Post Colonoscopy Ischaemic Colitis in a Patient without Risk Factors for Colon Ischemia: A Case Report
Dattatray Balasaheb Solanke1, Nirav Madhukant Pipaliya2, Alisha Nitin Chaubal3, Meghraj Ananda Ingle4, Prabha Dilip Sawant5
1 Senior Resident, Department of Gastroenterology, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai, Maharashtra, India.
2 Senior Resident, Department of Gastroenterology, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai, Maharashtra, India.
3 Senior Resident, Department of Gastroenterology, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai, Maharashtra, India.
4 Associate Professor, Department of Gastroenterology, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai, Maharashtra, India.
5 Professor and Head, Department of Gastroenterology, Department of Gastroenterology, Lokmanya Tilak Municipal Medical College and General Hospital, Sion, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Dattatray Balasaheb Solanke, Room No.507, New RMO Hostel, Lokmanya Tilak Municipal Medical College, Sion-400022, Mumbai, Maharashtra, India.
E-mail: dattatraybs@yahoo.co.in
Ischaemic colitis is the most common form of intestinal ischaemia and is more common in the elderly and in the people having risk factors for colonic ischaemia. Colonoscopy procedure itself is a rare cause of ischaemic colitis. Fewer than 20 cases of ischaemic colitis caused by colonoscopy procedure have been reported in the english literature till date.
This patient presented to us within hours of routine colonoscopy with rectal bleeding and lower abdominal pain. On repeat colonoscopy, the patient had mucosal oedema and ulcerations in the descending colon and sigmoid colon. Computed tomography of abdomen and biopsy of the involved segment confirmed ischaemic colitis. The patient recovered with conservative management.
Colonic blood flow, Colonic ulcerations, Haematochezia
Case Report
A 43-year-old farmer underwent colonoscopy as a part of the work-up for constipation in the Department of Gastroenterology. He did not have any alarming symptoms like bleeding per rectum, anorexia or weight loss and had no history of any coagulopathy, embolic risk-factors and vasculitis. He was of average built with a Body Mass Index (BMI) of 23.8 Kg/m2. On investigations, his liver function tests, kidney function tests, stool examination, serum proteins and serum lipids were normal. Bowel preparation for colonoscopy was done with split dosing of four liters of polyethylene glycol. Written informed consent was taken from the patient for the procedure as well as to use the data. The colonoscopy procedure was done without sedation and without any apparent complications. The patient tolerated the procedure well and was haemodynamically stable throughout the procedure.
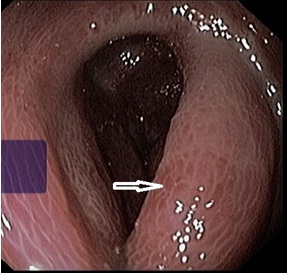
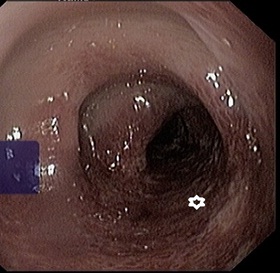
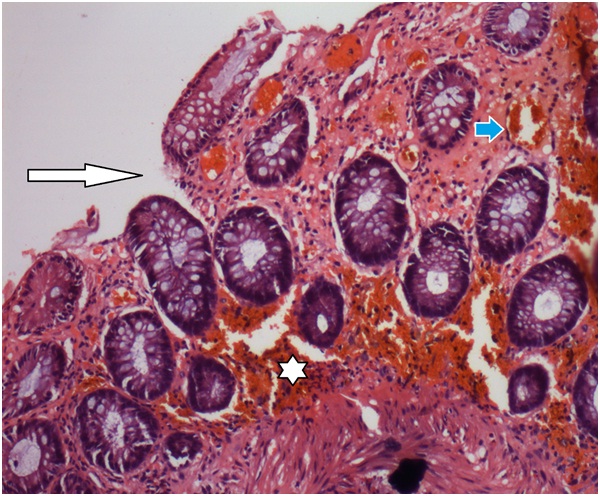
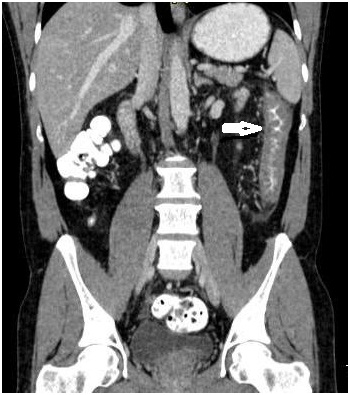
About six hours after index colonoscopy, he complained of haematochezia and lower abdominal pain. He was afebrile and was stable haemodynamically. Abdomen was soft on palpation with some tenderness on the left lower quadrant without signs of peritonitis. Laboratory investigations showed white cell count of 11,900/μL. C-Reactive Protein (CRP) was 0.2mg/dl. Liver and kidney function tests were normal. Stool cultures were negative. He was started on empirical antibiotics, intravenous fluids and analgesics. Roentgenogram as well as ultrasound examination of the abdomen revealed no abnormality. Repeat colonoscopy after 24 hours showed mucosal oedema, irregular ulcerations and submucosal haemorrhages in the region of descending colon and splenic flexure [Table/Fig-1,2]. The biopsy showed oedematous lamina propria with haemorrhages and congested capillaries suggestive of acute ischaemic changes [Table/Fig-3]. Computed tomography of the abdomen showed long segment wall thickening of the descending colon [Table/Fig-4]. The patient was managed conservatively. After 48 hours, his haematochezia and abdominal pain subsided. Flexible sigmoidoscopy was done after seven days to look for improvement and it showed significant decrease in ulcerations as well as inflammation.
Colonoscopy image showing mucosal oedema, in the region of descending colon and splenic flexure (Arrow).
Colonoscopy image showing irregular ulcerations (Asterix) and submucosal haemorrhages in the region of descending colon and splenic flexure.
Colon biopsy with H&E staining showing mucosal breach (white arrow), oedematous lamina propria with haemorrhages (astrix) and congested capillaries (blue arrow) suggestive of acute ischaemic changes.
Computed tomography of the abdomen showing long segment circumferential wall thickening of the descending colon (arrow).
Discussion
Ischaemic colitis is the commonest reason for intestinal ischaemia representing more than 50% of cases with gastrointestinal ischaemia [1]. Elderly patients more than 60 years of age account for as many as 90% of cases of ischaemic colitis [2]. Majority of the cases occur as a result of an acute insult resulting in self-limiting compromise in the intestinal blood flow, which is inadequate to meet the metabolic demands of the colon [3].
A plethora of drugs are known to cause ischaemic colitis including antihypertensive agents, diuretics, non-steroidal anti-inflammatory drugs, pseudoephedrine, cocaine, etc. Predisposing factors in young adults include vasculitis, abdominal surgery, oral contraceptives, hypercoagulable states, colonic obstruction and strenuous physical activities [4].
The patients present with mild crampy abdominal pain usually in left lower abdomen, urge to defecate, passage of bright red blood through anus usually mixed with stools and tenderness over the affected part of the bowel. Blood loss is usually minimal without haemodynamic instability [5]. Fever is unusual and the white cell count is usually raised.
The left colon is most commonly affected in approximately 75% of patients and splenic flexure is the most common site, found in about 25% of the patients [6]. In our case, left colon ischaemia developed involving descending colon and the splenic flexure.
Barium studies show non-specific findings in upto 21% patients which include mucosal thumbprinting, gas filled bowel loops, aperistaltic colon, colonic mural thickening and empty bowel [7]. Abdominal computed tomography may be helpful in the diagnosis of ischaemic colitis in up to 89% of patients demonstrating segmental circumferential wall thickening [5]. Our patient had long segment circumferential wall thickening of the descending colon on computed tomography [Table/Fig-4].
Colonoscopy is the gold standard test to diagnose ischaemic colitis. Zou et al., have noted the endoscopic findings of transient ischaemic colitis in a report of 85 cases which includes segmental erythema, petechial haemorrhages, fragile and oedematous mucosa, ulcerations in the longitudinal axis and sharp demarcation between involved and non-involved bowel segment [8]. The colonoscopy findings in our patient were compatible with ischaemic colitis [Table/Fig-1,2]. Histologic changes seen in acute ischaemic colitis include superficial mucosal necrosis with sparing of deeper crypts, haemorrhage into the lamina propria, pseudomembranes, hyalinization of the lamina propria, intravascular platelet thrombi and necrosis etc., [9]. Supportive care is usually adequate unless signs of peritonitis are present. Patients should be treated with bowel rest, adequate intravenous hydration and empirical antibiotics. It is a rare complication of colonoscopy procedure itself [5]. There are case reports of ischaemic colitis developing after colonoscopy in patients with risk-factors for colonic ischaemia. Wheeldon and Grundman first described a patient with Systemic Lupus Erythematosus (SLE) who developed ischaemic colitis after colonoscopy [10]. Subsequently, a few cases were reported of ischaemic colitis in vasculitides after colonoscopy [11]. A case of ischaemic colitis in an elderly patient on cardiovascular medications was reported by Nowaza et al., [12].
Few cases have been reported in patients without risk-factors [13]. Our patient was a middle aged male and did not have any predisposing conditions.
We believe that colonoscopy itself predisposes the patient to ischaemia due to pressure effect of insufflations and repeated traumas due to scope movements [5]. Reversible circulatory damage in colon occurs when colonic intraluminal pressure rises up to 30-40mmHg, whereas, irreversible damages may occur if the intraluminal pressures rises above 50mmHg [14]. Use of carbon dioxide as an insufflating agent which is rapidly absorbed, and also has vasodilatory effect, may minimize the risk. Decreased intravascular volume due to fasting and colonoscopy preparation and prolonged procedure time may also predispose to colonic ischaemia [13]. Hence, hydration should be maintained to prevent colonic ischaemia in patients with risk-factors.
Conclusion
Ischaemic colitis should be kept in mind by endoscopists as a rare but potential complication of colonoscopy procedure if the patient presents with new onset haematochezia and abdominal pain after colonoscopy. Patients with risk factors for colon ischaemia should receive adequate hydration before the procedure and intra-procedural hypotension should be avoided. Use of carbon dioxide as an insufflating agent may decrease the risk of post-colonoscopy ischaemic colitis.
[1]. Greenwald DA, Brandt LJ, Colonic ischemiaJ ClinGastroenterol 1998 27:122-28. [Google Scholar]
[2]. Theodoropoulou A, Koutroubakis IE, Ischemic colitis: Clinical practice in diagnosis and treatmentWorld Journal of Gastroenterology 2008 14(48):7302-08. [Google Scholar]
[3]. Tendler DA, Acute intestinal ischemia and infarctionSemin Gastrointest Dis 2003 14:66-76. [Google Scholar]
[4]. Brandt LJ, Boley SJ, Colonic ischemiaSurg Clin North Am 1992 72:203-29. [Google Scholar]
[5]. Green BT, Tendler DA, Ischemic colitis: a clinical reviewSouth Med J 2005 98:217-22. [Google Scholar]
[6]. Gandhi SK, Hanson MM, Vernava AM, Kaminski DL, Longo WE, Ischemic colitisDis Colon Rectum 1996 39:88-100. [Google Scholar]
[7]. Green BT, Stanley Branch M, Ischemic colitis in a young adult during sickle cell crisis: case report and reviewGastrointestinal Endoscopy 2003 57(4):605-07. [Google Scholar]
[8]. Zou X, Cao J, Yao Y, Liu W, Chen L, Endoscopic findings and clinicopathologic characteristics of ischemic colitis: a report of 85 casesDig Dis Sci 2009 54:2009-15. [Google Scholar]
[9]. Lisa A. Cerilli, Joel K. Greenson, The differential diagnosis of colitis in endoscopic biopsy specimens: a review articleArchives of Pathology & Laboratory Medicine 2012 136(8):854-64. [Google Scholar]
[10]. Wheeldon NM, Grundman MJ, Ischaemic colitis as a complication of colonoscopyBMJ 1990 301:1080-81. [Google Scholar]
[11]. Lee JR, Paik CN, Kim JD, Chung WC, Lee KM, Yang JM, Ischemic colitis associated with intestinal vasculitis: histological proof in systemic lupus erythematosusWorld J Gastroenterol 2008 14:3591-93. [Google Scholar]
[12]. Nozawa H, Akiyama Y, Sunaga S, Tsurita G, Ischemic colitis following colonoscopy in an elderly patient on cardiovascular medicationEndoscopy 2007 39:E344-45. [Google Scholar]
[13]. Cremers MI, Oliveira AP, Freitas J, Ischemic colitis as a complication of colonoscopyEndoscopy 1998 30:54 [Google Scholar]
[14]. Park JE, Moon W, Nam JH, Kim NH, Kim SH, Park MI, A case of ischemic colitis presenting as bloody diarrhea after normal saline enemaKorean J Gastroenterol 2007 50:126-30. [Google Scholar]