Ruptured Sinus of Valsalva with Infective Endocarditis Complicated with Post-Infectious Acute Glomerulonephritis: A Rare Case Presentation
Aditya Singh Kutiyal1, Mradul Kumar Daga2
1 Senior Resident, Department of Medicine, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India.
2 Director Professor, Department of Medicine, Maulana Azad Medical College and Lok Nayak Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Aditya Singh Kutiyal, 33, Binsar Apts., A.K.-4, Indirapuram-201010, Ghaziabad, Uttar Pradesh, India.
E-mail: kutiyaladitya@gmail.com
Ruptured Sinus of Valsalva (RSOV) is a rarely seen disease condition. RSOV can have varied presentations from being asymptomatic with just a cardiac murmur to profound hypotension. There has been simultaneous occurrence of RSOV with Infective Endocarditis (IE) in literature. Glomerulonephritis has also been reported in approximately 20% patients with IE. Large amount of proteinuria or decline in kidney functions is rarely encountered and mostly this finding has been incidental on routine evaluation. The co-existence of all the three conditions in a single patient is rare. This case was diagnosed to have RSOV with IE and was also diagnosed with post-infectious glomerulonephritis on renal biopsy. Patient was advised corrective cardiac surgery, but due to financial constraints, patient could not be operated and he died. Here, we report for the first time an unusual presence of both RSOV and sub-aortic membrane with IE complicated by glomerulonephritis.
Cardiac murmur, Hypotension, Proteinuria
Case Report
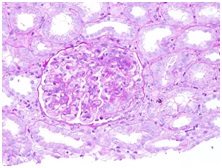
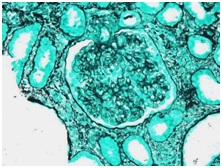
A 19-year-old male presented with complaints of fever since one week and breathlessness since two days. Breathlessness used to increase in the lying down position. Fever was of moderate grade, not associated with chills and rigor. There was no history of chronic cough, burning micturition, loose stools, abdominal pain and jaundice. On examination blood pressure was 136/60mmHg and pulse rate was 108/minute and regular. Apex beat was palpated at 6th intercostal space 4cm lateral to midclavicular line, parasternal heave and systolic thrill were present with pansystolic murmur at apex radiating to ipsilateral axilla and systolic murmur radiating to bilateral carotids. Respiratory examination revealed crepitations in bilateral basal lung fields. Patient was thoroughly investigated. Urine examination revealed presence of albumin with 12-15pus cells/high power field (hpf). Electrocardiography showed sinus tachycardia, C-reactive protein - positive, however rheumatoid factor was negative, and human immunodeficiency virus I and II was non-reactive, hepatitis B surface antigen and hepatitis C virus antibody were non-reactive. Anti-streptolysin O was < 200units. Chest X-ray showed only mild bilateral costophrenic angle blunting. Ultrasound abdomen was suggestive of mild hepatomegaly (16.6cm), and both kidneys had mild enlargement, rest was within normal limits. 2D Echocardiography revealed perimembranous (pm) Ventricular Sepal Defect (VSD) (Left - Right shunt) Ruptured Sinus of Valsalva (RSOV) to Right Ventricular Outflow Tract (RVOT) with subaortic membrane with severe Aortic Stenosis (AS) and severe Pulmonary Arterial Hypertension (PAH) with evidence of vegetation. Blood culture was positive for Staphylococcus aureus on two separate occasions which was sensitive to Amikacin, Ceftriaxone, ciprofloxacin, Teicoplanin and Clindamycin. Patient was diagnosed to have Pm VSD (L - R shunt) RSOV to RVOT with subaortic membrane with severe AS with severe PAH with Infective Endocarditis (IE) and was promptly started on intravenous antibiotics and supportive management. Patient was simultaneously counselled about the disease condition and its poor prognosis and management. Patient was advised for surgical intervention. Patient developed hematuria on 5th day of hospital stay and there was progressive decline in renal function. Repeat urine examination was suggestive of active sediments with hematuria, pyuria with proteinuria with protein (+++), red blood cells/hpf- 29-30, 60%-70% dysmorphic, white blood cells/hpf- 15-20, casts/low power field - 2-3 fine granular, coarse granular, occasional WBC casts. Renal biopsy was done in view of active sediment which was suggestive of acute glomerulonephritis with interstitial nephritis secondary to infection [Table/Fig-1,2]. Patient was already on broad spectrum antibiotics and still the renal function and general condition of the patient was on the decline so the patient was started on intra-venous corticosteroids. His condition did not show improvement and he became progressively dyspnoeic and succumbed to his illness in the next two days.
Haematoxylin and Eosin stain section showing numerous polymorphonuclear leukocytes with PAS (Periodic Acid-Schiff)-positive cytoplasm. There is endocapillary proliferation with diffusely enlarged Glomeruli and hypercellularity due to neutrophils and macrophages and proliferation of mesangial and endothelial cells suggestive of post infectious glomerulonephritis.
Silver stain of renal section showing large number of polymorphonuclear leukocytes typical of post infectious glomerulonephritis with endocapillary proliferation.
Discussion
RSOV is an uncommon condition. Sinus of Valsalva aneurysms (SVA) can co-exist with other congenital disease and can rupture into the cardiac chambers, causing acute clinical symptoms. Rupture of a SVA occurs most commonly at the right ventricle (60%) or at the right atrium (29%), followed by the left atrium (6%) and left ventricle (4%) or at the pericardium (1%) [1,2]. Incidence of ruptured SVA in Eastern is 0.46%-3.5% and in Western areas is 0.14%-0.23% and its incidence is five times higher in Asian countries with male/female ratio as 4:1 [3]. The unruptured aneurysm often remain undiagnosed but may manifest with symptoms of right ventricular outflow obstruction.
SVA is a failure of the fusion between the aortic media and annulus fibrosus, and due to the increased pressure at the root of the aorta there occurs subsequent aneurysmal enlargement at this weak point over several years and thus it can remain subclinical for several years and usually manifests with rupture between the 3rd and 4th decade of life. The commonest sites of aneurysm rupture are cardiac chambers, interventricular septum [4], or pericardial space [5].
Transthoracic Echocardiogram (TTE) and Transesophageal Echocardiogram (TEE) have a diagnostic accuracy of 75% and 90%, respectively, for detection of ruptured or unruptured SVA [4] Surgical repair is required for both ruptured SVA and for symptomatic unruptured aneurysm compressing the adjacent tissues. Surgical treatments for SVA include direct suturing of the aneurysm or suturing with a patch [6].
Patients undergoing surgical repair have low operative risk and high long-term survival rates. Operative mortality is generally low (1%) in patients without infection [6]. However, cases of infected SVA (endocarditis or sepsis) have 4-5 times greater risk of perioperative death. Recent series have estimated a survival of 5 and 10 years after the correction of SVA of 97% and 82%, respectively [7]. Therefore, an early surgical intervention should be encouraged.
In multiple studies there has been co-existence of SVA with IE. Our patient was a definitive case of IE as per Duke’s modified criteria. The patient fulfilled two major criterias with endocardial involvement evident on 2D echocardiogram which showed presence of vegetations and blood culture positivity for Staphylococcus aureus on two separate occasions.
Renal involvement develops in about 20%-25% patients with IE, but mostly remains asymptomatic [8]. Patients presenting with deranged kidney function tests and heavy proteinuria is very uncommon. Multiple renal pathologies have co-existed in past with IE like infectious immune complex mediated glomerulonephritis, drug induced acute interstitial nephritis, embolic disease, focal necrotizing GN and crescentic GN [9].
In past, use of antibiotics like aminoglycosides, vancomycin and amphotericin-B for the treatment of IE primarily resulted in drug-induced acute interstitial nephritis but the incidence has decreased since the advent of better newer antibiotics. Renal biopsy is advised if there is presence of significant proteinuria or deranged renal function parameters or if there happens to be rapidly progressive renal failure. In many cases IE related complications resolve with appropriate antibiotics therapy alone but there have also been reports where corticosteroids, cyclophosphamide and plasmapheresis was used in view of non-improvement of renal condition [10–12].
Here, we report for the first time a rare presentation of RSOV and subaortic membrane with IE complicated by glomerulonephritis in a patient.
Conclusion
RSOV is a rare cardiac condition with fatal outcome, if left untreated. Surgical repair procedures for RSOV have low operative risk and high long-term survival rates and thus an early surgical intervention should always be encouraged in such patients. RSOV can be complicated with Infective Endocarditis and Glomerulonephritis. Though antibiotics alone have been sufficient in many cases but corticosteroids, cyclophosphamide and plasmapheresis can also be used if renal condition fails to improve.
[1]. Vautrin E, Barone-Rochette G, Philippe J, Rupture of right sinus of valsalva into right atrium: Ultrasound, magnetic resonance, angiography and surgical imagingArch Cardiovasc Dis 2008 101:501-02. [Google Scholar]
[2]. Missault L, Callens B, Taeymans Y, Echocardiography of sinus of valsalva aneurysm with rupture into the right atriumInt J Cardiol 1995 47:269-72. [Google Scholar]
[3]. Chu SH, Hung CR, How SS, Chang H, SS Wang, Tsai CH, Ruptured aneurysms of the sinus of valsalva in oriental patientsJ Thorac Cardiovasc Surg 1990 99:288-98. [Google Scholar]
[4]. Choudhary SK, Bhan A, Reddy SC, Sharma R, Murari V, Airan B, Aneurysms of sinus of valsalva dissecting into interventricular septumAnn Thorac Surg 1998 65:735-40. [Google Scholar]
[5]. Biabnam KR, Roberts WC, Fatal intrapericardial rupture of sinus of Valsalva aneurysmAm Heart J 1992 120:1455-56. [Google Scholar]
[6]. Pannu HS, Shivaprakash K, Bazez S, Geographical variations in the presentation of ruptured aneurysms of sinuses of valsalva: Evaluation of surgical repairJ Card Surg 1995 10:316-24. [Google Scholar]
[7]. Harkness J, Fitton T, Barreiro CJ, Alejo D, Gott VL, Baumgartner WA, A 32-year experience with surgical repair of sinus of valsalva aneurysmsJ Cardiac Surg 2005 20:198-204. [Google Scholar]
[8]. Neugarten J, Gallo GR, Baldwin DS, Glomerulonephritis in bacterial endocarditisAm J Kidney Dis 1984 3:371-79. [Google Scholar]
[9]. Haffner D, Schindera F, Aschoff A, Mathia A, Waldherr R, Scharer K, The clinical spectrum of shunt nephritisNephrol Dial Transplant 1997 12:1143-48. [Google Scholar]
[10]. Le Moing V, Lacassin F, Delahousse M, Duval X, Longuet P, Leport C, Use of corticosteroids in glomerulonephritis related to infective endocarditis: Three cases and reviewClin Infect Dis 1999 28:1057-61. [Google Scholar]
[11]. Mantan M, Sethi GR, Batra VV, Post-infectious glomerulonephritis following infective endocarditis: Amenable to immunosuppressionIndian J Nephrol 2013 23(5):368-70. [Google Scholar]
[12]. Couzi L, Morel D, Deminière C, Merville P, An unusual endocarditis-induced crescentic glomerulonephritis treated by plasmapheresisClin Nephrol 2004 62:461-64. [Google Scholar]