Corneal transparency is a vital predict for corneal function. After Penetrating Keratoplasty (PK) graft central thickness is relevant measurement because of the direct relationship between corneal hydration and corneal thickness. Corneal thickness stabilise by 3 months after PK at a median thickness of 0.54 mm. Central Corneal Thickness (CCT) is a predictor for outcome of PK. The greater the increase in thickness, the more likely the graft would fail [1].
Pre-operative corneal pathology influences the corneal thickness post-operatively with thinner host cornea in keratoconus and thicker corneas in Pseudophakic Bullous Keratopathy (PBK) [2].
Optical Coherence Tomography (OCT) is a recent imaging modality which allows high-resolution cross-sectional imaging of the ocular tissues [3]. The Anterior Segment Optical Coherence Tomography (AS-OCT) is of potential usefulness in evaluating the cornea at various tissue planes with high axial resolution after PK. AS-OCT was shown to be a valuable imaging tool for lamellar corneal transplantation [4]. The objectives of the present study were to analyse the changes in OCT after PK and to evaluate its relationship with pre-operative diagnosis.
Materials and Methods
The observational study was conducted at Himalayan Institute of Medical Sciences, Swami Rama Himalayan University, Dehradun, Uttarakhand, India. The study was approved was approved by institutional research ethical committee and was in accordance to the tenets set forth in Declaration of Helsinki. We retrospectively reviewed the records of 51 eyes of 50 patients who underwent optical PK and were examined for routine follow-up between December 2012 and June 2015.
Inclusion criteria: Adherent leucoma, PBK, corneal opacity or scarring, graft failure, anterior staphyloma and corneal dystrophy were the indications of PK which were included in the study.
Exclusion criteria: Patients younger than 16 years of age, post-tectonic and therapeutic grafts, low graft clarity< grade 3 and cases with multiple procedures besides PK were excluded from the study. Uncooperative subjects were also excluded from study.
Various parameters like age, sex of the patient (recipient), size of donor and host, grading of donor graft and indications of PK were noted. Best Corrected Visual Acuity (BCVA) with various methods like pinhole, glasses and rigid gas permeable lenses for high astigmatism, Intraocular Pressure (IOP), CCT and graft clarity were recorded post-operative on first day, 1, 3 and 6 months for all patients. Follow-up at six months was considered as last follow-up.
Surgical technique: All PK’s were performed under peribulbar anaesthesia with complete lids akinesia by single surgeon. Mackey- Kaufmann (MK) media preserved full thickness corneal graft was used within 96 hours. Manual trephination was done for both donor and recipient cornea. All donor grafts were oversized by 0.5mm 16 interrupted or continous 16 bites suturing was done by using 10-0 nylon suture.
The histopathological examination of recepient button and donor corneoscleral rim was done for all cases. Topical prednisolone 1% with topical antibiotic six times daily along with artificial tears were used as post-operative medication by all cases. Follow-up schedule was weekly for first month, biweekly for second month and monthly for 3 to 6 months for all cases.
Procedure: AS-OCT were performed for all the patients post-operatively at first post-operative day, 1 month, 3 and 6 months post PK to monitor CCT by using Fourier-Domain Optical Coherence Tomography (FD-OCT) system RTVue (Optovue, Inc, Fremont, CA, USA.). This OCT has speed of 26,000 axial scans per second with depth resolution of 5μm due to shorter wavelength of 830nm. A Corneal Adaptor Module (CAM) consisting of 2 adaptor lenses (a wide-angle or high-magnification lens) were used to provide telecentric scanning of anterior segment imaging. The wide-angle lens (long lens) was placed in front of the retinal objective lens to focus the OCT beam on the anterior segment provides a scan of width upto 6mm and a transverse resolution of 15 μm. Patients were asked to gaze at the fixating target within the OCT system after illuminating the anterior segment with two gooseneck lights.
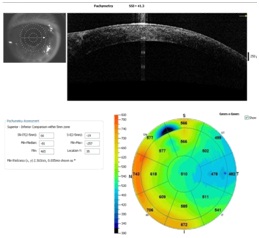
AS-OCT imaging was done by scan types of pachymetry (6mm x 6mm). Pachymetry comprised of 6mm radial lines on 8 meridians with this scanning pattern centred on the pupil or centre of the graft. The pachymetry map was divided into zones by octants (superior, superotemporal, temporal, inferotemporal, inferior, inferonasal, nasal, supernasal and annular rings (2, 5 and 6 mm diameters) [5]. The average corneal thickness of each zone was presented in zonal average maps as shown in [Table/Fig-1].
Depicting pachymetry maps.
The CCT’s at first post-operative day, 1, 3 and 6 months were evaluated for all the indications. For statistical analysis CCT was divided into 3 groups as group A, B and C for CCT in range of 400-550, 551-700 and >700μm respectively.
Statistical Analysis
Data were initially entered into an excel spreadsheet and then transferred to SPSS software (Statistical Package for Social Sciences, version 22.0, SPSS Inc, Chicago, IL) The quantitative factors like age, graft size, BCVA, IOP, CCT, keratometry and qualitative factors like indications of PK were included in the data. The descriptive statistics was used to express data in terms of frequency and percentage. Data were expressed in terms of means±standard deviations. As for few indications of keratoplasty number of units was less so Kruskal – Wallis test was used for comparison of means±standard deviations of CCT at first post-operative day, 1, 3 and 6 months. Chi square test was used to find out the association between indication of PK and CCT. The p-value < 0.05 was considered statistically significant.
Results
Fifty one eyes of 50 patients were reviewed in the present study. All cases had clear graft at time of enrollment. The age at which PKs were done ranged from 17-80 years (mean 51.64years ±SD 18.45 years). In this study, the number of men (35 of 50) was higher than women (15 of 50). Most frequent indication for PK was adherent leucoma 20(39.21%) followed by PBK 16(31.37%) [Table/Fig-2]. Left eye was involved in majority 30(58.82%) of cases. Mean CCT in cases of adherent leucoma on first post-operative day, 1, 3 and 6 months were 622.6 μm, 607.3 μm, 560.8 μm, 530.5 μm, respectively. Mean CCT in cases of PBK on first post-operative day, 1, 3 and 6 months were 640.5 μm, 595.13 μm, 563.06 μm and 525.68 μm, respectively.
| Indications of PK | n(%) |
|---|
| Adherent leucoma | 20(39.21%) |
| PBK | 16(31.37%) |
| Corneal opacity | 5(9.80%) |
| Graft failure | 6(11.76%) |
| Corneal dystrophy | 2(3.92%) |
| Anterior staphyloma | 2(3.92%) |
| Total | 51 (n) |
PK-Penetrating keratoplasty
PBK-Pseudophakic bullous keratopathy
The p-value by Kruskal-Wallis test for mean CCT in all indications on first post-day, 1, 3 and 6 months were 0.233, 0.200, 0.456, 0.834 respectively which were nonsignificant. On first post surgical day and on 6 month follow-up maximum mean CCT was observed in regrafts as 712±115.9μm and 594±144.7μm respectively. In the pre-operative diagnosis of corneal dystrophy, the maximum CCT was observed on 1 and 3 month follow-up as 748±13.4 μm and 635±20.5 μm, respectively.
The p-value for CCT in all indications on first post-day, 1, 3 and 6 months in different groups A(400-500), B(500-700) and C(≥700) were 0.442, 0.021, 0.725, 0.364, respectively. On first post surgical day and at 1 months follow-up maximum cases 36(70.58%) and 33(64.70%) had CCT in range of 551-700 μm, respectively. On 3 and 6 month follow-up maximum cases 28(54.90%) and 40(78.43%) had CCT of 400-500 μm, respectively [Table/Fig-3].
Depicting the association of various indications of PK with CCT groups at first postop day, 1 month, 3 and 6 months post PK.
| Indications of PK | Groups of CCT at various time period post PK |
|---|
| First post op | 1 month | 3 months | 6 months |
|---|
| A | B | C | A | B | C | A | B | C | A | B | C |
| Adherent leucoma | 3 | 13 | 4 | 5 | 12 | 3 | 12 | 6 | 2 | 15 | 5 | 0 |
| PBK | 0 | 14 | 2 | 4 | 11 | 1 | 9 | 7 | 0 | 13 | 3 | 0 |
| Corneal opacity | 0 | 4 | 1 | 2 | 3 | 0 | 3 | 2 | 0 | 5 | 0 | 0 |
| Graft failure | 0 | 3 | 3 | 3 | 6 | 0 | 3 | 2 | 1 | 4 | 1 | 1 |
| Corneal dystrophy | 0 | 1 | 1 | 0 | 0 | 2 | 0 | 2 | 0 | 1 | 1 | 0 |
| Anterior staphyloma | 0 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 0 | 2 | 0 | 0 |
| N (%) | 3 (5.8) | 36 (70.5) | 12 (23.5) | 12 (23.5) | 33 (64.7) | 6 (11.7) | 28 (54.9) | 20 (39.2) | 3 (5.8) | 40 (78.4) | 10 (19.6) | 1 (1.9) |
| p* value | 0.442 | 0.021 | 0.725 | 0.364 |
p* value - p-value by Chi-Square Tests
PK- Penetrating keratoplasty
CCT- Central corneal thickness
μm-micrometer
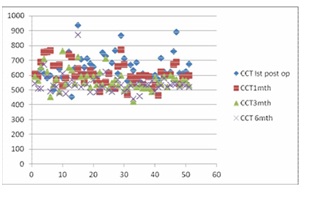
Changes in CCT according to post-operative time are shown in [Table/Fig-4]. Graft CCT significantly decreased between 1st post-operative day and 1 month. CCT further decreased in between 3 to 6 months post-operative time period post PK. The mean CCT at 1st post-operative day, 1, 3 and 6 month were 647.31±90.40 μm, 605.31±75.08 μm, 564.66±66.26 μm and 537.37±64.09 μm, respectively. Maximum CCT was seen on 1st post-operative day and minimum CCT was seen at 6 month irrespective of indications of PK. The CCT at 6 month post-surgery showed a strongly positive correlation with the IOP(r=0.66) and weakly positive correlation with BCVA (r=0.28).
Scatter diagram showing the changes in CCT at different time interval post PK.
Discussion
The adherent leucoma was the most common indication of PK in this study which is similar to the results of other published Indian studies. Bullous keratopathy was second common indication for PK in the present study of 16(31.37%) of total indications which is comparable to other studies [6,7].
Graft central thickness is considered to be a clinically relevant entity for post PK evaluation which indicates the graft hydration. Quantitatively, it is a useful method for evaluating corneal oedema. Vincent et al., reported the average graft central thickness of 558μm and 533 μm in successful transplants at 1 and 6 months respectively which was comparable to the present study which was in range of 551-700μm on 1 month and 400-550μm at 6 months follow-up. Corneal thickness recovered and normalised mainly by first 6 months post-operatively [8].
Kanellopoulos et al., concluded that one day post-operatively PK, the CCT was 785.81 ± 80.75 (688–943) μm which was comparable to thickness of 551-700 μm [9].
In the present study, CCT showed a typical pattern at first post-operative day and 1 month in which maximum patients were there in range of 551-700μm amongst all indications which amounts to 36(70.58%) and 33(64.70%) respectively. At 3 and 6 months post-operative time the CCT decreased in range of 400-550 μm with 28(54.90%) and 40(78.43%) in all indications, respectively.
In this present study, CCT decreased during the first three post-operative months from an average of 647μm at first post-operative day to an average of 565μm at 3 months, which is similar to observation of Collaborative Corneal Transplantation Studies [1]. Graft central thickness decreased during the first 3 post-operative months from an average of 0.645 mm at 1 week to an average of 0.541 mm at 3 months was reported by Vincent et al., [8].
Lass et al., reported a decrease in graft thickness from an average of 0.59 to 0.60 mm to an average of 0.52mm at 1 week to 3 months respectively [10]. In another study published by Lass et al., the average graft thickness had decreased from 0.69 to 0.70 mm at 1 week to 0.54 to 0.55 mm at 4 months [11]. Lindstrom et al., reported an average graft thickness of 0.69 mm at 1 day after surgery, decreasing to 0.54 mm after 3 months [12]. Bourne et al., in a series of 34 grafts reported a decrease in graft thickness from an average of 0.645 mm at 4 days to an average of 0.551 mm at 3 months [13]. Shinton et al., reported the median difference between total corneal thickness at day 1 and at last follow-up was 180 μm (95% CI 134 to 237, n=43) with reduction of 22% after DSEK [14]. In the present study the mean CCT at first post-operative day was 647.31±90.40 μm, and at 6 month follow-up was 537.37±64.09 μm with a difference of 110 μm. Shinton et al., reported that at 1 month post-operatively, the correlation between graft thickness and BCVA was very weak (rs=0.196) but 6 months post-operatively, there was a statistically significant correlation of moderate strength between graft thickness and BCVA (rs=0.460, p=0.041) [14]. In the present study at 6 months follow-up there was a strongly positive correlation between graft thickness and IOP but correlation between graft CCT and BCVA was also weakly positive which can be due to various other factors which play their role in visual outcome like suturing pattern, graft host alignment etc. In this study mean CCT in all indications at different time points were non-significant in omit similar way as pre-operative diagnosis had no significant influences on post-operative graft central thickness similar way as pre-operative diagnosis had no significant influences on post-operative graft central thickness [15].
Limitation
There are few limitations to the present study. Sample size of few indications was small. We did not assess the donor related factors like death to preservation time, death to utilisation time which may affect the graft thickness. Specular microscopy of donor endothelial cell count was lacking due to non-availability of this facility. Endothelial cell count of the graft after PK was also lacking in this study. Visual outcome assessment is based on BCVA but the data regarding astigmatism is not available for these patients.
Conclusion
Graft central thickness is considered to be quantitative method for evaluating corneal oedema post PK as it is good indicator of corneal hydration. AS-OCT is best non-invasive invivo method of investigation of CCT in post-operative period after PK. Graft CCT decreases during post-operative period of 6 months with significant decrease till one month post PK, without any influence of the pre-operative diagnosis. The CCT is strongly correlated to IOP but it shows weak correlation with BCVA as this is outcome of multiple factors.
PK-Penetrating keratoplasty
PBK-Pseudophakic bullous keratopathy
p* value - p-value by Chi-Square Tests
PK- Penetrating keratoplasty
CCT- Central corneal thickness
μm-micrometer