Management of Recurrent Odontogenic Myxoma of Mandible: A Clinical Case Report
Yogesh Mittal1, Ankita Chugh2, K George Varghese3, Shailendra Dwivedi4, Vidhi Goyal5
1 Senior Resident, Department of Trauma and Emergency, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
2 Assistant Professor, Department of Dentistry, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
3 Principal and Professor, Department of Oral and Maxillofacial Surgery, Government Dental College, Kottayam, Kerala, India.
4 Senior Resident and Postdoctoral Fellow, Department of Biochemistry, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
5 Postgraduate Student, Department of Prosthodontics, Crown and Bridge, Manipal College of Dental Sciences, Manipal, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Yogesh Mittal, Room No. 315 Resident Hostel AIIMS Residential Complex, All India Institute of Medical Sciences, Jodhpur, Rajasthan, India.
E-mail: dryogesh82@gmail.com
Odontogenic Myxoma (OM) is a slow growing painless locally aggressive tumor seen in gnathic bones and is generally asymptomatic. OM is characterized by spindle, wedge or stellate shaped cells loosely arranged in an abundant mucoid stroma. It is found incidentally on radiographs and may vary from a unilocular radiolucency to a multilocular lesion with well-defined or diffuse margins. Treatment includes surgical management that may range from simple enucleation and curettage to surgical excision including peripheral osteotomy, segmental resection, hemimandibulectomy and maxillectomy. Here we are presenting a case report on odontogenic myxoma with recurrence after conservative treatment.
Fine needle aspiration cytology, Reconstruction Plate, Segmental Resection
Case Report
A 48-year-old female reported to the Department of Oral and Maxillofacial Surgery, with chief complaint of mild pain and gradually increasing swelling of right lower front tooth region since five months. There was no history of trauma and infection. The past medical and dental history was non-contributory. Pain was intermediate and usually occurred while eating. Extra-oral examination revealed a swelling measuring approximately 2.5x 2cm in size, extending from midline of lower lip to corner of mouth and inferiorly till the lower border of chin. Colour, texture and temperature of overlying skin were normal and there was no complain of paresthesia. Intra-oral examination showed a firm, non-tender swelling with labial plate expansion extending from right lower over retained deciduous second molar to left lower central incisor and it obliterated the labial vestibule [Table/Fig-1a]. Overlying mucosa was smooth and shiny with slight black discoloration of attached gingiva. There was missing second right lower premolar and associated teeth had low degree of mobility.
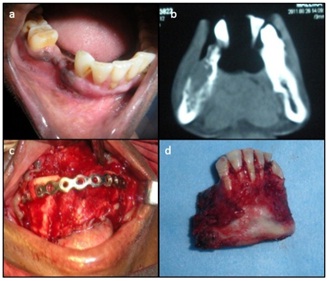
(a) Intraoral swelling over the right lower vestibule; (b) OPG showed a large well defined, sclerotic margin and multilocular radiolucent lesion; (c) Enucleation of tumour along with bony curettage; (d) Histopathology report showing loosely arranged spindle shaped stellate and round cells.

The Ortho-Pantomo-Graph (OPG) showed a large well defined multilocular radiolucent lesion with sclerotic margin and “soap bubble” appearance extending from root tip of impacted right mandibular second premolar to left mandibular canine anteriorly and inferiorly up to the lower border of chin along with displacement of roots [Table/Fig-1b]. Differential diagnosis was given as odontogenic tumour, ameloblastoma, aneurysmal cyst and giant cell lesion. To rule out odontogenic cyst Fine Needle Aspiration Cytology (FNAC) was performed initially which came out to be negative. Then benign odontogenic tumours were considered and incisional biopsy was planned under local anaesthesia. Histopathological examination showed cellular myxoid tissue with one nest of odontogenic cells in a homogenous pale eosinophilic background, a fragment of globular calcification, numerous endothelium lined capillary spaces and few thin walled arterioles, reported it as an Odontogenic Myxoma (OM). Segmental resection of the anterior mandible was planned under General Anesthesia (GA). Treatment plan was explained to the patient but the attendants of patient requested for a more conservative approach. Patient was explained high chance of recurrence of tumour and subsequently the new treatment of enucleation and curettage of lesion was planned under GA. Under sterile and aseptic condition a crevicular along with vertical releasing incision was given from right lower first molar to left lower first premolar. Mucoperiosteal flap was elevated and complete enucleation of tumour along with bony curettage and extraction of involved teeth was done [Table/Fig-1c]. Specimen was sent for histopathological examination. Loose arrangement of spindle shaped stellate cells was seen during histopathological examination which confirmed the incisional biopsy report as OM. [Tabe/Fig-1d]. Post-operative period and wound healing was uneventful [Table/Fig-2a]. Patient was recalled every two months for follow-up. After two years patient developed recurrence of the tumour and 3D Computed Tomgraphy (CT) scan showed insufficient bone formation [Table/Fig-2b]. After that we planned segmental resection of mandible under GA and reconstruction with stainless steel reconstruction plate without any graft [Table/Fig-2c,2d]. Under sterile and aseptic conditions an intra-oral crevicular and crestal incision along with vertical releasing incision was given from right lower second molar to left lower first molar. Mucoperiosteal flap was elevated to expose the lower border of mandible and 2.5mm long reconstruction plate was adapted over the lower border of mandible before resection to avoid the occlusal and facial symmetry after post-operative period. Segmental resection done from right first molar to left first premolar with gigli saw and reconstruction plate fixed in good occlusal condition. Post-resection OPG showed no recurrence of tumour after three years follow-up [Tabe/Fig-3].
(a) Post-operative wound healing after one month; (b) CT scan showing recurrence of lesion with insufficient bone formation; (c) Segmental resection of mandible and reconstruction with stainless steel reconstruction plate; (d) Specimen of resected segment.
Postoperative OPG showing segmental resection with reconstruction plate.

Discussion
Odontogenic myxoma is a tumour of jaw bone which is locally invasive and aggressive, benign and non-metastasizing in nature. It is derived from embryonic mesenchymal tissue of dental anlage like dental papilla, follicle or periodontal ligament [1,2]. World Health Organization (WHO), classified OM as a benign tumour which was ectomesenchymal in origin with or without odontogenic epithelium. Thoma and Goldman were the first ones to describe OM of jaw in 1947. It is a non-encapsulated benign tumor that allows substantial infiltration into the adjacent medullary bone and has a high recurrence rate and histologically consists of rounded and angular cells that lie in abundant mucoid stroma [3]. Most of the OM cases show marked female predilection and are usually reported in 2nd or 3rd decade of life [1,4]. Odontogenic myxoma can be grouped in two categories, first is the most common type arising specifically in the jaw bones and the second category include those arising from the soft tissues. Despite the reports of odontogenic myxoma in various anatomic sites, two third of these tumour presents in posterior mandible usually in molar ramus area and one third presents in the maxilla [5,6]. It is usually found incidentally on radiographs and may vary from a unilocular radiolucency to a multicystic lesion with well-defined or diffuse margins expressing as a “soap bubble,” “honey combed” or “tennis racket” appearance [1,7]. Larger lesions may cause tooth displacement and cortical bone expansion and rarely root resorption is seen [8]. Histopathological examination of the peripheral area reveals the presence of residual bone in trabecular spaces because of myxomatous tissue penetration and thus, explaining why it is difficult to remove this tumour in a conservative manner. Chondroitin sulfate and hyaluronic acid are the two mucopolysaccharides which are seen in this type of tumour [9,10]. Radiographic examination reveals unilocular or multilocular radiolucency with either diffuse or well defined margins [11]. Other clinically similar conditions like ameloblastoma, giant cell lesion, intra-osseous hemangioma, odontogenic cyst and osseous aneurysmal cyst helps establishing the differential diagnosis [12,13]. The current recommended treatment depends on the size, site of the lesion and its nature and behavior, proximity of vital structure as well as age of the patient, degree of functional and aesthetic compromise acceptance. The other treatment options available for more aggressive lesions are peripheral ostectomy, radical resection or segmental resection [13]. Reconstruction can be done immediately following the surgical procedure or delayed until an adequate disease free period has passed. Smaller defects of size less than 5cm are reconstructed using cortico-cancellous iliac crest bone graft or buccal fat pad in maxilla whereas the larger defects of size more than 5cm require prosthetic reconstruction by obturator in maxilla and reconstruction plate followed by immediate or delayed vascularized fibular free flap, costochondral graft, scapular osteocutaneous free flap or iliac crest graft in mandible.
Conclusion
Odontogenic myxoma being locally invasive, aggressive tumour with a high recurrence tendency should preferably be treated according to the size, site and behaviour of the tumour, so as to provide for adequate clear margins to avoid recurrence and further patient morbidity due to repeated interventions. Hence, to conclude, we say that in a locally aggressive tumour delayed reconstruction should be the treatment of choice because of high recurrence rates of these types of lesions.
[1]. Sivakumar G, Kavitha B, Saraswathi T, Sivapathasundharam B, Odontogenic myxoma of maxillaIndian J Dent Res 2008 19:62-65. [Google Scholar]
[2]. Shah A, Lone P, Latoo S, Ahmed I, Malik A, Hassan S, Odontogenic myxoma of the maxilla: A report of a rare case and review on histogenetic and diagnostic conceptsNatl J Maxillofac Surg 2011 2(2):189-95. [Google Scholar]
[3]. Kramer IRH, Pindborg JJ, Shear M, Histological Typing of OdontogenicTumours 1992 2nd edBerlinSpringer Verlag:23 [Google Scholar]
[4]. Reddy S. P, Naag A, Kashyap B, Odontogenicmyxoma: Report of two casesNatl J Maxillofac Surg 2010 1:183-86. [Google Scholar]
[5]. Khogare S, Deshpande DM, Malik NA, Odontogenic myxoma: A case studyInt J Oral Maxillofac Surg 2007 16:107 [Google Scholar]
[6]. Dabbaghi A, Nikkerdar N, Soheyla Bayati S, Golshah A, Rare appearance of an odontogenic myxoma in cone-beam computed tomography: A case reportJ Dent Res Dent Clin Dent Prospect 2016 10(1):65-68. [Google Scholar]
[7]. Singaraju S, Wanjari S.P, Parwani R.N, Odontogenicmyxoma of the maxilla: A report of a rare case literatureJOMFP 2010 14:19-23. [Google Scholar]
[8]. Spencer K.R, Smith A, Odontogenic myxoma.: Case report with reconstructive considerationsAust DentJ 1998 43(4):209-12. [Google Scholar]
[9]. Landa LE, Hedrick MH, Nepomuceno-Perez MC, Sotereanos GC, Recurrent myxoma of the zygoma: A case reportJ Oral Maxillofac Surg 2002 60(6;704):08 [Google Scholar]
[10]. White DK, Chen S, Mohnac AM, Miller AS, Odontogenic myxoma: A clinical and ultrastructural studyOral Surg 1975 39(6):901-17. [Google Scholar]
[11]. Bucci E, Lo Muzio L, Mignogna MD, De Rosa G, Odontogenic myxoma: Report of a case with peculiar featuresJ Oral Maxillofac surg 1991 49:91-94. [Google Scholar]
[12]. Peltola J, Magnusson B, Happoren RP, Bomen H, Odontogenic myxoma-A radiological study of 21 tumorsBr J Oral Maxillofac surg 1994 32:298-302. [Google Scholar]
[13]. Hernández Vallejo G, Cohn C, GarcíaPeñín A, Martínez Lara S, Llanes Menéndez F, Montalvo Moreno JJ, Myxomas of the jaws: Report of three casesMed Oral 2001 6:106-13. [Google Scholar]