Fiberoptic Guided Retrograde Intubation in an Anticipated Difficult Airway: Revival of an Antiquated Technique
Samarjit Dey1, Marie Ninu2, Md. Yunus3, Newstar Syiemiong4
1 Assistant Professor, Department of Anaesthesiology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, India.
2 Senior Resident, Department of Anaesthesiology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, India.
3 Additional Professor, Department of Anaesthesiology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, India.
4 Senior Resident, Department of Anaesthesiology, North Eastern Indira Gandhi Regional Institute of Health and Medical Sciences, Shillong, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Samarjit Dey, 105, Department of Anaesthesiology, NEIGRIHMS, Shillong-793018, Meghalaya, India.
E-mail: drsamar0002@gmail.com
Retrograde intubation is an invaluable technique which can be helpful in anticipated difficult airway situation. In this advanced era where fiberoptic intubation and video laryngoscopes are in abundant use, retrograde intubation is a forgotten technique. However, it may be useful in various difficult airway situations in this advanced era. In our case the patient had a bitter experience with previous fiberoptic intubation. Owing to that we had planned and performed a fiber optic guided retrograde intubation, where we had kept the fiberoptic bronchoscope in the pharynx keeping larynx and vocal cords in the focus to facilitate the emergence of guide wire through one of the nostrils as well as direct visual confirmation of intubation. This fiber optic guided retrograde intubation is a first reported case of its kind in a predicted difficult airway which can be beneficial in different difficult airway situations.
Bronchoscope, Pharynx, Tuberculous osteomyelitis
Case Report
A 30-year-old female patient presented with difficulty in opening mouth for 19 years. The symptoms started gradually and were progressive in nature. There was no associated pain while trying to open her mouth. She was diagnosed with tuberculous osteomyelitis (spine) in 1997 and completed treatment, following which she started developing difficulty in opening mouth and diagnosed with temporomandibular joint fibrosis. She underwent surgery for the same complaint in 2003 after which she felt better and could open her jaw up to some extent but the symptoms gradually recurred. No significant past and family history was noted.
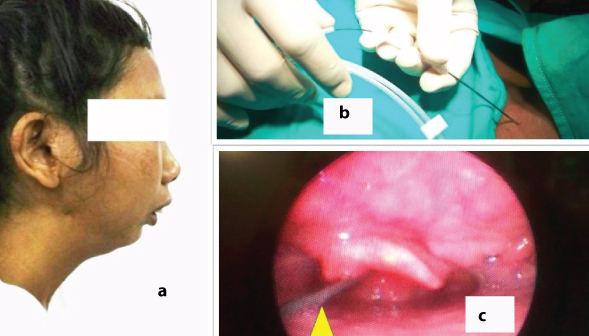
She had severe restriction in opening her mouth. No tenderness was noted at the temporomandibular (TM) joint. No abnormality was noted on her general physical and systemic examination. There was inadequate mouth opening (maximum 1 finger), retracted mandible [Table/Fig-1a]. Thyromental distance was 6.5cm there was hardly any space for TM joint opening up because of the fibrosis. Normal extension and flexion of neck were noted. Mallampati grading could not be assessed. Patient was planned for release of fibrosis and mobilization of temporomandibular joint.
(a) Lateral view of the patient with retracted mandible; (b) Introduction of guide wire through tuhoy needle; (c) Fiberoptic view of the retrograde guidewire.
Pre-operatively she was counseled and explained about the procedure. Consent was obtained for the same. She was nebulized with 4% lignocaine. After xylometazoline drops, nasal pellets soaked with Lignocaine 2% (with adrenaline 1:200000) were placed in both nostrils in the pre-operative room. Inj Glycopyrrolate 0.2mg IV was given in the pre-operative area. Inj Midazolam 1mg IV was given after connecting all the ASA standard monitors. Bilateral superior laryngeal block was given with 2% lignocaine on both sides followed by trans-tracheal block with 4% lignocaine. It was confirmed by aspiration of air bubble and coughing during and after injection. Oral cavity was sprayed with 10% lignocaine. The total dose of Lignocaine was kept within 5mg/kg.
Nasopharyngeal airway size 7mm was lubricated and inserted through right nostril. Another nasopharyngeal airway (6.5mm) was connected to breathing circuit via a 5mm ET tube connector and supplemental oxygen was given @8liter/min. Flexible fiberoptic bronchoscope was inserted through right nostril (through the nasopharyngeal airway) and was kept in the pharynx with epiglottis and vocal cords in view. The cricothyroid membrane was identified externally and after infiltration a Tuohy needle (18G) was inserted through the membrane with bevel end facing cephalad direction [Table/Fig-1b].
A DJ stent guide wire was inserted through Tuohy needle under fibreoptic guidance [Table/Fig-1c] and was directed and brought out through left nostril under fiberoptic guidance. An intubating bougie was then railroaded over the guide wire through the left nostril. Once the bougie was in place the guide wire was removed. A 6.5mm ID cuffed endotracheal tube was then inserted over the bougie into the trachea and simultaneously confirming by fiberoptic bronchoscope. The bougie was removed and the ventilator circuit attached to the tube and position confirmed by auscultation and capnography. Meanwhile inj Propofol 100mg i.v., inj Vecuronium 5mg IV given. Inhalational was initiated. Inj Paracetamol 1g IV, Inj Palonosetron 0.075mg i.v. given. Procedure was uneventful. Patient tolerated the awake fiberoptic guided retrograde intubation well. Surgery was uneventful. She was reversed with 0.5mg inj Glycopyrolate IV and inj Neostigmine 2.5mg IV and then shifted to post-operative area with postoperative advice.
Discussion
Difficult airway if not managed properly may lead to significant morbidity or even mortality. However, there are various procedures to tackle the difficult airway. American Society of Anesthesiologists and Difficult Airway Society have described a stepwise and plan wise approach to difficult airway management [1]. Retrograde intubation technique was first reported by D.J. Waters in 1963 [2]. The use of retrograde wire technique to assist in the management of difficult airway was first reported in 1981. Since that period, different modifications of retrograde technique have been tried and it also included the use of the fiberoptic bronchoscope as described by Roberts KW et al., to assist tracheal intubation under direct visual control [3]. Here we have revived the neglected retrograde intubation technique with a touch of fiberoptic guidance, which proved comfortable to the patient also.
Owing to the emergence of new equipments for intubation such as laryngeal mask airway, fibreoptic bronchoscope, airway bougie, lighted stylet, combitube and video laryngoscopy, the retrograde intubation was somehow put aside in the management of predictable and non–predictable difficult airways [4].
Harris et al., concluded that retrograde intubation is not widely taught and also this technique is felt by some to be an antiquated technique in a world of fiberoptic visualization tools [5].
The advantages of retrograde intubation over fibreoptic bronchoscope-guided intubation include its applicability when blood and secretions are present in the upper airway, shorter procedural duration and a lower risk of subglottic oedema and stenosis [4]. A Hussain et al., reported a case of Retrograde-Assisted Fiberoptic Intubation [6]. He had used the suction port of the fiberscope to pass the guide wire during retrograde intubation.
Dhanyee et al., reported a case of wire guided fireoptic retrograde intubation in a case of glottis mass, in which there was a mass, occupying most of the supraglottic space, with no visible airway (as seen via fiberoptic bronchoscope) [7]. It was oedematous, friable and they were reluctant to push the fibreoptic bronchoscope past it blindly. So, they had used a fiberoptic guided retrograde intubation.
In our case, we had planned for an retrograde intubation using a DJ stent wire under fiberoptic visualisation so that we could visualize the guide wire passing through nostrils, which is also a difficult step and most of the time it is difficult to negotiate a preformed endotracheal tube over the guide wire So, we had railroaded a bougie over the guide wire first then once the bougie was placed inside vocal cords ET tube was pushed over it into the vocal cords. Retrograde intubation should be taught and practiced as we may not know when and where it may be useful to us.
Conclusion
Fiberoptic guided awake retrograde intubation is an alternative option for anticipated as well unanticipated difficult airway and should widely be practiced and taught to acquire and retain the skill.
[1]. Sasanka S, Aids to tracheal intubationAnaesthesia update 2003 17:1 [Google Scholar]
[2]. Waters DJ, Guided blind endotracheal intubation. For patients with deformities of the upper airwayAnaesthesia 1963 18:158-62. [Google Scholar]
[3]. Roberts KW, Solgonick RM, A modification of retrograde wire–guided fiberoptic-assisted endotracheal Intubation in a patient with ankylosing spondylitisAnaesth Analg 1996 82:1290-91. [Google Scholar]
[4]. Vieira D, Lages N, Dias J, Maria L, Correia C, Retrograde intubation: an old–new techniqueOA Anaesthetics 2013 1(2):18 [Google Scholar]
[5]. Harris EA, Arheart KL, Fischler KE, Does the site of anterior tracheal puncture affect the success rate of retrograde intubation? A prospective, manikin-based studyAnesthesiol Res Pract 2013 2013:354317 [Google Scholar]
[6]. Hussain A, Ahmad N, Channa A, Retrograde-assisted fiberoptic intubation: An unusual but useful use of flexible fiberoptic endoscopeThe Internet Journal of Anesthesiology 2003 8:2 [Google Scholar]
[7]. Dhanyee AS, Pillai R, Sahajanandan R, Wire guided fibreoptic retrograde intubation in a case of glottic massIndian J Anaesth 2016 60:219-21. [Google Scholar]