Eosinophilic Granuloma Presenting as Palatal Swelling
B. Balaji Babu1, Lakshmi Kavitha Nadendla2, Ginjupally Uday3, Pooja Madki4
1 Professor and Head, Department of Oral Medicine and Radiology, Kamineni Institute of Dental Sciences, Narketpally, Telangana, India.
2 Reader, Department of Oral Medicine and Radiology, Kamineni Institute of Dental Sciences, Narketpally, Telangana, India.
3 Senior Lecturer, Department of Oral Medicine and Radiology, Kamineni Institute of Dental Sciences, Narketpally, Telangana, India.
4 Postgraduate Student, Department of Oral Medicine and Radiology, Kamineni Institute of Dental Sciences, Narketpally, Telangana, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ginjupally Uday, S/O Mallikarjuna Rao, H.No. 5-10, Thallampadu, Khammam– 507170, Andhra Pradesh, India.
E-mail: uday2361@gmail.com
Swellings involving palate can be challenging to diagnose for the clinician as they have wide range of origin which can result from developmental, inflammatory, reactive or a neoplastic process. The clinical presentation of these swellings is similar and difficult to differentiate from each other. So it is important to take proper history from the patient and subject the patient to appropriate laboratory and radiographic investigations and finally biopsy is mandatory for accurate diagnosis. Thus, this article highlights on various common palatal swellings, their clinical presentation, and differential diagnosis helpful for proper diagnosis of swellings associated with palate.
Aspiration, Biopsy, Lymph nodes, MRI scan, Pain
Case Report
A 32-years-old male patient reported to Department of Oral Medicine and Radiology, with a complaint of pain and swelling in his palate since three months. History revealed bleeding gums from upper right back teeth region followed by pain and swelling since two months. Patient had a history of cigarette smoking since 20 years, five cigarettes per day.
Face appeared to be symmetrical extra-orally. Single right submandibular and upper cervical lymph nodes palpable of size measuring approximately 2x2cm which were tender, movable and firm in consistency.
Intra-orally a diffuse swelling was found on right half of the palate measuring approximately 4x3cm and extending from maxillary right first premolar to distal aspect of right maxillary 3rd molar. Surface of the swelling appeared to be erythematous with ulcerations of size 0.2x0.2cm surrounded by erythematous halo and floor of the ulcer was covered by yellowish slough. On palpation swelling was tender and of variable consistency [Table/Fig-1]. Because the lesion was on the posterior lateral aspect of hard palate, minor salivary gland tumor was given first priority for the clinical diagnosis.
Palatal swelling with surface ulcerations.

Differential Diagnosis: The differential diagnoses that could be considered for the present case are presented in [Table/Fig-2].
Differential diagnoses of palatal swellings.
| Condition | Differential Diagnosis |
|---|
| Palatal abscess | Possibility of palatal abscess was ruled out due to absence of signs of inflammation. |
| Carcinoma of maxillary sinus | Presents with palatal swelling but it is associated with chronic unilateral nasal stuffiness which was lacking in our case |
| Reactive lesions of palate | No aetiologic irritation factor was found in this case |
| Torus palatinus | Occurs in the midline of the hard palate but the discussed case was not a midline one and consistency of this lesion is bony hard and in the present case it was variable. |
| Vascular lesions | Vascular lesions were excluded because the swelling in the present case didn’t blanch on diascopy and vascular lesions are usually reddish-blue in color. |
| Hodgkin’s and non-Hodgkin’s lymphomas | These lesions can present as palatal mass with ulcerations but these are rare in the palate region and usually they are rapidly progressing and present as a poorly defined mass. |
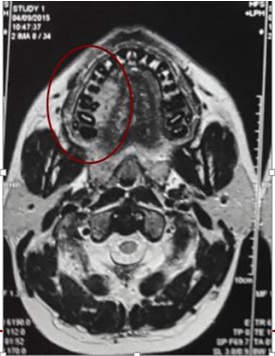
Following set of investigations were done which consist of aspiration, maxillary occlusal radiograph, Orthopantomograph (OPG), Magnetic Resonance Imaging (MRI) was done. Aspiration was negative. Maxillary occlusal view [Table/Fig-3], OPG [Table/Fig-4] did not reveal any bony changes. MRI showed cortical destruction involving lingual cortex of the right side of maxilla near premolar and molar tooth with a soft tissue mass in the hard palate and bilateral level 2 and level 3 lymphnodes were noted [Table/Fig-5].
Maxillary occlusal radiograph showing no bony changes.
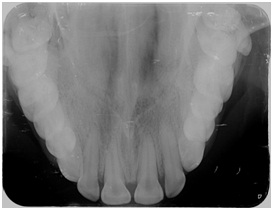
OPG showing no bony changes.

MRI showing cortical destruction on right side of palate.
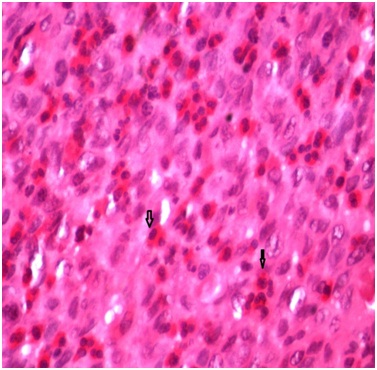
Diagnosis: Biopsy of the palatal mass was done and submitted for histopathologic examination under 40X view, which revealed ulcerated oral epithelium with underlying lesion composed of tumor cells with epitheloid and spindling nuclei with moderate amount of eosinophilic cytoplasm along with numerous vascular spaces lined by plump endothelial cells. Few cells exhibited dysplastic features along with mitotic figures and collection of inflammatory cells in ulcerated area admixed with numerous eosinophils in underlying stroma [Table/Fig-6]. Based on microscopic findings, diagnosis of eosinophilic granuloma was given. Patient was referred to regional cancer institute and he was treated by surgical curettage. After a period of follow-up of six months, no recurrence was noted.
Photomicrographunder 40 X showing numerous eosinophils and vascular channels.
Discussion
Langerhans Cell Histiocytosis (LCH) is a group of disorders containing three clinical variants: Eosinophilic granuloma, Hand-Shuller-Christian disease and Letterer-Siwe disease. Though the latter two are more generalized and serious forms, eosinophilic granuloma is a localized form [1]. Eosinophilic granuloma is one of the rarest bone tumors representing less than 1% of them. The mandible is a more commonly affected site than the maxilla [2]. Present case is unique because eosinophilic granuloma of palate is extremely rare. In 90% of the reported cases it appears in children under the age of 10 years [3]. However, the presented case was an adult male patient. The patients usually report with complaints like bone pain, swelling, ulcerations, necrosis of gingiva and destruction of alveolar bone resulting in mobility or loss of teeth [4]. However, in our case patient presented with pain and swelling in palate region without any mobility of involved teeth apart from mild periodontal pocket and bleeding from gums and ulcerations over the swelling.
Most common radiographic presentation of eosininophilic granuloma is an osteolytic lesion with well-defined border but poorly defined in some cases. Other radiographic features are destruction of alveolar bone which gives “floating tooth appearance” [5]. Present case didn’t reveal significant bony changes in maxillary occlusal radiograph and OPG. MRI showed cortical destruction involving lingual cortex. This lesion may be confused with chronic inflammation, odontogenic cyst, osteomyelitis, malignant lymphoma and metastatic bone diseases etc., [6]. However, a definitive diagnosis needs to be determined by correlation of the clinical findings with the histologic features [7].
There are several accepted forms of treatment for eosinophilic granuloma. Surgical curettage, local irradiation, and chemotherapy have all been used, alone or in combination, with favorable results [8]. Surgery is the preferred method of treatment for a single and localized manifestation of the disease. Radiotherapy is suggested in cases of local recurrence or if surgical treatment is not possible [9]. Chemotherapy with methotrexate and vinblastin, with prednisolone, is recommended for the diffuse form of the condition [10].
Conclusion
Early clinical signs of eosinophilic granuloma are often ignored as the disease appears either to be symptomless or exhibit manifestation of minor degree like pain and swelling. Hence, eosinophilic granuloma should be considered as one of the differential diagnoses for lesions presenting with palatal swellings. For definitive diagnosis and selection of treatment plan appropriate imaging modalities and careful histopathological examination is required.
[1]. Yashoda V, Reddy ESK, Bhavani SN, Krishna A, Shekhar MS, Solitary extragnathic langerhans cell histiocytosis – A rare caseJ Clin Diagn Res 2015 9(3):ZD22-33. [Google Scholar]
[2]. Seema S, Pranav S, Shetty DC, Aadithya Urs B, A case of multiple eosinophilic granulomas of jaws: A diagnostic challengeInt J Oral Maxillofac Pathol 2012 3(3):37-40. [Google Scholar]
[3]. Agarwal A, Agarwal GP, Alam S, Husain B, A case of unifocaleosinophilic granuloma of the mandible in an adult female: A case reportCase Rep Dent 2012 2012:521726 [Google Scholar]
[4]. Vandana KL, Desai R, Banupurmath CR, Karthik M, Eosinophilic granuloma with oral manifestations: A case reportJ Indian Soc Pedo Prev Dent 2003 21(3):105-07. [Google Scholar]
[5]. Lee BD, Lee W, Lee J, Son HJ, Eosinophilic granuloma in the anterior mandible mimicking radicular cystImaging Sci Dent 2013 43:117-22. [Google Scholar]
[6]. Fonseca N, Saikrishna D, Eosinophilic granuloma of mandible: A report of two casesJournal of Orofacial Research 2014 4(4):234-38. [Google Scholar]
[7]. Atri R, Dhankhar R, Dhull AK, Nair VJ, Kaushal V, Alveolar Langerhans cell histiocytosis - A case reportJ Oral Health Comm Dent 2008 2(1):16-18. [Google Scholar]
[8]. Ardekian L, Peled M, Rosen D, Rachmiel A, Abuel-Naaj I, Laufer D, Clinical and radiographic features of eosinophilic granuloma in the jaws. Review of 41 lesions treated by surgery and low-dose radiotherapyOral Surg Oral Med Oral Pathol Oral Radiol Endod 1999 87(2):238-42. [Google Scholar]
[9]. Divya KS, Oral manifestion of langerhans cell histiocytosis mimicking inflammationIndian J Dent Res 2014 25:228-30. [Google Scholar]
[10]. Pazhutan M, Sakhdari Sh, Mashhadiabbas F, Afghahi M, Khodaei F, Langerhan’s cell histiocytosis with multiple radiolucent lesions in the body of the mandible: Report of a caseCaspian J Dent Res 2014 3:52-56. [Google Scholar]