Efficacy of Transcutaneous Electrical Nerve Stimulation in the Treatment of Overactive Bladder
Nidhi Sharma1, Kaja Rekha2, Krishnamurthy Jayashree Srinivasan3
1 Associate Professor, Department of Obstetrics and Gynaecology, Saveetha Medical College, Chennai, Tamil Nadu, India.
2 Tutor, Department of Cardiopulmonary Physiotherapy, Saveetha College of Physiotherapy, Chennai, Tamil Nadu, India.
3 Head of the Department, Department of Obstetrics and Gynaecology, Saveetha Medical College, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Nidhi Sharma, No 5, Jayanthi Street, Dr Seethapathi Nagar, Velachery, Chennai-600042, Tamil Nadu, India.
E-mail: drbonuramkumar@yahoo.co.in
Introduction
Overactive Bladder (OAB) accounts for 40-70% cases of incontinence. The etiology is unknown though detrusor instability is found in urodynamic evaluation of almost all cases. Detrusor instability or hyperreflexia can be inhibited by direct inhibition of impulses in the pre-ganglionic afferent neuron or by inhibition of bladder pre-ganglionic neurons of the efferent limb of micturition reflex. Transcutaneous Electrical Nerve Stimulation (TENS) is based on the gate control theory of abolishing the local micturition reflex arc.
Aim
To assess the effectiveness and safety of TENS in idiopathic OAB.
Materials and Methods
It is a prospective experimental study to evaluate the effectiveness of TENS v/s placebo in reducing OAB symptoms. (n1=20, n2 =20). Ten treatment sessions (5 sessions/week) of 30 minutes, were conducted.
Results
There was a significant improvement in Overactive Bladder Symptom Scores (OABSS) in TENS group and 2 patients were completely dry following TENS therapy.
Conclusion
In elderly women, patients with OAB where other co-medications have their own anticholinergic side effects and impairment of cognition is a concern, TENS can be a useful intervention. TENS units are safe, economical and easily commercially available.
Detrusor instability, Gateway control, Urinary incontinence
Introduction
Overactive Bladder (OAB) accounts for 40-70% cases of incontinence [1,2]. OAB syndrome is a syndrome complex characterized by urinary urgency (frequent feeling of need to void). This may or may not be associated with urge associated urinary incontinence [3,4].
Urgency signifies a sudden severe desire to void (detrusor instability). If the patient can override this by contracting the external sphincter and pelvic diaphragm the instability is aborted (clinically urgency, pathophysiology detrusor hypereflexia). If the patient is not able to contract the external sphincter and pelvic diaphragm the urgency is converted to urge incontinence (clinically urge incontinence, pathophysiology detrusor-external sphincter dyssynergia).
In a few cases of OAB, the patient leaks 15-20 seconds after performing the valsalva manoeuver, demonstrating stress incontinence. In these cases the urodynamic studies reveal involuntary detrusor contractions, induced by valsalva manoeuver, and hence the leak continues even after the stress is over. This is termed as “stress induced detrusor hyperreflexia.”
The etiology is unknown though several precipitating factors (chronic cystitis, genital prolapse, senile atrophic vaginitis, bladder calculi, carcinoma in situ or transitional cell carcinoma of the bladder) have been identified [5,6]. It is also important to realize that the detrusor instability is a disease of spontaneous exacerbations and remissions that may require intermittent rather than continuous therapy [7].
The first line therapy according to international guidelines is life style modifications and behavior therapy in combination with antimuscurinic drugs [3,4]. Unfortunately, most patients are middle to old age and do not tolerate anticholinergic side effects like dry mouth and constipation [8,9]. This study was designed to assess the effectiveness and safety of Transcutaneous Electrical Nerve Stimulation (TENS) in idiopathic OAB. TENS is based on the gate control theory of abolishing the local micturition reflex arc [10]. But the exact optimal stimulation required in bladder dysfunction is unknown [11]. It is a non-pharmacological method of inhibiting the presynaptic afferent neurons carrying impulses from bladder by stimulating the nerves of peripheral segmental dermatome (gate control theory of electro modulation by stimulating the peripheral nerves corresponding to the visceral organ). It acts at the level of primitive voiding reflex coordinating the bladder, sphincter and the pelvic floor. Detrusor hyperreflexia can be inhibited by direct inhibition of impulses in the preganglionic afferent neuron or by inhibition of bladder preganglionic neurons of the efferent limb of micturition reflex. Recently, the role of increased serum nerve growth factor and adipokinases in the pathophysiology of OAB syndrome refractory to anti-muscurinics has been proved [12–14]. It has also been hypothesized that the TENS works by improving the local vascularity and a possible inhibition of sympathetic impulses by the release of brain endorphins [15–17].
Aim
To evaluate the effectiveness of TENS v/s placebo in reducing OAB symptoms.
Materials and Methods
It was a prospective experimental study conducted in the Department of Obstetrics and Gynecology at Saveetha Medical College, Chennai from Jan 2015 to Jan 2016. There were two groups, 20 each in control and TENS group.
We had obtained the patients’ consent for participation in research and ethical committee clearance along with research board clearance was obtained for the study. The placebo group was also treated with the TENS therapy after the conclusion of study according to the Principle of HELSINKI.
Inclusion criteria were women with OAB not responding to lifestyle changes and behavioral therapy in the age group of 18-60 years. Patients with known pelvic pathology, pregnancy or any medication for chronic renal diseases were excluded from the study.
Twenty patients with a clinical diagnosis of OAB were treated with square wave biphasic pulse of frequency 75-100 Hz with a current density on 4 cm square. Ten treatment sessions (5 sessions/week) of 30 minutes, were conducted. The electrodes were applied on bladder dermatome S2, S3 and S4 in the lower back after explaining the procedure. The electrode skin impedance was minimized by applying a generous layer of electrode gel to promote good contact under entire electrode. The participants were given 5 sittings per week for 2 weeks. Twenty cases of OAB were taken as controls on placebo. For ensuring the blinding of participants, TENS electrodes were attached to the control group as in the study group but no current was delivered. Pre and post questionnaires (OABSS) were used. [Appendix 1]. Patients were instructed to circle the score that best applied during the last week.
Statistical Analysis
Statistical analysis was done using student’s paired t-test, Wilcoxon Sign rank test and Mann-Whitney U test using SPSS package. The confidence interval was 99.99 and p value 0.0001 for paired t-test.
Results
The mean age of the 40 patients was 48 years (range 18-60). Case groups were comparable to controls in relation to age, parity and total pre-experimental OABSS score. TENS showed an improvement in the study group. In the treatment groups there was a reduction in the diurnal voiding frequency (OABSS Question 1) from pretest scores (1.49±0.69) to (0.45±0.51) in the post TENS group. This was a statistically significant reduction (p-value= 0.0001, t = 6.8920, SED = 0.145). In control group, the reduction in the voiding frequency from pretest scores (1.20±0.41) to (0.55±0.60) in the post placebo group. This was also a statistically significant reduction (p-value= 0.0001, t = 5.9402, SED = 0.109). Thus, there was a significant reduction (MEAN ± SD) in diurnal voiding frequency in both control and TENS groups [Table/Fig-1,2].
Changes in pre-test-post-test in efficacy measures and responsiveness of OABSS-placebo group.
| Question | Pre-test | Post-test | p-value | t value | SED |
|---|
| (Mean+SD) | (Mean+SD) |
|---|
| 1 | 1.20±0.41 | 0.55±0.60 | 0.0001 | 5.9402 | 0.109 |
| 2 | 1.20±0.41 | 0.75±0.64 | 0.0009 | 3.9428 | 0.114 |
| 3 | 3.15±0.99 | 2.55±1.23 | 0.0067 | 3.0403 | 0.197 |
| 4 | 3.55±0.83 | 2.90±1.21 | 0.0010 | 3.9010 | 0.167 |
Changes in pre-test-post-test in efficacy measures and responsiveness of OABSS -TENS group.
| Question | Pre-test | Post-test | p-value | t-value | SED |
|---|
| (Mean±SD) | (Mean±SD) |
|---|
| 1 | 1.49+0.69 | 0.45±0.51 | 0.0001 | 6.8920 | 0.145 |
| 2 | 1.70±0.98 | 0.50±0.61 | 0.0001 | 5.6404 | 0.213 |
| 3 | 3.60±1.23 | 1.65±1.04 | 0.0001 | 7.3223 | 0.266 |
| 4 | 4.15±1.09 | 2.15±1.18 | 0.0001 | 9.7468 | 0.205 |
In the TENS treatment group, there was a reduction in the nocturnal voiding frequency (OABSS Question 2) from pretest scores (1.70±0.98) to (0.50±0.61) in the post TENS group. This was statistically significant reduction (p-value= 0.0001, t = 5.6404, SED = 0.213). In control group, the reduction in the nocturnal voiding frequency from pretest scores (1.20±0.41) to (0.75±0.64) in the post placebo group. This was not statistically significant reduction (p-value= 0.0009, t = 3.9428, SED = 0.113). Thus, there was a significant reduction (MEAN ± SD) in nocturnal voiding frequency in TENS group but not in the control group [Table/Fig-1,2].
In the TENS treatment group, there was a reduction in the urgency episodes (OABSS question 3) from pretest scores (3.60±1.23) to (1.65±1.04) in the post TENS group. This was statistically significant reduction (p-value= 0.0001, t = 7.3223, SED = 0.266). In control group the reduction in the urgency episodes from pretest scores (3.15±0.99) to (2.55±1.23) in the post placebo group. This was not statistically significant reduction (p-value= 0.0067, t = 3.0403, SED = 0.197). Thus, there was a significant reduction (MEAN ± SD) in urgency episodes in TENS group but not in the control group [Table/Fig-1,2].
In the TENS treatment group, there was a reduction in the urge incontinence episodes (OABSS Question 4) from pretest scores (4.15+1.09) to (2.15+1.18) in the post TENS group. This was statistically significant reduction (p-value= 0.0001, t = 9.7468, SED = 0.205). In control group, the reduction in the urge incontinence episodes from pretest scores (3.55±0.83) to (2.90±1.21) in the post placebo group. This was not a statistically significant reduction (p-value= 0.0010, t = 3.9010, SED = 0.167). Thus, there was a significant reduction (Mean ± SD) in urge incontinence in TENS group but not in the control group [Table/Fig-1,2].
Wilcoxon Sign rank test and Mann-Whitney U test using SPSS package was done for intergroup analysis [Table/Fig-3] for total OABSS score. This revealed a statistically difference in TENS group as compared to control group (Z =-0.509, Asymptomatic Significance = 0.611 and Exact Significance = 0.857).
| Control group |
|---|
| Mann-Whitney U | 2.000 |
| Wilcoxon W | 23.000 |
| Z | -0.509 |
| Asymp. Sig. (2-tailed) | 0.611 |
| Exact Sig. [2*(1-tailed Sig.)] | 0.857b |
a. Grouping Variable: TENS group
b. Not corrected for ties.
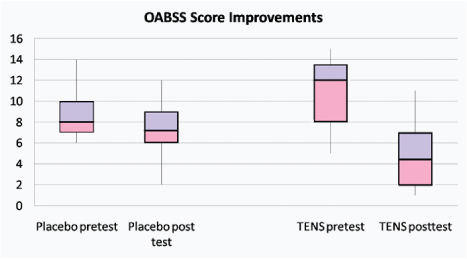
There were no cases of electrode injury in our patients. Box plots were plotted for the total OABSS scores placebo group and TENS group (the overall total score is the sum of all 4 scores). There was a significant improvement in OABSS scores in TENS group and 2 patients were completely dry following TENS therapy [Table/Fig-4].
Improvement in overall total OABSS scores of all questions - placebo group and TENS group.
Discussion
OAB is a disease of spontaneous remissions and exacerbations. Patients often present late after several years of symptoms. Life style modifications and reducing caffeine intake can be practiced as first line treatment. In our study, we found a significant improvement in symptoms after TENS. This is in accord with other studies where TENS has been compared with S3 neuromodulation therapy and antimuscurinic therapy [18,19]. Several other prospective studies have implicated TENS as an effective and safe treatment warranting randomized, placebo controlled trials [20]. The addition of TENS therapy with antimuscurinic therapy has been advocated to ensure complete dryness in children [20]. In elderly patients, where other co-medications have their own anticholinergic side effects and impairment of cognition is a concern, TENS can be a useful intervention [21]. Genetic differences result in dissimilar metabolic degradation of antimuscurinics by cytochrome P-450, so dose adjustment is a challenge. TENS, dose on the contrary is easy to adjust while balancing efficacy against tolerability.
Limitation of our study is that patients who are involved in clinical trial receive more intensive monitoring of their treatment. Motivation increases lifestyle modifications like decreased caffeine intake. This might explain the improvement in OABSS scores in our set of patients who were taken as controls.
Efficacy of TENS depends on the accepted principle that an optimal effect requires an adequate dose [22]. Steps taken to prevent tolerance to TENS therapy include use of alternate high and low frequencies and using burst currents [23].
TENS units are commercially available without prescription as over counter or on rent. Standard TENS device with accessories cost between Rs 1800 and Rs 2,500 with more advanced TENS device between Rs 22,000- Rs 25,800 [24]. Indian Physiotherapists use TENS predominantly for musculoskeletal pain and neuropathic pain and rarely for dysmenorrhea, labour pain and post-operative pain. TENS devises may be loaned to the patients for their duration of stay during hospital. Similar to the model of patient controlled analgesia, patient can be trained on how to self-administer TENS for treating incontinence. Costs to the clinic will be initial outlay for TENS devise and then the running costs of replacing batteries and self adhering electrodes or carbon rubber electrodes. In rural India there may be a socio-cultural barrier to accept TENS due to reluctance to try new treatments. Carbon electrodes will be a better choice in rural India as self-adhering electrodes deteriorate rapidly if not kept in cool and dust free area [24].
Limitation
The limitation of this study is that all patients were uniformly treated with alternate high and low frequency TENS with burst therapy intermittently, to prevent the development of tolerance. High intensity was used to achieve maximum effect. The ideal stimulation protocol needs to be worked out.
Conclusion
Many OAB patients have been successfully treated with TENS. TENS is a portable, non-addictive, non-invasive means of bladder control with flexible patient directed dosing. Small electrical pulses delivered via electrodes directly placed on skin reduce detrusor hyperreflexia through both central and peripheral mechanisms. High stimulus just below strong but comfortable intensity with alternating high and low frequency current produces maximal effect. There is increasing evidence that the therapy is also effective in labour pain, chronic pelvic pain, vulvodynia, fecal incontinence and neurogenic dysfunctional elimination syndrome and post stroke incontinence. Future advancements will likely emphasis on the exact placement site of electrodes with less collateral stimulation.
Competing Interests
We do not have any commercial association that might pose a conflict of interest in connection with the manuscript. We certify that neither this manuscript nor one with substantially similar content under our authorship has been published or is being considered for publication elsewhere.
Appendix 1
OABSS: Patients were instructed to circle the score that best applied to their urinary condition during the past week; the overall score was the sum of the four scores.
| No | Question | Answer | Score |
|---|
| 1. | How many times do youtypically urinate fromwalking in the morning until sleeping at night? | < 7 | 0 |
| 8-14 | 1 |
| >15 | 2 |
| 2. | How many times do youtypically wake up to urinatefrom sleeping at night untilwaking in the morning? | 0 | 0 |
| 1 | 1 |
| 2 | 2 |
| >3 | 3 |
| 3. | How often do you havea sudden desire to urinate,which is difficult to defer? | None | 0 |
| < once / week | 1 |
| > once /week | 2 |
| About once /week | 3 |
| 2-4 times a day | 4 |
| >5 | 5 |
| 4. | How often do youleak urine becauseyou cannot defer it | None | 0 |
| < once / week | 1 |
| > once /week | 2 |
| About once /week | 3 |
| 2-4 times a day | 4 |
| >5 | 5 |
a. Grouping Variable: TENS group
b. Not corrected for ties.
[1]. Coyne KS, Margolis MK, Kopp ZS, Kaplan SA, Racial differences in the prevalence of overactive bladder in the United Status from the epidemiology of LUTS(EpiLUTS) StudyUrology 2012 79(1):95-101. [Google Scholar]
[2]. Reynolds WS, Fowke J, Dmochowski R, The burden of overactive bladder on US public healthCurr Bladder Dysfunct Rep 2016 11(1):8-13. [Google Scholar]
[3]. Gromely EA, Lightner DJ, Burgio KL, Chai TC, Clemens JQ, Culkin DJ, Diagnosis and treatment of overactive bladder (non neurogenic) in adults: AUA/SUFU guidelineJ Urol 2012 188(6 supple):2455-63. [Google Scholar]
[4]. Lucas MG, Bedretdinova D, Bosch JLHR, Burkhad F, Cruz F, Nambiar AK, EAU guidelines on urinary incontinenceEuropean Association of Urology 2014 [Google Scholar]
[5]. Swartz M, Vasavada S, Diagnosing, treating refractory OABRenal and Urology News 2009 [Google Scholar]
[6]. Robinson D, Giarenis I, Cardozo L, The medical management of refractory bladderMaturita 2013 74(4):386-90. [Google Scholar]
[7]. Digesu GA, Sadenghi P, Sharma S, Puccini F, Tubaro A, Fernando R, The importance of cystoscopy and bladder biopsy in women with refractory overactive bladder: the urogynaecologist’s point of viewEur J Obstet Gynaecol Reprod Biol 2013 169(2):408-11. [Google Scholar]
[8]. Benner JS, Nichol MB, Rovner ES, Jumadilova Z, Alvir J, Hussein M, Patient reported reasons for discontinuing overactive bladder medicationBJU Int 2010 105(9):1276-82. [Google Scholar]
[9]. Jundt K, Schreyer K, Friese K, Peschers U, Anticholinergictherapy: do patients take the pills prescribed?Arch Gynecol Obstet 2011 284(3):663-66. [Google Scholar]
[10]. Melzack R, Wall P, The Challenge of Pain 1965 LondonPenguin Books [Google Scholar]
[11]. Bristow SE, Hasan ST, Neal DE, TENS: a treatment option for bladder dysfunctionInt Urogynecol J Pelvic Floor Dysfunct 1996 7(4):185-90. [Google Scholar]
[12]. Liu HT, Jiang Y H, Kuo HC, Increased lipokines implicate chronic inflammation in the pathogenesis of overactive bladder syndrome refractory to antimuscurinic therapyPL oS One 2013 8(10):e76706 [Google Scholar]
[13]. Liu HT, Jiang YH, Kuo HC, Increased serum nerve growth factor levels in patients with overactive bladder syndrome refractory to antimuscrunic therapyNeurourol Urodyn 2011 30(8):1525-29. [Google Scholar]
[14]. Vijaya G, Cartwright R, Derpapas A, Gallo P, Fernando R, Khullar V, Changes in nerve growth factor level and symptom severity following antibiotic treatment for refractory overactive bladderInt Urogynecol J 2013 24(9):1523-28. [Google Scholar]
[15]. Asbjornsen G, Hernaes B, Molvaer G, The effect of transcutaneous nerve stimulation on pressure sores in geriatric patientsJournal of Clinical and Experimental Gerontology 1990 12:209-10. [Google Scholar]
[16]. Kaada B, Promoting healing of chronic ulceration by transcutaneous nerve stimulation (TNS)VASA 1983 12:262-69. [Google Scholar]
[17]. Kaada B, Emru M, Promoting healing of leprous ulcers by transcutaneous nerve stimulationAcupuncture and Electrotherapeutic Research 1988 13:165-76. [Google Scholar]
[18]. Hasan ST, Robson WA, Pridie AK, Neal DE, Transcutaneous electrical nerve stimulation and temporary S3 neuromodulation in idiopathic detrusor instabilityJ Urol 1996 155(6):2005-11. [Google Scholar]
[19]. Sillen U, Arwidsson C, Doroszkiewicz M, Antonsson H, Jansson I, Stalklint M, Effectiveness of Transcutaneous Neuromodulation (TENS) on overactive bladder symptoms in children: A randomized controlled trialJ Pediatr Urol 2014 10(6):1100-05. [Google Scholar]
[20]. Tellenbach M, Schneider M, Mordasini L, Thalmann GN, Kessler TM, Transcutaneous electrical nerve stimulation: An effective neurogenic treatment for refractory nonneurogenic overactive bladder syndrome?World J Urol 2013 31(5):1205-10. [Google Scholar]
[21]. Schwantes U, Grosse J, Wiedemann A, Refractory Overactivebladder: a common problem?Int Urogynecol J 2015 26:1407-14. [Google Scholar]
[22]. Johnson M, Martinson M, Efficacy of electrical nerve stimulation for chronic musculoskeletal pain: a Meta analysis of randomized controlled trialsPain 2007 130:157-65. [Google Scholar]
[23]. Josimari M, De Santana PT, Deirdre M, Walsh PT, Vance C, Barbara A, Effectiveness of transcutaneous Electrical nerve stimulation for treatment of Hyperalgesia and PainCurr Rheumatol Rep 2008 10(6):492-99. [Google Scholar]
[24]. Banerjee G, Johnson MI, Transcutaneous electrical nerve stimulation (TENS): A potential intervention for pain management in IndiaIndian Journal of Pain 2013 27(3):132-41. [Google Scholar]