’s Lactate solution over a period of l5 minutes before administering spinal anaesthesia. Following all aseptic and anti-septic precautions spinal anaesthesia was administered between the third and fourth lumbar inter-vertebral space with the patient in lateral recumbent position. A skin wheal was raised with the 1% lignocaine solution at the selected interspace and lignocaine solution was injected upto the interspinous ligament. Then a skin nick was made with the triangular knife over the wheal. Dural puncture was performed with a 23/25 gauge Quincke (3.5 inch/ 9cm) spinal needle using the midline approach with a slight cephlad angle to the skin. The needle was slowly advanced, when dural puncture was felt, the stylet was removed to observe for back flow of CSF. When free flow of CSF was observed the stellate was reinserted partially and the length of the needle was marked with a skin marker at the site of skin entry, later measured using slide callipers. The local anaesthetic was then injected into the subarachnoid space. The dose of intrathecal local anaesthetic was decided as per our hospital protocol, the patient characteristics and the surgical requirement. Traumatic lumbar puncture, any alteration in the angulation of the spinal needle compared to the angulation at the time of insertion, use of paramedian approach were eliminated from analysis of SSD. Following intrathecal injection, the spinal needle was marked and withdrawn and later the depth of insertion was measured using slide calipers to analyse the SSD. Surgery was started after desired level surgical blockade was achieved. Intra-operative monitoring as per standard protocol was done. Patients were managed on case by case basis by the concerned consultant anaesthesiologist.
Statistical Analysis
Statistical Package for Social Sciences (SSPS 21.0, Chicago, IL) was used for the analysis. Descriptive statistics for overall sample and group wise (Group M, Group F and Group PF) were calculated for all the variables. Data was expressed as mean and standard deviation. Demographic parameters and SSD were compared using one-way ANOVA with post-hoc (Bonferroni correction factor) analysis to observe significant differences among the study groups. Multivariate analysis was done. Forward step wise multivariate regression analysis was performed to see important covariates influencing SSD for each group separately. The p-value 0.05 (two tailed) was considered as statistically significant.
Sample size calculation was based on a total of 6901(2308 male, 2260 non-pregnant female, 2332 parturient female) number of patients who were operated under spinal anaesthesia in the various surgical departments of the hospital, over a span of 8 months previously. Taking a confidence interval of 0.95 and using systemic sampling technique, a total sample size of 290 patients was determined (Group M=97, Group F=95, Group PF=98). Taking a 3% failure rate of spinal anaesthesia a sample size of 100 patients per group was taken for our study.
Results
The study population comprised of 100 male, 100 non-pregnant female and 100 parturient female patients who underwent surgery under spinal anaesthesia under various departments such as Gynaecology, Orthopaedics, General surgery, Urosurgery etc., in Gauhati Medical College and Hospital. Patient characteristics and skin to SSD were observed in this study using a predesigned proforma (Annexure 1). The overall mean and standard deviation of demographic parameters observed in our study population were an age of 35.48±l2.38 years, the height of 156±0.06 centimeters, and the weight of 55.98±7.l3 kilograms, the BMI observed was 22.88±2.39 kg/m2 [Table/Fig-1].
Demographic parameters (overall).
| Patient characteristics | n=300 |
|---|
| Age (years) | 35.48±12.38 |
| Height (cm) | 156±0.06 |
| Weight (kg) | 55.98±7.13 |
| BMI (kg/m2) | 22.88±2.39 |
The demographic characteristics and skin to SSD observed in the three groups, Group M, Group F and Group PF are depicted in [Table/Fig-2]. The overall mean SSD was 4.37±0.31cm [Table/Fig-3].
Demographic parameters (for each group).
| Patientcharacteristics | Group-M(N=100) | Group F(N=100) | Group PF(N=100) | p-value |
|---|
| Age (years) | 40.0±14.7 | 40.4 | 26.0±4.1 | <0.05 |
| Height (cm) | 161.3±5.0 | 153.8±5.4 | 154.00±5.5 | <0.05 |
| Weight (kg) | 59.7±6.4 | 51.6±6.9 | 56.6±5.7 | <0.05 |
| BMI (kg/m2) | 22.9±1.93 | 21.8±2.4 | 23.9±2.3 | <0.05 |
Skin to subarachnoid space distance.
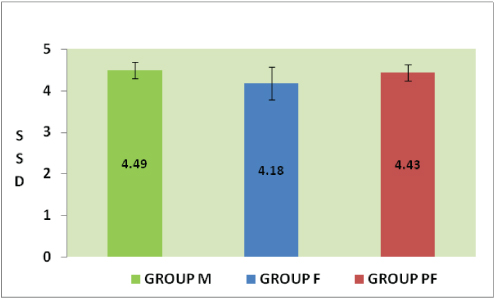
Age in Group M and Group F was significantly different from Group PF. Height in Group M was significantly different from those in Group F and PF. BMI values in Group M were comparable with those in Group F but significantly different from those in Group PF. The age, height, weight and BMI values showed a statistically significant difference among the two groups. There was significant difference in BMI values among the 3 groups. Post-hoc Bonferroni correction factor comparisons after ANOVA analysis showed that, the observed SSD in Group M was significantly different from Group F but was comparable with Group PF [Table/Fig-4].
Showing Pearson correlation coefficient showing correlation of the variables with skin to sub arachnoid space depth.
| Skin to subarachnoidspacedepth(SSD)Correlationcoefficient | WeightCorrelationcoefficient | HeightCorrelationcoefficient | AgeCorrelationcoefficient | BMICorrelationcoefficient |
|---|
| Group M | 1.000 | 0.712 | 0.229 | 0.024 | 0.777 |
| Group F | 1.000 | 0.702 | 0.181 | 0.081 | 0.730 |
| Group PF | 1.000 | 0.739 | -0.116 | 0.031 | 0.873 |
Multivariate regression analysis was performed to determine the covariates (age, height, weight, BMI) that influence SSD in our study groups. In group M patients the SSD was seen to correlate with the BMI and height of the patients. In group F patients SSD correlated with the BMI, height and age of the patients. In group PF patients SSD correlated with the BMI, weight and height of the patients. Though there was a linear correlation between SSD with age and height, the values were not significant [Table/Fig-4,5].
Showing regression equation for the three study groups.
| For GROUP M, y =1.718+0.077BMI+0.632 Height |
| For GROUP F, y = 1.828+0.077 BMI+0.018 Height-0.007 Age |
| For GROUP PF, y = - 4.748+0.209BMI+4.703 Height -0.054 weight |
| Regression equation for the three groups where y= Subarachnoid space depth (SSD) |
Discussion
In this prospective, observational, analytical study while evaluating the relationship of distance of skin to SSD with age, sex and BMI in patients undergoing spinal anaesthesia we observed a SSD of 4.49±0.19 cm, 4.18±0.39 cm, 4.43±0.19 cm in male, non-pregnant female and parturient female patients respectively, the mean SSD observed in our study population was 4.37±0.31cm. The longer skin to SSD in parturient females compared to non- pregnant females may be due to hormonal effects of pregnancy such as weight gain, softening of tissues and ligaments and collection of fat in the subcutaneous tissues. It can be observed that various anthropometric variables such as age, height, weight, BMI showed statistically significant differences between males, non-pregnant and pregnant females. The difference in anthropometric variables may be the reason behind the observed differences of skin to SSD.
Basgul et al., in a similar study on Turkish population observed a mean SSD of 5.40±0.66 cm [10]. Vassiliadis et al., studies SSD among Greek population and reported a mean SSD of 5.4±0.7 cm in male patients which was 1cm longer that that observed in our male population [11]. Both these studies observed a higher SSD than our study population. The shorter SSD, observed in our study population, was possibly because of shorter patients observed in our sample population compared to western population who were much taller. Prakash et al., observed a mean SSD of 4.71±0.31cm in Indian population, which was comparable to our study results [8]. The observed SSD in 288 male, 205 non-pregnant female and 190 parturient female patients by Prakash et al., was 4.8l±0.68 cm, 4.55±0.66cm and 4.73±0.73cm respectively, which were comparable with the SSD observed in our study population [8]. In a study by Bassiakou et al., on Greek population, the observed SSD in parturient females was 6.5±l.2cm, which was 2.07cm longer than that found in our study group [12]. It was probably because subcutaneous tissue is the most variable layer that is related to weight of a patient [13].
The formulae to predict the skin to SSD derived from our study was for males: SSD (cm)= 1.718+0.077 BMI+0.632 Height, for non-pregnant females: SSD (cm) = 1.828+0.077 BMI+0.018 Height-0.007 Age, for parturient females: SSD (cm)= -4.748+0.209BMI+4.703 Height -0.054 weight. In our study SSD correlated with BMI and height among all our study population. Among the measured variables but there was co-rrelation of SSD with age among non-pregnant female patients and weight among the parturient female patients. Prakash et al., in a similar study to estimate SSD observed that the predictive formulae for estimating SSD in males correlated with the weight and age (SSD (cm) = 2.86+0.03×weight+0.004×age), in non-pregnant females it correlated with weight (SSD (cm) = 4+0.18×weight−10.3×BSA+0.04×height), BSA and height and with only BMI in the parturient group [8]. Vassiliadis et al., found a positive correlation of SSD with age but not with weight, height and BMI in male patients, however in parturient females, SSD could be correlated with weight and height [11]. Bassiakou et al., also reported co-rrelation between SSD, BMI and body weight in parturients, whereas in male patients SSD correlated with weight and age [12]. Formulae to calculate SSD by Bonadioet al., SSD (cm) =0.77cm + 2.56 ×BSA (m2), Craig et al., SSD (cm) =0.03cm × height(cm) and Stocker et al., SSD (mm) =0.5 × weight (kg)+18 were based on Body Surface Area (BSA), height and body weight, respectively and did not correlate with BMI as observed in our study [13–15]. Basgul et al., in Turkish population, observed weight as the only significant predictor of SSD [10].
Use of spinal ultrasound to predict the SSD was observed by Gnahoet al., who reported that an accurate estimation of SSD was possible using ultrasound [16]. However, equipment non-availability, costs and lack of proper skills in performing neuraxial ultrasound may limit its role in determining the SSD. Hence, SSD predicted using simple mathematical calculations may be practical.
Limitation
The formulae to predict the SSD is applicable only for midline approach and not for paramedian approach of spinal anaesthesia. Other limitations of our study include non-randomisation of sample population. Multicentric prospective studies are required for the validation of the formulae.
Conclusion
Spinal anaesthesia is a reliable anaesthetic technique for lower abdominal, caesarean section, urological and lower limb surgeries. Based on our study findings, it can be concluded that there is a variation in skin to SSD based on age, sex and BMI, with a greater SSD being observed in male and pregnant female patients compared to the non pregnant female patients. Skin to SSD may be correlated with the BMI as suggested by our study results. But multicentric studies taking larger population needs to be undertaken to further confirm our study results.
| ANNEXURE-1 |
|---|
| PROFORMA: |
| Serial No: Hospital No:Name of the patient: ASA grade: Age: Sex: Religion: Occupation:Address:Height (cm): Weight (kg):Body mass index (BMI):Date of admission: Date of operation:Diagnosis:Surgical Procedure:History:H/O present illness:H/O any associated illness:Past medical and surgical history:Personal history:Family history:Drug history:General Examination:Pulse: Blood pressure:Systemic Examination:Airway Examination:Laboratory Investigation:Any specific investigation, if required.Skin to subarachnoid space distance: |