Temporomandibular Joint (TMJ) ankylosis is a situation in which the mandibular condyle is fused to the glenoid fossa by bone or fibrous tissue. The management of TMJ ankylosis has a complicated chore and it is challenging for the maxillofacial surgeon because of technical hitches and high rate of re-ankylosis. Interpositional gap arthroplasty is one of the modalities for its management. A range of inter-positional materials have been used to avert recurrence after gap arthroplasty in TMJ ankylosis. The aim of this series was to evaluate the effectiveness of the temporomyofacial flap in the treatment of TMJ ankylosis as an interpositional gap arthroplasty. A total of 10 cases with unilateral TMJ ankylosis were treated by interpositional gap arthroplasty by pedicled temporalis myofacial flap and evaluated with a follow-up of 6 months to 5 years (Mean 3.3 years) for the functional stability of TMJ. All the patients were successfully treated. There were no signs of recurrence in any patients up to last follow up visit. The result showed that temporalis myofascial flap is a preferable choice for inter-positional gap arthroplasty which proves its versatility as an inter-positional material.
Case Series
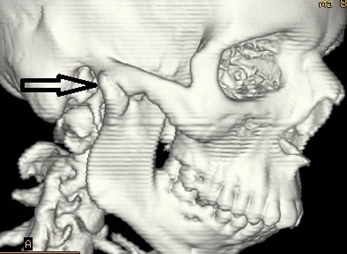
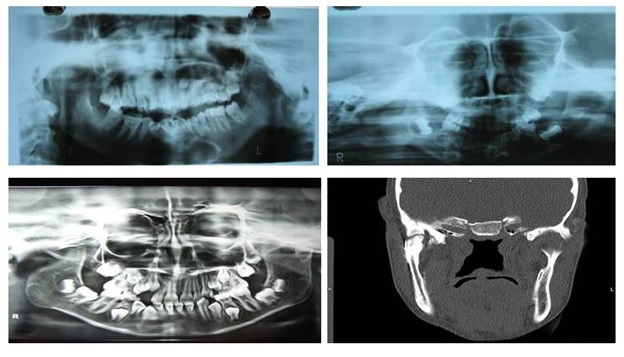
Total 10 patients with Temporomandibular Joint (TMJ) ankylosis reporting to the outpatient department of Oral and Maxillofacial Surgery, Maharaja Ganga Singh Dental College and Research Centre, Sri ganganagar, Rajasthan, India were included irrespective of age, sex, caste and socioeconomical status. Diagnosis of TMJ ankylosis was based on the basis of clinical assessment as Maximum inter-incisal Mouth Opening (MMO) [Table/Fig-1] and other cardinal signs of ankylosis [1] followed by radiographic assessment using Postero-anterior (PA) mandible view, Orthopantomogram (OPG), lateral oblique view and CT scan which showed various degrees of condylar involvement with condyles varying from normal size to a large spherical mass involving the condylar process as well as the coronoid process [Table/Fig-2].
Pre-operative maximum mouth opening.

3D CT scan showing ankylotic mass.
The patients were classified into three groups for an ease, based on the anatomic borders and the extent of ankylotic mass [1]:
Class 1: Ankylotic bony mass restricted to the mandibular condyle and glenoid fossa.
Class 2: Ankylotic bony mass extends out of the glenoid fossa involving the medial aspect of the skull base.
Class 3: Extension into the middle cranial fossa.
In our study, out of 10 cases, 8 cases belonged to class 1 and 2 cases belonged to class 2.
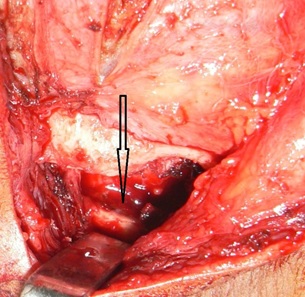
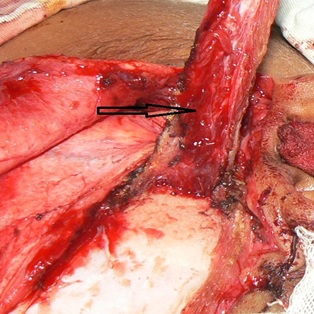
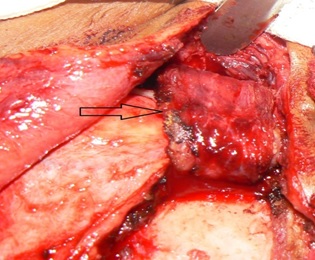
Surgical Procedure: All patients were operated under general anesthesia after written informed consent. Classical pre-auricular and Al-Kayat and Bramely’s modified pre-auricular incision were made as indicated to gain access to TMJ region of involved side [Table/Fig-3] [2,3]. Layer by layer dissection was carried out until superficial temporal fascia was reached. Superficial temporal fascia dissected out and retracted anteriorly to avoid injury to facial nerve. Periosteum over zygomatic arch was dissected and care was taken to avoid injury to superficial temporal artery and vein too. Ankylotic mass was exposed and belligerent excision of bony mass was carried out by chisel and bur with the gap of at least 10-15 mm between the floor of the glenoid fossa and the mandible [Table/Fig-4,5]. The glenoid fossa was recontured and shaped as necessary. Following excision of the bony mass the MMO of 30-35mm was achieved passively. In accordance with the protocol for TMJ ankylosis (1990, 2009) [4,5] contralateral coronoidectomy was performed in 4 cases through intra-oral approach when mouth opening was less than 35mm intra-operatively. Finger shaped composite temporal myofascial flap (includes temporalis muscle and fascia).
Classical pre-auricular Alkayat Bramely’s incision.


As shown in [Table/Fig-6] the length and width of the flap was marked and decided according to the need so that it can be rotated and reached to the joint space without any gratuitous stretching. The flap was rotated over the zygomatic arch and was sutured anteriorly, posteriorly and medially so that it covers the arthroplasty site completely and proficiently. Layer by layer suturing was carried out and surgical drain was placed [Table/Fig-7]. Physiotherapy was started from the first post-operative day with jaw exercises under supervision [Table/Fig-8]. It was intensified gradually in the post-operative and recall period and MMO was noted at regular follow-up maximum up to 5 years. Aggressive physiotherapy was carried out in subsequent visits [Table/Fig-9].
Temporalis myocutaneous fascia flap.
Interpostional gap arthroplasty with rotation of temporalis myocutaneous fascia flap.
Primary closure and surgical drain in place.

Post-operative maximum mouth opening.

Results: A total of 10 patients with TMJ ankylosis were successfully treated by interpositional gap arthroplasty. Mean age of the patients was 8.6 years. All the patients had a history of trauma to the TMJ which could be the aetiological factor for TMJ ankylosis. Patients had pre-operative maximal mouth opening at incisal edges of 1-11mm, (mean 6.8mm). Patients had maximum mouth opening of 30-38mm (mean 34.5mm) on last follow-up (mean 4.1 years). Transient paraesthesia of the temporal branch of facial nerve was observed in 1 case which was recovered within 3 months by conservative treatment. Periodic OPGs were obtained to check the maintenance of the intra-articular space [Table/Fig-10]. There were no signs of recurrence in any patients up to last follow-up visit [Table/Fig-11]. Overall results of all the cases have been described in [Table/Fig-12].

Post-operative X-rays show no signs of recurrence.
Summarization of overall results.
| Patient | Age | Sex | Involved Joint Side | Pre-Op | MMO (mm) | At Last Follow-Up | Coronoidectomy | Transient Paresthesia of Temporal Branch of Facial Nerve | Follow- Up in Years |
|---|
| 1 | 17 | M | LEFT | 3 | | 33 | NO | NO | 5 |
| 2 | 23 | F | LEFT | 7 | | 38 | YES | NO | 5 |
| 3 | 24 | F | RIGHT | 3 | | 34 | NO | NO | 4.5 |
| 4 | 6 | M | RIGHT | 2 | | 39 | NO | NO | 4 |
| 5 | 14 | M | LEFT | 8 | | 40 | YES | NO | 5 |
| 6 | 15 | F | LEFT | 3 | | 35 | YES | NO | 4.5 |
| 7 | 11 | F | LEFT | 4 | | 34 | NO | YES | 2.5 |
| 8 | 9 | M | RIGHT | 5 | | 35 | NO | NO | 3 |
| 9 | 12 | F | RIGHT | 7 | | 36 | NO | NO | 3.5 |
| 10 | 13 | F | RIGHT | 8 | | 32 | YES | NO | 4 |
M: male, F: female, MMO: maximal mouth opening, mm: millimeter, Pre-op: pre operative, Imm. post-op: immediate post operative.
Discussion
The TMJ is a very complex joint of human body. It has intricate structural components and it behaves in a unique way during its bilateral movements. It’s the only synovial joint with articular disk. During chewing, it sustains an enormous amount of pressure. Ankylosis of the TMJ is defined as a situation in which the mandibular condyle is fused to the glenoid fossa by bone or fibrous tissue causing loss of function of TMJ [3]. Ankylosis is most frequently caused by trauma, local or systemic infection, congenital anomalies and systemic diseases. It can be classified by a grouping of location (intra- or extra-articular), type of tissue involved (bony, fibro-osseous) and extent of fusion (complete, incomplete) [4,5]. It can be classified simply as true or false. True TMJ ankylosis is a situation that results in intra-articular bony or fibrous union between the articulating surfaces of the TMJ; whereas, false ankylosis is an extra-articular condition [3]. TMJ ankylosis presents as a strict physical and emotional disability of the affected individual. It affects the mastication, communication, oral hygiene, overall facial appearance and in advance stages it also causes airway difficulty too. The clinical expression of TMJ ankylosis depends upon time of onset, aetiology and extension of involvement of one or both joints. It may present in mild forms as restricted mouth opening to severe forms causing the facial asymmetry and airway difficulty [6–8]. The aim of managing such a patient should be to establish movement, function of the jaw, avoid relapse, refurbish appearance and achieve normal growth and occlusion if in child. Management of such patients is best done via gap arthroplasty in which condylectomy is done creating a gap of 1-1.5cm with interpositional grafting. Many inter-positional autogenous, allogenic and xenografts have been used for the inter-positional grafting. Autogenous tissues like articular disk, temporalis muscle and fascia, fascia lata, skin, human amniotic memebrane, fat, auricular cartilage, costochondral graft etc., have been used. Alloplastic substances like wooden block, gold foils, acrylic blocks, silastic, teflon and proplast have also been used [9]. Temporalis fascia flap was first described by Yolovine in 1898 [10]. He used it for orbital reconstruction. It was first used by Murphy in 1912 for the surgery of TMJ [11].
The management of TMJ ankylosis is one of the exigent procedures for a maxillofacial surgeon because of complexity of the TMJ region and high recurrence rate. Different techniques for the surgical management of TMJ ankylosis have been described that includes gap arthroplasty, inter-positional arthroplasty and TMJ reconstruction but none has proved exclusively acceptable [12,13]. The typical pathogenesis of ankylosis is the development of a bony bunch, which replaces the TMJ articulation, resulting in limitation of mandibular movements. So treatment of TMJ ankylosis needs removal of an adequate amount of bone/bony mass to allow for free movement of the mandible [14–16]. Arthroplasty without interposition requires a gap of 10-20mm and often result in deviation of mouth and also has a higher recurrence rate of about 53% due to osteoblastic growth between the abraded bone surfaces [6]. Therefore, it is better to create a minimal gap (10mm) and then perform inter-positional gap arthroplasty to prevent recurrence [15].
Selection, application and success of the inter-positional material are the points of debate among all surgeons. The drawbacks of various materials respectively are that the temporalis muscle shows some amount of degeneration and gets fibrosed which aggravates trismus [9,15,16]. Fascia lacks in volume; chondral graft shows resorption, infection and calcification, while the alloplastic implants used for reconstruction corrode, break-up and cause foreign body giant cell reaction under functional loads [9]. Thus, TMJ reconstruction with various autogenous and alloplastic materials have common complications like re-ankylosis, resorption, overgrowth, fracture, and pain. Secondary surgical site morbidity, complications and dubious long-term outcomes must be taken into consideration in all the methods of functioning TMJ reconstruction [13–16].
The pedicled temporalis myofascial flap has the following advantages over other methods of reconstruction of TMJ: Close proximity to the TMJ without involving a supplementary surgical site, satisfactory blood supply, autogenous origin; thus, lacks antigenesity and toxicity, maintenance of attachment to the coronoid process which provides movement of the flap during function, simulating physiologic action of the disc. Its proximity to the joint allows for a pedicled transfer of vascularized tissue into the joint area, exihibit a low degree of friction and positional stability [17–20].
In the present series pedicled temporalis myofacial flap was used as an inter-positional material in gap arthroplasty in 10 cases and satisfactory results were found post-operatively without recurrence at long follow-up period which is concurrent to other studies [9–13,17–26] [Table/Fig-13]. At the same time early aggressive and harsh post-operative physiotherapy exercises for mouth opening are mandatory in each patient to prevent re-ankylosis or recurrence. The middle temporal artery which is a branch of a superficial temporal artery supplies mainly to the temporalis fascia and posterior part of the muscle. The superficial temporal artery is located within the superficial temporal fascia and vein lies on its outer surface. While harvesting temporalis muscle or the fascia if the superficial temporal vessels are severed then this could be one of the reason for failure of flap. Results of our study indicate that the temporalis fascia survives when it is carefully dissected to preserve blood supply. The fate of temporalis muscle graft was studied and demonstrated by magnetic resonance imaging and conclusion was made that the flaps appeared to be viable and the tissue signal was compatible with vital muscle [20–26]. The limitations of the temporalis myofacial flap in inter-positional gap arthroplasty are degeneration of the fibrous tissue causing trismus and re-ankylosis, if post-operative aggressive physiotherapy is not followed and loss of ramus height. The results of various studies of inter-positional gap arthroplasty by temporalis fascia flap alone or in combination for the treatment of TMJ ankylosis are shown in [Table/Fig-13].
Results of various studies of interpositional gap arthroplasty by temporalis fascia flap alone or in combination for the treatment of TMJ ankylosis.
| Sr. No | Author | Year | No. of patients included | Pre-operative MMO* in mm | Post-operative MMO in mm | Follow-up period in years | Recur-rence rate |
|---|
| 1. | Pogrel MA and Kaban LB [14] | 1990 | 16 | 2-30 | 21-40 | 1-3 | 0% |
| 2. | Umeda et al., [23] | 1990 | 25 | - | - | 0.5-5.5 | 16% |
| 3. | Herbosa and Rotskoff [19] | 1990 | 15 | <20 | 35-45 | 1-2 | 0% |
| 4. | C. Chossegros et al., [17] | 1997 | 6 | 2-20 | 30-40 | 3-20 | 17% |
| 5. | Su-Gwan [9] | 2001 | 7 | 9-20 | 34-39 | 1-2.5 | 0% |
| 6. | Mani and Panda [15] | 2003 | 15 | - | - | 0.5-2.5 | 0% |
| 7. | Danda AK [25] | 2009 | 8 | 2-6 | 7-42 | 2 | 12.5% |
| 8. | Bulgannawar BA et al., [26] | 2011 | 8 | 1-9 | 32-40 | 6 | 0% |
| 9 | Karamese M et al., [21] | 2013 | 11 | 4-7 | 13-26 | 3-5 | 0% |
* MMO- maximum mouth opening
Conclusion
Inter-position of the temporalis myofacial flap in gap arthroplasty has superior results than other non-vascular interpositional graft and reconstruction materials in terms of functional stability of joint, recurrence and economical which proves its versatility in the management of TMJ ankylosis.
M: male, F: female, MMO: maximal mouth opening, mm: millimeter, Pre-op: pre operative, Imm. post-op: immediate post operative.
* MMO- maximum mouth opening
[1]. Movahed R, Mercuri LG, Management of temporomandibular joint ankylosisOral and Maxillofac Surg Clin of North America 2015 27(1):27-35. [Google Scholar]
[2]. Al-Kayat Bramley P, A modified pre-auricular approach to the temporomandibular joint and malar archBr Jour of Oral Surg 1979 17(2):91-103. [Google Scholar]
[3]. El-Mofty S, Ankylosis of the temporomandibular jointOral Surg Oral Med Oral Pathol 1972 33(4):650-60. [Google Scholar]
[4]. Kaban L, Perrott D, Fisher K, A protocol for management of temporomandibular joint ankylosisJ Oral Maxillofac Surg 1990 48(11):1145-51. [Google Scholar]
[5]. Kaban L, Bouchard C, Troulis M, A protocol for management of temporomandibular joint ankylosis in childrenJ Oral Maxillofac Surg 2009 67(9):1966-78. [Google Scholar]
[6]. Roychoudhury A, Parkash H, Trikha A, Functional restoration by gap arthroplasty in temporomandibular joint ankylosisOral Surg Oral Med Oral Pathol Oral Radiol Endod 1999 87(2):166-69. [Google Scholar]
[7]. Kazanjian V, Temporomandibular joint ankylosis with mandibular retrusionAm J Surg 1955 90(6):905-10. [Google Scholar]
[8]. Laskin D, Role of the meniscus in the etiology of post-traumatic temporomandibular joint ankylosisInt J Oral Surg 1978 7(4):340-45. [Google Scholar]
[9]. Su-Gwan K, Treatment of temporomandibular joint ankylosis with temporalis muscle and fascia flapInt J Oral Maxillofac Surg 2001 30(3):189-93. [Google Scholar]
[10]. Yolovine SS, Procede de cloture plastique de l’orbit apres l’extenterationArch d’Ophthamol 1898 18:679 [Google Scholar]
[11]. Murphy JB, Bony ankylosis of jaw with interposition of flaps from temporal fasciaSurg Clin 1913 2:659 [Google Scholar]
[12]. Majmudar A, Bainton R, Suture of temporalis fascia and muscle flaps in temporomandibular joint surgeryBr J Oral Maxillofac Surg 2004 42:357 [Google Scholar]
[13]. Raveh J, Vuillemin T, Ladrach K, Sutter F, Temporomandibular joint ankylosis: Surgical treatment and long-term resultsJ Oral Maxillofac Surg 1989 47:900 [Google Scholar]
[14]. Pogeral MA, Kaban LB, The role of a temporalis fascia and muscle flap in temporomandibular joint surgeryJ Oral Maxillofac Surg 1990 48:14 [Google Scholar]
[15]. Mani V, Panda AK, Versality of temporalis myofascial flap in maxillofacial reconstruction-analysis of 30 casesInt J Oral Maxillofac Surg 2003 32:368 [Google Scholar]
[16]. Cheung LK, The vascular anatomy of the human temporlis muscle: Implications for surgical splitting techniquesInt J Oral Maxillofac Surg 1996 25:414 [Google Scholar]
[17]. Chossegros C, Guyot L, Cheynet F, Blanc L, Gola R, Bourezak Z, Conrath J, Comparison of different materials for interposition arthroplasty in treatment of temporomandibular join ankylosis surgery: Long-term follow-up in 25 casesBr J Oral Maxillofac Surg 1997 35:157 [Google Scholar]
[18]. Feinberg SE, Larsen PE, The use of a pedicled temporalis muscle-pericranial flap for replacement of the TMJ disc: Preliminary reportJ Oral and Maxillofac Surg 1989 47:142-46. [Google Scholar]
[19]. Herbosa EG, Rotskoff KS, Composite temporalis pedicle flap as an interpositional graft in temporomandibular joint arthroplasty: A preliminary reportJ Oral Maxillofac Surg 1990 48(11):1049-56. [Google Scholar]
[20]. Cheung Lim-Kwong, "The vascular anatomy of the human temporalis muscle: Implications for surgical splitting techniques."Int J Oral Maxillofac Surg 1996 25(6):414-21. [Google Scholar]
[21]. Karamese M, Duymaz A, Seyhan N, Keskin M, Tosun Z, Management of temporomandibular joint ankylosis with temporalis fascia flap and fat graftJ of Cranio-Maxillofac Surg 2013 41(8):789-93. [Google Scholar]
[22]. Omura S, Fujita K, Modification of the temporalis muscle and fascia flap for the management of ankylosis of the temporomandibular jointJ Oral Maxillofac Surg 1996 54(6):794-95. [Google Scholar]
[23]. Umeda H, Kaban LB, Pogrel MA, Stren M, Rotskoff KS, Long-term viability of temporalis muscle/fascia flap used for temporomandibular reconstructionJ Oral Maxillofac Surg 1993 51(5):530-34. [Google Scholar]
[24]. Al-Moraissi EA, El-Sharkawy TM, Mounair RM, El-Ghareeb TI, A systematic review and meta-analysis of the clinical outcomes for various surgical modalities in the management of temporomandibular joint ankylosisInt J Oral Maxillofac Surg 2015 44(4):470-82. [Google Scholar]
[25]. Danda AK, Ramkumar S, Chinnaswami R, Comparison of gap arthroplasty with and without a temporalis muscle flap for the treatment of ankylosisJ Oral Maxillofac Surg 2009 67(7):1425-31. [Google Scholar]
[26]. Bulgannawar BA, Rai BD, Nair MA, Kalola R, Use of temporalis fascia as an interpositional arthroplasty in temporomandibular joint ankylosis: Analysis of 8 casesJ Oral Maxillofac Surg 2011 69(4):1031-35. [Google Scholar]