Spontaneous Subdural Haematoma Developing Secondary to Arachnoid Cyst Rupture
Mehmet Onur Yüksel1, Mehmet Sabri Gürbüz2, Mehmet Senol3, Numan Karaarslan4
1 Specialist Neurosurgeon, Department of Neurosurgery, Erzurum Bolge Training and Research Hospital, Erzurum, Turkey.
2 Specialist Neurosurgeon, Department of Neurosurgery, Safa Hospital, Istanbul, Turkey.
3 Specialist Neurosurgeon, Department of Neurosurgery, Erzurum Bolge Training and Research Hospital, Erzurum, Turkey.
4 Assistant Professor, Department of Neurosurgery, Namık Kemal University Faculty of Medicine, Tekirdag, Turkey.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Mehmet Sabri Gürbüz, Yıldıztepe mah. Bağcılar cad. No: 108 34203 Bağcılar, Istanbul, Turkey.
E-mail: mehmetsabrigurbuz@gmail.com
Arachnoid cysts are congenital, benign, non-neoplastic, extra-axial intra-arachnoidal lesions. Arachnoid cysts rarely become symptomatic, with bleeding. Intracranial haemorrhage as a complication of arachnoid cyst is a very rare condition. It is well-known that mid-cranial fossa cysts might cause intracerebral haemorrhage or subdural haematoma secondary to traumas. However, the occurrence of spontaneous subdural haematoma secondary to arachnoid cysts, developing without any trauma, is even rarer. A 17-year-old boy presenting with diplopia and headache, with no history of trauma, was diagnosed with left temporal lobe arachnoid cyst and left fronto-parietal subdural haematoma. He was operated on, solely for his haematoma, with no intervention performed for the arachnoid cyst. Authors suggest that it is sufficient to perform an operation for the haematoma only -without arachnoid cyst resection- if there is no clinical presentation specific to the arachnoid cyst itself.
Arachnoid cyst complication, Spontaneous rupture, Without trauma
Case Report
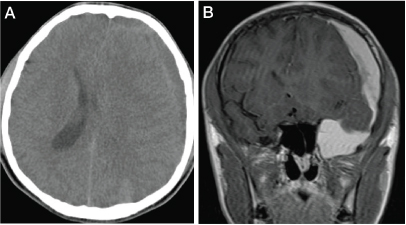
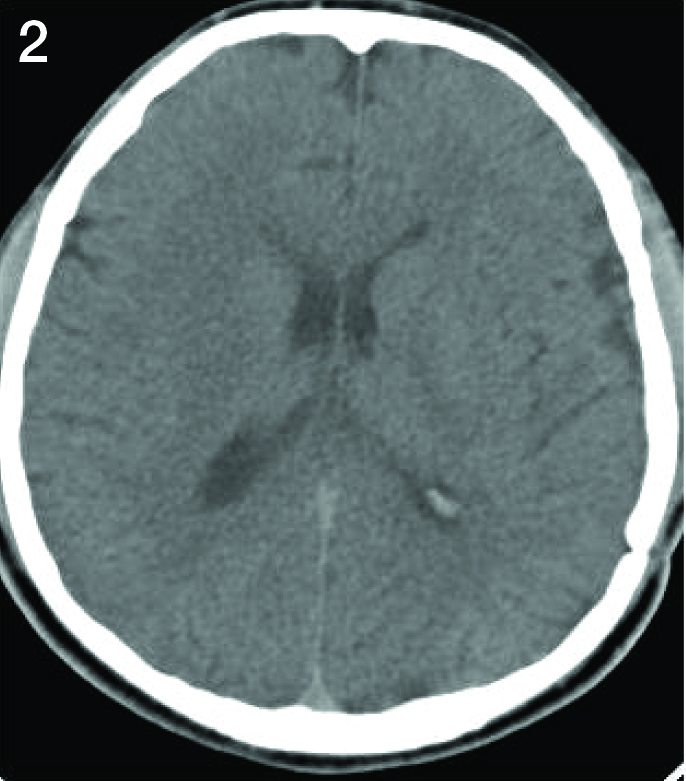
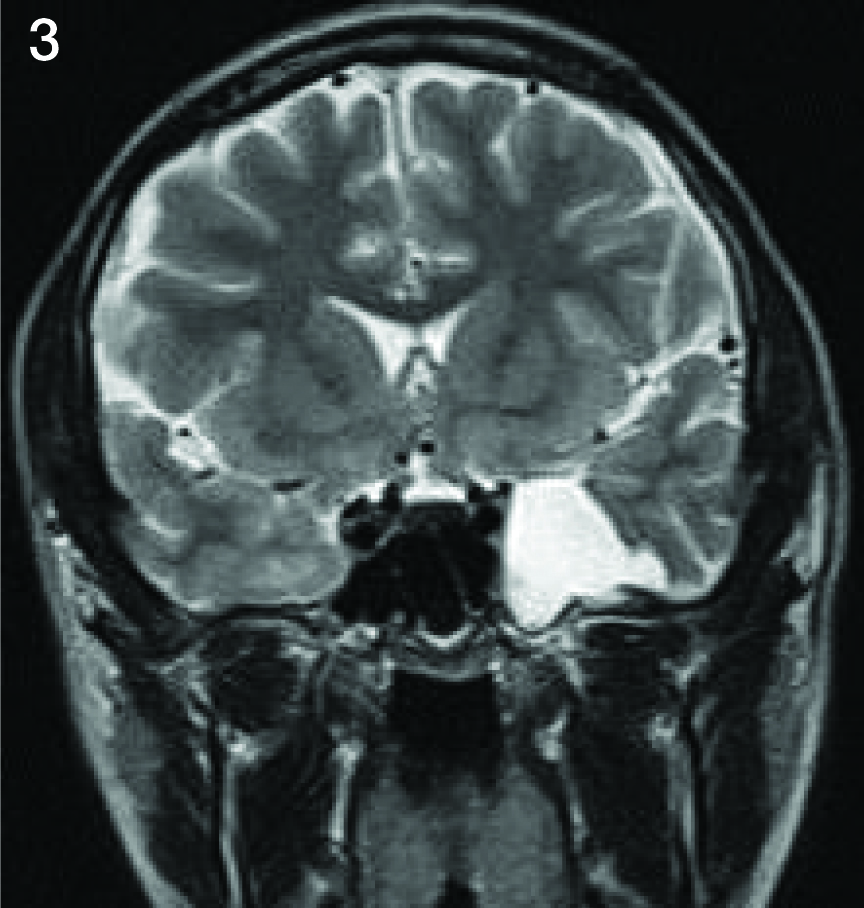
A 17-year-old boy had been admitted to the outpatient clinic of eye diseases, with the complaints of intensifying headache and double vision for the previous 10 days. Papilloedema had been detected in his fundoscopic examination and the patient had been referred to the Department of Neurosurgery, after eliminating possible ophthalmological pathologies. His physical examination was unremarkable. The neurological examination revealed only painless restriction of his eye movement in left lateral gaze. He had no history of trauma. Cranial CT (Computed Tomography) and MRI (Magnetic Resonance Imaging) revealed a left temporal arachnoid cyst and a left frontoparietal subdural haematoma 2.5 cm in thickness causing an 11mm midline shift [Table/Fig-1a&b]. Subdural haematoma was evacuated via a left fronto-parietal craniotomy. No intervention was performed for the arachnoid cyst since the haematoma was not intracystic. Post-operative CT scan revealed that the subdural haematoma had been evacuated successfully [Table/Fig-2]. No perioperative or post-operative complication was encountered. The patient was discharged from hospital on the 5th day of operation, with no neurological deficit. One-year follow-up MRI of the patient revealed no recurrence of haematoma and no significant change in pre-existing arachnoid cyst [Table/Fig-3].
1a: Axial cranial CT image taken on admission, showing a left fronto-parietal subdural haematoma compressing the left cerebral hemisphere and resulting in an 11 mm midline shift.
1b: T-1 weighted coronal cranial MR image showing a left fronto-parietal subdural haematoma and its communication with left temporal arachnoid cyst.
Post-operative axial cranial CT image showing the successful evacuation of left fronto-parietal subdural haematoma via a left fronto-parietal craniotomy and disappearance of the midline shift.
T-2 weighted coronal cranial MRI at 1-year follow-up showing no recurrence of haematoma and no significant change in pre-existing arachnoid cyst.
Discussion
Arachnoid cysts are extra-axial cystic cavities filled with Cerebro-Spinal Fluid (CSF) or with a fluid resembling CSF. Arachnoid cysts might be primary or congenital and may develop secondary to pathologies such as extra-axial haematoma, trauma, tumour or infection [1,2]. Arachnoid cysts, which are benign, congenital, non-neoplastic extra-axial masses, account for only 1% of the lesions that occupy intracranial space [1]. Although they might develop in all age groups, 75% of them develop until childhood age and majority of them are discovered incidentally [2,3].
Although the findings vary according to the localization of the cysts, majority of them progress in an asymptomatic manner throughout life [3,4]. Slyvian fissure-localized cysts generally appear with the findings of raised intracranial pressure. Although the most frequent symptom is convulsion in supra-tentorial arachnoid cysts, cerebellar findings are in the front line in posterior fossa cysts [5,6].
The natural course of arachnoid cysts is not fully understood. Most of them progress silently, while some others might be complicated with the development of subdural effusion, subdural haematoma, and intracerebral or intracystic haemorrhage [4,5]. Intracranial haemorrhages associated with arachnoid cysts usually occur secondary to minor head traumas and spontaneous bleedings are observed extremely rarely [6,7]. It is postulated that head trauma causes CSF entering the cystic cavity, increasing the intracystic pressure which eventually leads to the rupture of the vessels located in the CSF-filled cystic cavity [7,8]. It has also been reported that the rupture of weak leptomeningeal veins located in the cyst wall may lead to subdural haematoma. Membranous adhesions and decreased compliance are considered the most important predisposing factors [8].
Haematomas secondary to the rupture of arachnoid cysts spontaneously or due to traumas should be treated in an individual-based manner that is specific to each case, either conservatively or surgically [9,10]. Clinical assessment is the most important guide in deciding whether to wait for the spontaneous resolution of haematoma or to evacuate it surgically. Intracranial haemorrhages seen as complications of arachnoid cysts generally require surgical intervention. [8,10]. On the other hand, spontaneous resolution of haematoma has also been reported in the literature [9,11,12]. In our case, surgical intervention was required, because the patient had an approximately 11mm midline shift and findings of increased intracranial pressure.
In our case report, no intervention was required for the arachnoid cyst. Surgical interventions like cysto-peritoneal shunt, ventriculo-peritoneal shunt or fenestration between cyst, cisternae and ventricles (with endoscopy or craniotomy) have also been reported in the literature [6,10]. These interventions might be required when the arachnoid cyst becomes symptomatic or causes hydrocephalus and in case of any seizure confirmed with electroencephalogram [11,12]. However, if these symptoms do not exist, we believe that there is no need for any intervention to the cyst. By doing so, additional perioperative and post-operative complications resulting from cyst resection or shunting procedure will be avoided [1,6]. In the series including 16 cases, Parsch et al., [8] did not consider it necessary to perform any intervention for previously asymptomatic arachnoid cysts. Consequently, as long as the arachnoid cyst itself is not symptomatic and when there is no intracystic haemorrhage, there is no need for cyst resection since there is no data in the literature claiming increased risk of re-bleeding of an arachnoid cyst which has previously bled once [3,8].
Conclusion
Spontaneous subdural haematomas that develop as complications of arachnoid cysts are extremely rare. In these cases, it is sufficient to perform operation solely for the haematoma without arachnoid cyst resection if there is no clinical presentation proved to be associated with arachnoid cyst itself.
[1]. Robinson RG, Congenital cysts of the brain: Arachnoid malformationsNeurol Surg 1971 4:133-73. [Google Scholar]
[2]. Galassi E, Piazza G, Gaist G, Frank F, Arachnoid cysts of the middle cranial fossa: a clinical and radiological study of 25 cases treated surgicallySurg Neurol 1980 14:211-19. [Google Scholar]
[3]. Wester K, Pecularities of intracranial arachnoid cysts: Location, sidedness and sex distribution in 126 consecutive patientsNeurosurgery 1999 45(4):775-79. [Google Scholar]
[4]. Mori K, Yamamoto T, Horinaka N, Maeda M, Arachnoid cyst is a risk factor for chronic subdural haematoma in juveniles: twelve cases of chronic subdural haematoma associated with arachnoid cystJ Neurotrauma 2002 19:1017-27. [Google Scholar]
[5]. Iaconetta G, Esposito M, Maiuri F, Cappabianca P, Arachnoid cyst with intracystic haemorrhage and subdural haematoma: case report and literature reviewNeurol Sci 2006 26:451-55. [Google Scholar]
[6]. Daneyemez M, Gezen F, Akboru M, Sirin S, Ocal E, Presentation and management of supratentorial and infratentorial arachnoid cysts. Review of 25 casesJ Neurosurg Sci 1999 43(2):115-20. [Google Scholar]
[7]. Gündüz B, Ofluoğlu EA, Ekinci B, Toplamaoğlu H, An arachnoid cyst complicated by spontaneous intracystic haemorrhage: a case reportSinir Sistemi Cerrahisi Derg 2008 1(2):112-15. [Google Scholar]
[8]. Parsch CS, Krauss J, Hoffmann E, Meixensberger J, Roosen K, Arachnoid cysts assosiated with subdural haematomas and hygromas: analysis of 16 cases, longterm fallow-up, and review of the literatureNeurosurgery 1997 40:483-90. [Google Scholar]
[9]. Yilmaz C, Cetinalp E, Caner H, Altinors N, Disappearance of arachnoid cyst after rupturing into subdural spaceActa Neurochir (Wien) 2007 149:731-33. [Google Scholar]
[10]. Cincu R, Agrawal A, Eiras J, Intracranial arachnoid cysts: Current concepts and treatment alternativesClin Neurol Neurosurg 2007 109:837-43. [Google Scholar]
[11]. Rakier A, Feinsod M, Gradual resolution of an arachnoid cyst after spontaneous rupture into the subdural space. Case reportJ Neurosurg 1995 83:1085-86. [Google Scholar]
[12]. Bilginer B, Onal MB, Oguz KK, Akalan N, Arachnoid cyst associated with subdural haematoma: report of three cases and review of the literatureChilds Nerv Syst 2009 25:119-24. [Google Scholar]