Incidence of Second Primary Malignancy (SPM) after successful treatment of primary is increasing. Occurrences of SPMs is more common in head and neck cancers than any other sites with incidence ranging between 5-30% within 10 years of diagnosis of primary malignancy and more common in smokers and alcohol consumers [1–3]. According to the criteria for classifications of second primary cancer proposed by Warren in 1934, there should be at least 2 cm of normal mucosa between the two tumours and if the tumours are in the same location, then they should be separated by time by at least five years [4].
The cases of SPMs may cause the problem for optimal treatment due to location of tumour in anatomical regions of previously irradiated areas. Treatment strategies depend on volume, dose, and tolerance of normal tissue which are in close proximity to previously irradiated tissues. This study was conducted retrospectively to analyse incidence, disease free survival between malignancies, pattern of treatment and outcome.
Materials and Methods
Sixteen patients of SPM of head and neck region managed over a period of two years from January 2012 to December 2015 in Department of Radiotherapy –II, Pt. BD Sharma PGIMS, Rohtak were analysed retrospectively to find out the incidence of SPM, disease free survival between two malignancies, after second malignancy, age, smoking status, pattern of treatment and outcome. All cases of second primary tumour were confirmed by biopsy. Histopathologically both index and second primary tumours were squamous cell carcinoma. SPMs were classified with time interval of 5 years and normal mucosa of 2 cm for tumour those developed at same subsite and for different subsite.
Results
Twenty two treated cases of head and neck cancer develop second primary tumour of head and neck during this period. Out of those three underwent surgery, one had metastases and two had poor general condition so they were given palliative and supportive treatment. Sixteen patients with unresectable disease treated with reirradiation were analysed in this study. All the patients were planned for and given external beam radiotherapy to receive a total dose of 40 Gy in 20 fractions over 4 weeks (2Gy/fraction, 5 days/week) on teletherapy cobalt 60 machine with spinal cord sparing bilateral parallel opposed field to face and neck.
Median age of presentation of first malignancy was 27 years (ranged 26 -65 years), whereas median age was 60 years for second malignancy (range 45-71 years). Fifteen patients 94% (15/16) were male and one was female 6% [Table/Fig-1]. All patients were smokers during first malignancy; 87.5% (14/16) had history of smoking during second malignancy. Only 56% quit smoking after treatment of first malignancy, remaining 44% never quit smoking. Almost all patients those quit restarted smoking within 8-14 months after completion of treatment. Alcohol consumers were 63% (10/16) during treatment throughout the malignancies.
Patients characteristics.
| Sr No. | Year of 1st Malignancy | Male / Female | Site of Index Tumour | Age | Second tumour | Site |
|---|
| 1 | 1994 | Male | Rt Tonsil, III | 26 | 2013 | Left Pyriform Fossa |
| 2. | 2001 | Male | Tonsil | 59 | 2013 | Base Of Tongue |
| 3. | 2001 | Male | Right lower alveolus | 38 | 2013 | Larynx |
| 4 | 2002, | Female | Base of Tongue | 42 | 2012 | R.Alveolus |
| 5. | 2002 | Male | Base of Tongue | 51 | 2012 | R Vallecula |
| 6. | 2005 | Male | Left Tonsil | 56 | 2014 | Left tonsil, soft palate, vallecula |
| 7. | 2005 | Male | Left Tonsil | 47 | 2015 | Soft palate |
| 8. | 2007 | Male | Tonsil III | 45 | 2015 | Floor of mouth |
| 9. | 2008 | Male | Base of Tongue | 60 | 2013 | Base of tongue vallecula |
| 10. | 2008 | Male | Supraglottis Larynx | 57 | 2014 | Hard Palate |
| 11. | 2009 | Male | Suprglottis Larynx | 49 | 2013 | Ant tongue |
| 12. | 2010 | Male | Larynx | 61 | 2012 | Floor of Mouth |
| 13. | 2011 | Male | Larynx | 53 | 2013 | Hard Palate |
| 14. | 2012 | Male | Rt Pyriform fossa | 61 | 2014 | Retromolar trigone |
| 15. | 2012 | Male | Floor of mouth | 49 | 2014 | Larynx, Epiglottis |
| 16. | 2010 | Male | Vocal cord Right | 65 | 2014 | Buccal mucosa, |
Site of primary malignancy
Oropharynx (50%) was most common site of presentation primary tumour whereas oral cavity was most common site of presentation in second primary tumour [Table/Fig-2].
Site of primary malignancy.
| Primary tumour | No | % | Secondary tumour | No | % |
|---|
| Oral cavityAlveolusFloor of MouthHard PalateRetromolar trigoneBuccal Mucosa | 0101--- | 6.256.25--- | Oral cavity-Alveolus-Floor of Mouth-Hard Palate-Retromolar trigone-Buccal Mucosa-Ant Tongue | 08010202010101 | 506.2512.512.56.256.256.25 |
| OropharynxTonsilBase of TongueValleculaSoft Palate | 0503-- | 31.2518.75-- | Oropharynx-Tonsil- Tongue-Vallecula-Soft Palate | 0501020101 | 31.256.2512.56.256.25 |
| HypopharynxPyriform fossa | 01 | 6.25 | HypopharynxPyriform fossa | 01 | 6.25 |
| Larynx | 05 | 31.25 | Larynx | 02 | 12.5 |
Treatment received for primary malignancy
Almost all patient received radiation therapy during their course of treatment for primary tumour. Combined modality treatment was given in 11 patients including chemotherapy and radiotherapy. Neoadjuvant chemotherapy followed by concomitant chemoradiation was received by 8 patients. Paclitaxel, carboplatin and 5FU was most common chemotherapeutic agents used as NACT whereas cisplatin (9/16) followed by gemcitabine (2/16) used as weekly concurrent with radiation [Table/Fig-3].
Treatment received for primary malignancy.
| Treatment modality | No of Patients | Dose |
|---|
| Radiation alone | 5/16 | 54 Gy – 60 Gy |
| Combined modality treatment | 11 /16 | 66 Gy – 70 Gy |
| NACT Given | 08/16 | |
| Concomitant | 11/16 | |
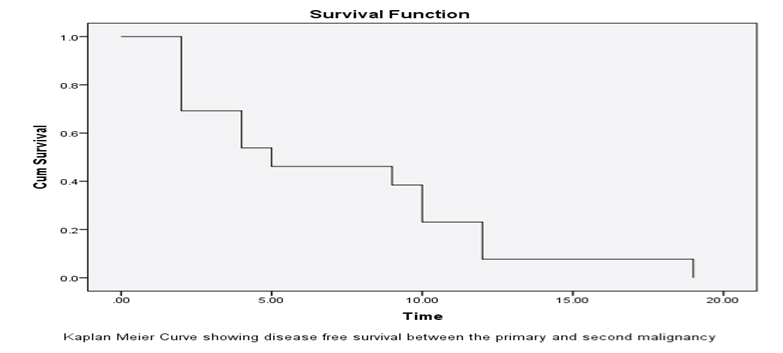
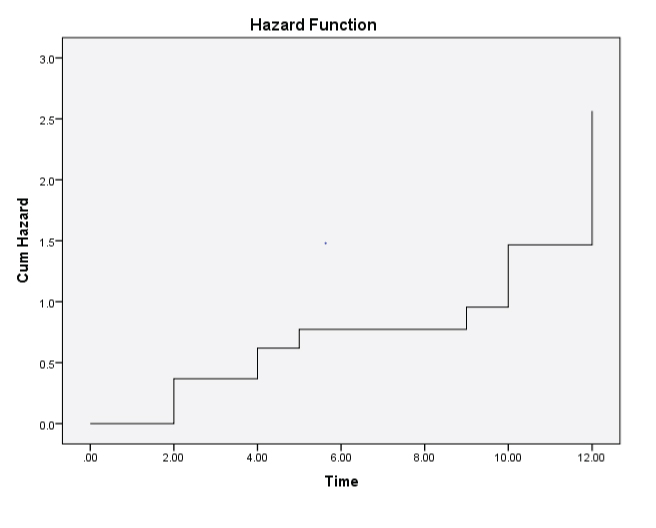
Disease free survival median months 84 (ranged 24 -228 months) between first and second malignancy. The minimal time interval was 2 years between two malignancies [Table/Fig-4]. Majority of patients lost to follow-up after treatment completion of first malignancy. All patients developed SPMs at previous irradiated area. All 16 patients were treated with radiation alone with dose of 40 Gy in 20 fractions over 4 weeks five days a week to face and neck by bilateral parallel opposed spinal cord sparing field. Fifteen patients completed prescribed radiation, one left treatment after three weeks due to grade 3 mucositis. Five patients died they had stable disease. Three patients are disease free after 12-14 months of follow-up. Six showed partial response at six months of follow-up. One patient developed metastases to lung and liver 6 months after completion of treatment. All patients developed grade 2 and 3 mucositis during treatment and follow-up [Table/Fig-5].
Kaplan meier curve showing disease free survival between the primary and second malignancy.
Kaplan meier curve showing hazard function.
Discussion
The reported probability of occurrence of second primary tumours within five years of radiation alone is approximately 15% of patients [5]. Among them, one quarter are in head and neck region and in 30% of patients within 10 years of onset [1–3]. Overall Head and Neck Squamous Cell Carcinoma (HNSCC) patients have 36% cumulative life time risk of developing SPM over 20 years [6]. Total number of cancer patients registered in Department of Radiotherapy-II were 5948 between 2012- 2015 among them 1896 (32%) were of head and neck cancer. Twenty two (1.16 %) cases of treated head and neck cancer developed SPMs of head and neck during this period.
Several aetiological factors have been documented for development of SPMs these include genetic predisposition, field cancerization, use of chemotherapeutic agents, oncogenic viruses such as human papilloma virus, etc.
Other factors such as age, smoking and alcohol consumption also play an important role in development of SPMs. Medical literature revealed higher risk in range between 5 and 30% in smokers and alcohol drinkers than non-smokers and non-alcohol drinkers [7,8].
In present study, 44% patients continued smoking after treatment of index tumour; overall 87.5% were smokers at the time of diagnosis of second malignancy. Alcohol consumers were 63% (10/16) during treatment and throughout the malignancies. Moreover, in present analysis all SPMs devolved in previously irradiated area and chemotherapy received patients.
The anatomic distribution associated with risk factors. The risk factor for oral cavity and hypopharynx SPMs related to carcinogen exposure, such as tobacco use, smoking, alcohol drinking and betel nut chewing [9].
The literature also depicts younger patients at primary tumour having the highest risk of SPMs due the longer survival with advance treatment strategies [10,11]. Similar age trends were seen in present study.
Site of index tumour also affects occurrence and prognosis of SPMs such as index tumour of the oral cavity and oropharynx associated with tumours of same location [10,12].
This analysis also showed preponderance of oral cavity tumours (50%) among them the most common site was floor of mouth and hard palate (25%), oropharynx 31% and hypopharynx 6.25 %. Majority of patient lost to follow-up after treatment completion of first malignancy in our study. The diagnosis of SPM was made only when the patients presented with symptoms. The delay in presentation might be due to the fact that late radiation toxicities symptoms such as mucositis, fibrosis, oedema, etc which were present for a longer duration.
Previous irradiation attributed to limited treatment options. Many strategies have been tried to improve local control, quality of life and survival. These include surgery, chemotherapy, and Reirradiation.
Reirradiation is a treatment option in unresectable SPMs. Reirradiation can be performed with external beam radiotherapy, radiosurgery, intensity modulated radiotherapy or brachytherapy. However, rerradiation is associated with treatment induced complications. Moreover various factors should also be considered before administering reirradiation such as co-morbidities, performance status, speech and swallowing function and sequelae of previous treatment such as fibrosis, carotid stenosis, osteoradionecrosis etc., as per recommendation of the American College of Radiology (ACR) expert panel HNC appropriate criteria for RERT [13].
In reirradiation, dose of 55 Gy to 60 Gy is recommended for curative treatment to achieve local control [14,15]. However, conventional reirradiation with 60 Gy to previously irradiated tissue associated with sever late complication such as bleeding, necrosis and death were reported in earlier studies [16,17]. Conformal therapy now recommended strategies for reirradiation for SPMs. In present study, all patients were given dose of 40 Gy and treated on cobalt 60 machines with spinal cord sparing field to face and neck.
Fifteen patients completed prescribed radiation, one left treatment after three weeks due to grade 3 mucositis. Patient followed-up for 9 month range 12-16 months. Three patients were disease free after 12-14 months of follow-up (20%). Six showed partial response at six months of follow-up. One patient developed metastases to lung and liver 6 months after completion of treatment. Five patients died they had stable disease. All patients developed grade 2 and 3 mucositis during treatment and follow-up.
Though literature review depicted favorable outcome of reirradiation, external beam radiation alone associated with severe late toxicity [17–20]. Stevens et al., observed local control rate was 60% in case of a second primary and 27% in case of a recurrent tumours, originating in different head and neck sites reirradiated by conventional irradiation alone and 14 patients with brachytherapy. The 5 years overall survival varied from 17% among patients with recurrent tumours to 37% among those with SPTs [17]. Wang et al., found 5 year survival of 93% for early stage second primary laryngeal tumours [18] whereas, other series reported a median survival of 10 months and a 3-year overall survival of 22% with primary reirradiation alone [19,20].
Conclusion
Longer survival with advances in treatment strategies associated with increased incidence of SPMs. SPMs have a poor prognosis with dismal survival. Lack of awareness, loss to follow-up, continuation of smoking and alcohol consumption may contribute to SPMs. A thorough follow-up after treatment of head and neck cancer is necessary for detection and early treatment of SPMs.