A Case of Immune Thrombocytopenic Purpura Secondary to Pulmonary Tuberculosis
Sameer Panda1, Lalit Kumar Meher2, Siba Prasad Dalai3, Sachidananda Nayak4, Sujit Kumar Tripathy5
1 Junior Resident, Department of Medicine, MKCG Medical College, Brahmapur, Odisha, india.
2 Professor, Department of Medicine, MKCG Medical College, Brahmapur, Odisha.
3 Junior Resident, Department of Medicine, MKCG Medical College, Brahmapur, Odisha, India.
4 Assistant Professor, Department of Medicine, MKCG Medical College, Brahmapur, Odisha, India.
5 Senior Resident, Department of Medicine, MKCG Medical College, Brahmapur, Odisha, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Sameer Panda, Junior Resident, Room No: 84, PG Hostel- 2, MKCG Medical College, Brahmapur-760004, Odisha, India.
E-mail: drsameer777@gmail.com
The haematological abnormalities associated with active pulmonary tuberculosis were known to human beings since decades but Immune Thrombocytopenic Purpura (ITP) secondary to pulmonary tuberculosis have been reported only in a couple of instances. We report a 27 year-old male patient who was admitted to our hospital with fever, shortness of breath, haematuria, epistaxis and generalized petechiae. The sputum positivity for Acid Fast Bacilli (AFB) and chest X-ray reports were suggestive of active pulmonary tuberculosis in our patient. Clinical and laboratory parameters including bone marrow aspiration cytology diagnosed the case to be ITP. Patient was put on Directly Observed Treatment and Short course (DOTS) category-1 Anti-Tuberculosis Therapy (ATT) and prednisone following which thrombocytopenia was corrected and there was complete recovery of the patient without recurrence of thrombocytopenia.
Anti-tuberculosis therapy, Directly observed treatment and short course, Prednisolone
Case Report
A 27-year-old, non-smoker male was admitted to the in-patient Department of Medicine of MKCG Medical College with complaints of intermittent fever not associated with chills and rigor for 8 days, shortness of breath {Medical Research Council (MRC) dyspnoea grade 2}, multiple purpuric spots over chest and extremities, epistaxis, bleeding per rectum, sub-conjunctival bleed and haematuria. There was no history of any haematological disorder, liver disease, cardiovascular disease or any medication intake in the recent past. Physical examinations revealed a temperature of 102°F, and respiratory rate of 28/minute. Blood pressure was 100/60mm Hg, no lymphadenopathy or hepatospleenomegaly. Chest wall examination revealed crepitation over right infra-clavicular area. Per-rectal examination revealed no pathology. The electrocardiography was with-in normal limit. The initial complete blood count and routine biochemical parameters were normal [Table/Fig-1,2].
| Parameter Tested | Test Values | Reference Range |
|---|
| Haemoglobin (Hb) | 11.5g/dl | 11.0-15.5g/dl |
| Red Blood Count | 5.64 lacs/ μL | 3.5-5.5 lacs/ μL |
| Mean Corpuscular Volume (MCV) | 61fL | 60-90fL |
| Mean Corpuscular Haemoglobin (MCH) | 20.4pg | 27-32pg |
| Mean Corpuscular Haemoglobin Concentration (MCHC) | 33.4g/dl | 30-35g/dl |
| Red cell distribution width coefficient of variation(RDW-CV) | 18.4% | 11.6%-14.6% |
| Total Leukocyte Count (TLC) | 9,360/μL | 4000-11,000/ μL |
| Total Platelet Count (TPC) | 5000 | 1.6-4.0 lacs/ μL |
| Erythrocyte Sedimentation Rate (ESR) | 126 mm in 1st hour | 0-22 (M)0-29 (F) |
| Differential count |
| Neutrophil | 70% | 40-75% |
| Lymphocyte | 25% | 20-45% |
| Eosinophil | 0.1% | 01-06% |
| Monocyte | 3.3% | 02-10% |
| Basophil | 0.1% | 00-01% |
Comment on Peripheral Smear (CPS): Microcytic Hypochromic Anaemia, Moderate Anisopoikilocytosis with Remarkable Paucity of Platelets.
| Parameter Tested | Test Values | Reference Range |
|---|
| Bleeding Time | 4 minutes 46 seconds | 3-9 minutes |
| Clotting Time | 3 minutes 26 seconds | 2-6 minutes |
| Activated Partial Thromboplastin Time (Aptt) | 27 seconds | 28-38 seconds |
| Pt-Inr | 1.09 | 0.8-1.2 |
| Sr Urea | 42mg/dl | 10-50mg/dl |
| Sr Creatinine | 1.0mg/dl | 0.6-1.4mg/dl |
| Total Cholesterol | 130mg/dl | Below 200mg/dl |
| Trigleceride | 206mg/dl | Below 150mg/dl |
| Low Density Lipoprotein | 88mg/dL | Below 70mg/dL |
| High Density Lipoprotein | 42mg/dL | 40-60mg/dl |
| Sr Bilirubin (Total) | 0.8mg/dl | Upto 1mg/dl |
| Sr Bilirubin (Direct) | 0.1mg/dl | Upto 0.2mg/dl |
| Sr Sgot | 57IU/L | Upto 40IU/L |
| Sr Sgpt | 34IU/L | Upto 40IU/L |
| Sr Alkaline Phosphate | 230IU/L | 110-310IU/L |
| Sr Protein | 5.8mg/dl | 6.6-8.0mg/dl |
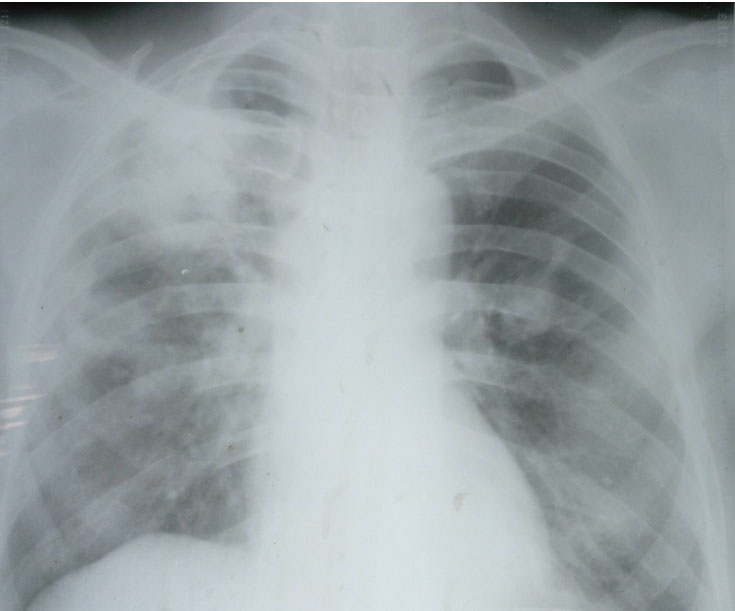
Direct Coombs test was negative and Fibrin Degradation Product (FDP) was normal. Serum ferritin was 226ng/ml. (normal value 18-270ng/ml). Quantitative Buffy Coat and Immuno-cromatography Test for malarial antigens were negative. Antibodies to Salmonella antigen, Anti-neutrophlic antibody and rheumatoid factor were absent. HIV, Hepatitis B surface Antigen, Anti-Hepatitis C Virus antibody tests were negative. Blood culture was negative. Bone marrow biopsy showed hyper-cellular marrow and normal maturation of myeloid and erythroid precursors. Megakaryocytes were increased in number and had normal morphology. No granulomas, leukemic infiltrate or metastatic deposits were detected. Sputum was positive for Acid Fast Bacilli [AFB] on more than two occasions. A chest x-ray demonstrated patchy opacity over right upper zone [Table/Fig-3]. Based upon above finding, a provisional diagnosis of pulmonary tuberculosis with thrombocytopenia was made. Patient was then put on Directly Observed Treatment and Short (DOTS) course category-1 Anti-Tuberculosis Therapy (ATT) (i.e., isoniazid 5mg/kg/d, rifampicin10mg/kg/d, ethambutol 25mg/kg/d, pyrazinamide 30mg/kg/d) and subsequently received 8 units of random donor platelets. However, over a period of next 7 days the platelet counts did not increased satisfactorily and the petechiae and purpura were remained as before. In view of low platelet count oral prednisone (1mg/kg/day) was started along with ATT. By judging the clinical severity and patient’s affordability for human immunoglobulin in a resource limited setting like our institution, we had preferred prednisolone as a primary therapy.
Chest X-ray demonstrating patchy opacity over right upper zone.
Platelets count started to increase after two weeks of the ATT and prednisone. There was no fresh bleeding from any sites, petechiae and purpura started to decrease. Prednisone was then tapered off over a period of one month. Patient was followed-up every month for first 6 months and there was no recurrence of thrombocytopenia. Sputum AFB was negative at 2nd and 6th months of follow-up. Platelet counts were 1.54lacs/Cumm, 2.24lacs/Cumm at first and second month of treatment. At the end of six month and one year of follow-up platelet count was 2.67lacs/Cumm and 3.06lacs/Cumm respectively.
Discussion
Tuberculosis can present with various haematological manifestations like anemia, leukocytosis and pancytopenia. Pancytopenia in tuberculosis occurs by means of granulomatous infiltration of bone marrow where-as, Immune Thrombocytopenic Purpura (ITP) in association with pulmonary tuberculosis is a very rare event. ITP is an acquired disorder in which there is immune mediated destruction of platelets. In adults, ITP have a more chronic course but sometime ITP can present with a very abrupt onset [1,2]. ITP can be diagnosed by presence of thrombocytopenia with a normal peripheral smear and exclusion of other secondary causes capable of producing thrombocytopenia [3]. Common secondary causes of ITP include autoimmune diseases like SLE, infections (HIV/hepatitis C), drugs (rifampicin) and lympho-proliferative disorders but tuberculosis per se a very rare condition [4]. The association of severe thrombocytopenia due to ITP with tuberculosis is very rare event and had been reported only in a couple of instances [5,6]. The present reported case has normal blood count and normal peripheral smear except thrombocytopenia. Clinical and laboratory examinations also showed no other disorder leading to thrombocytopenia such as Disseminated Intravascular Coagulation (DIC), Thrombotic Thrombocytopenic Purpura (TTP), Evan’s syndrome or Haemophagocytic Syndrome. Sputum AFB was positive and there was infiltrating shadow on right upper zone in chest x-ray. So, diagnosis of pulmonary tuberculosis with thrombocytopenia was made. As, there was no evidence of bone marrow infiltration with tuberculosis, the cause accounting for thrombocytopenia in the reporting patient who responded to anti- tubercular medication is immune mediated platelet destruction associated with tuberculosis [7]. Presence of either platelet antigen specific antibodies or platelet surface membrane Immunoglobulin G (IgG) supports the immune mediated cytopenias in tuberculosis [8,9]. The anti-platelet antibodies present in some cases of ITP secondary to tuberculosis has been postulated to be secreted by the lymphocytes [10].
The previously reported cases were started with various drugs like Intravenous Immunoglobulin, Thrombopoietin (TPO) Receptor agonist (eltrombopag), high dose dexamethasone to improve platelet count [11,12]. In the present case patient received very short course of prednisone under coverage of ATT, which was withdrawn over a period of one month. Steroid was restricted to a period of one month in view of improved clinical conditions probably due to ATT. Our patient showed improvement in platelet counts only with ATT on subsequent visits. There were no signs or symptoms of hepatic dysfunction. So, we conclude that present case of thrombocytopenia in pulmonary tuberculosis was immune mediated, which responded to ATT completely.
Conclusion
In conclusion, secondary ITP can occur as one of the manifestation of pulmonary tuberculosis and ATT can cure the condition.
Comment on Peripheral Smear (CPS): Microcytic Hypochromic Anaemia, Moderate Anisopoikilocytosis with Remarkable Paucity of Platelets.
[1]. Mert A, Bilir M, Tabak F, Miliary tuberculosis: Clinical manifestation, diagnosis and outcome in 38 adultsRespirology 2001 6:217-24. [Google Scholar]
[2]. Glasser RM, Walker RI, Herion JC, The significance of hematologicabnormalities in patients with tuberculosisArch Intern Med 1970 125:691-95. [Google Scholar]
[3]. Ghobrial MW, Albornoz MA, Immune thrombocytopenia: A rare presenting manifestation of tuberculosisAm J Hematol 2001 67:139-43. [Google Scholar]
[4]. George JN, Raskob GE, Idiopathic thrombocytopenic purpura. Diagnosis and managementAm J Med Sci 1998 316:87-93. [Google Scholar]
[5]. Madkaikar M, Ghosh K, Jijina F, Tuberculosis and immune thrombocytopeniaHaematologica 2002 87:ELT38 [Google Scholar]
[6]. Ozkalemkas F, Ali R, Ozkan A, Tuberculosis presenting as immune thrombocytopenic purpuraAnn Clin Microbiol Antimicrob 2004 3:16 [Google Scholar]
[7]. Kalra A, Palaniswamy C, Immune thrombocytopenia in a challenging case of disseminated tuberculosisCase Report Med 2010 2010:pii946278 [Google Scholar]
[8]. Boots RJ, Roberts AW, McEvoy D, Immune thrombocytopenia complicating pulmonary tuberculosis. Case report and Investigationof mechanismThorax 1992 47:396-97. [Google Scholar]
[9]. Jurak SS, Aster R, Sawaf H, Immune thrombocytopenia associated with tuberculosisClin Pediatr 1983 22:318-19. [Google Scholar]
[10]. Tsuro K, Kojima H, Mitoro A, Immune thrombocytopenic purpura associated with pulmonary tuberculosisIntern Med 2006 45:739-42. [Google Scholar]
[11]. Srividya G, Nikhila GP, Kaushik AV, Jayachandran K, Immune thrombocytopenia in tuberculosis: Causal or coincidental?Journal of Global Infectious Diseases 2014 6(3):128 [Google Scholar]
[12]. Neunert C, Lim W, Crowther M, Cohen A, Solberg L, Crowther MA, The American Society of Hematology 2011 evidence-based practice guideline for immune thrombocytopeniaBlood 2011 117(16):4190-207. [Google Scholar]