Subperiosteal Schwannoma of Pelvis- A Rare Case and Review of Literature
Devendra Lakhotia1, Sunil Jeph2, Swati Sharma3
1 Assistant Professor, Department of Orthopaedics, Institute for Medical Sciences and Research Centre, Jaipur National University, Jagatpura, Jaipur, Rajasthan, India.
2 Senior Resident, Department of Orthopaedics, Institute for Medical Sciences and Research Centre, Jaipur National University, Jagatpura, Jaipur, Rajasthan, India.
3 Junior Resident, Department of Medicine, Holy Family Hospital, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Devendra Lakhotia, Assistant Professor, Department of Orthopaedics, Institute for Medical Sciences and Research Centre, Jaipur National University, Jagatpura, Jaipur-302017, Rajasthan, India.
E-mail: drdevendra.ortho@gmail.com
Schwannoma are benign tumours of the nerve sheath. They are commonly found in the soft tissue, but its presence in the bone is extremely rare. We herein present a case of 34-year-old man with two adjacent pelvic subperiosteal schwannomas. Computed Tomography (CT) scan showed osseous pressure erosion and Magnetic Resonance Imaging (MRI) showed two cystic signal intensity lesions, one near superior aspect of right posterior iliac wing and another inferior to it with adjacent cortical pressure erosion. The tumour was excised en bloc and on histopathological examination, the diagnosis was confirmed as subperiosteal schwannoma. To our knowledge, this is the first case report of subperiosteal schwannoma involving the pelvis. When a surface cystic lesion is encountered, subperiosteal schwannoma should be considered as a possible differential diagnosis.
Benign tumours, Nerve sheath, Posterior pelvis, Sacroiliac joint
Case Report
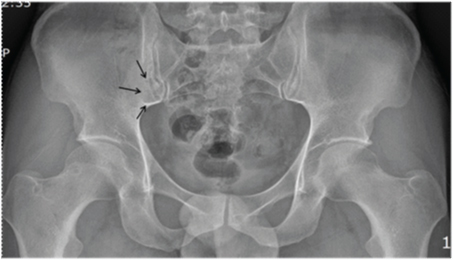
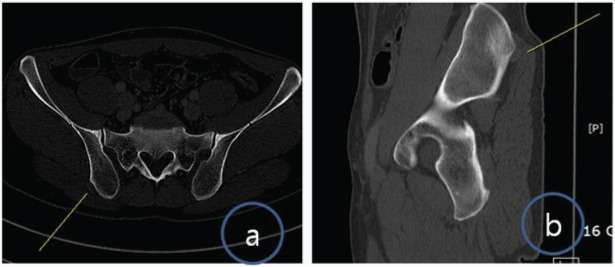
A 34-year-old man presented with pain in posterior pelvis near the right sacroiliac joint for last three months. Although there was no visible swelling but a small tender swelling felt on deep palpation. It was pea-sized and fixed. The surrounding skin was normal. There was no other swelling, café-au-lait spot or cutaneous neurofibroma. He had no significant past medical or family history. There were no other constitutional symptoms such as low grade fever, chills, or weight loss. Anteroposterior pelvic radiograph showed an ill-defined lytic lesion with non-sclerotic margins near inferior aspect of right sacroiliac joint. There was no sub-periosteal reaction or new bone formation [Table/Fig-1]. CT scan pelvis showed two small nodular soft tissue density lesions near right posterior iliac wing (about 1.1 cm in size) with osseous pressure erosion [Table/Fig-2a,b].
Anteroposterior pelvic radiograph demonstrates lytic lesion near inferior aspect of right sacroiliac joint (indicated by multiple arrows).
(a) Transverse CT scan demonstrates small nodular soft tissue density lesion near right posterior iliac wing with slight osseous pressure erosion; (b) Sagittal CT scan demonstrates small nodular soft tissue density lesion near right posterior iliac wing.
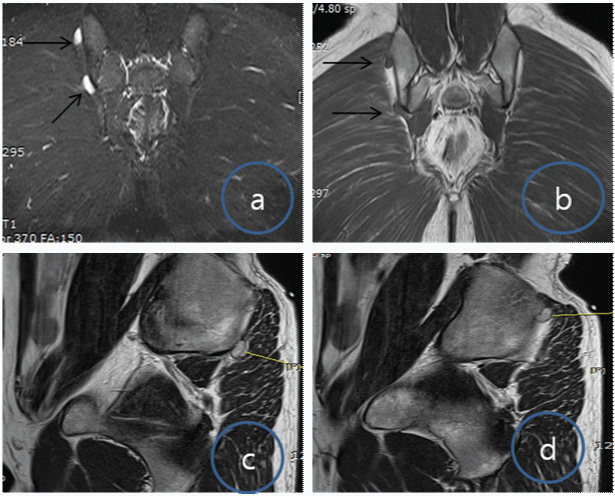
MRI showed two surface cystic lesion arising near right posterior iliac wing, one superior and other inferior [Table/Fig-3a-d]. Lesions were isointense on T1 and hyperintense on T2 MRI images. The size of the elongated cystic signal intensity lesions were 1.5 x 1 cm x 0.8 cm and 1.2 x 1 x 0.5cm respectively with adjacent cortical pressure erosion.
(a,b) Coronal T1 and T2-weighted image of the pelvis showing two small elongated soft tissue masses, isointense on T1 and hyperintense on T2 (arrows); (c,d) Sagittal T1 weighted image of the pelvis showing isointense small soft tissue masses, lying on posterior iliac wing near sacroiliac joint at two different levels (line).
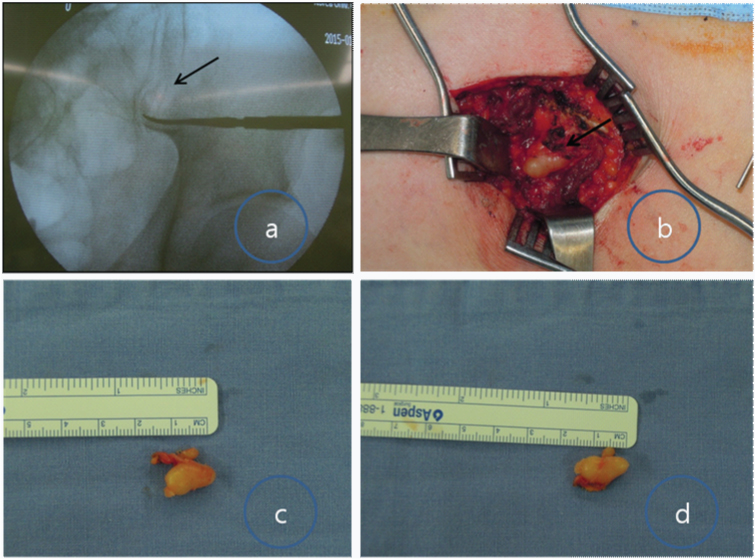
Excisional biopsy of the lesion was performed. The lesion was approached through posterior vertical incision over the sacrum after localization under the C- arm [Table/Fig-4a]. The swelling was well embedded in the pelvis and was completely excised. There were two yellowish firm nodular lesions [Table/Fig-4b] of about 20mm x 10mm x 8 mm and 15mm x 10mm x 5mm respectively and appeared to be arise from the bone. These were well-encapsulated glistening lesions which were scalloped into the pelvis. These were excised in one piece without compromising the surrounding normal tissues [Table/Fig-4c,d].
(a) Intraoperative localization of the lesion using C- arm; (b) Intraoperative photograph showing subperiosteal location of lesion near sacroiliac joint; (c,d) enbloc excised glistening yellow lesion.
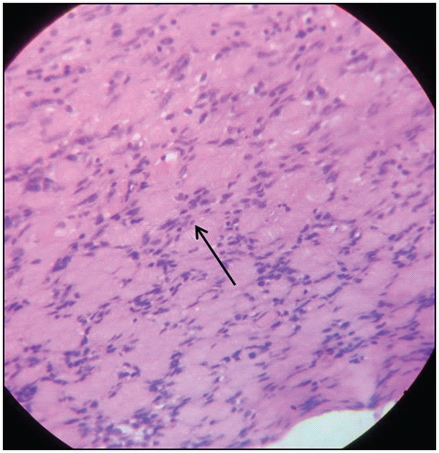
Histological examination showed that they were subperiosteal cellular benign schwannoma [Table/Fig-5]. It revealed well-encapsulated lesions composed of spindle shaped cells with thin wavy spindle nuclei. Hypo- and hyper-cellular areas (Antoni A and B) were seen together with nuclear palisading (Verocay bodies). No mitoses were identified and there was no necrosis. The lesions showed diffuse strong expression of S100 by immunohistochemistry (IHC). The patient’s post-operative recovery was uneventful and remained asymptomatic till last follow-up.
H&E stain (×100) shows abundant spindle cells (Antoni A pattern) with elongated nuclei arranged in a well organizing palisading pattern (arrow) surrounding pink areas (Verocay bodies).
Discussion
Schwannomas are common benign peripheral nerve tumours arising from schwann cells of the nerve sheath [1]. Intraosseous schwannomas account for less than 1% of primary bone tumours [2] and its subperiosteal location is still more uncommon. The average age of presentation is 40–60years with equal involvement of both the gender [3]. In the present case the age of the patient was 34years.
There are numerous case reports of intraosseous schwannoma [4–7] especially as intramedullary locations. We presented a rare case of a subperiosteal schwannoma in the pelvis. There are only few case reports [Table/Fig-6] with subperiosteal schwannoma [8–12]. All the cases were in young age group (20-40years of age) with equal involvement of both the genders. Most of these cases presented with vague pain. The presentation in the form of swelling depends on the location. The cases with involvement of ulna, tibia and humerus presented with palpable swelling whereas femur and pelvis (present case) presented with no swelling. There were two types of radiological findings, one with periosteal reaction and other without it. Most of the cases had delayed presentation of more than one year due to deep location, muscle mass and small size. In our case the patient presented at 3 months. With proper clinical examination and radiological imaging, we were able to locate the lesion although the definitive diagnosis was made only after the histological analysis. The differential diagnosis on the basis of clinical presentation and imaging are periosteal chondromas, periosteal ganglia, epidermoid cyst, subperiosteal hematoma and a surface Aneurysmal Bone Cyst (ABC) [13].
Summary of cases of subperiosteal schwannoma at different locations.
| Authors | Age | Sex | Location | Periostealreaction | Year | Presentation | Radiography | Delayed presentation |
|---|
| Suvana SK et al., [8] | 22 | Female | Tibia | Present | 1995 | Painless lump | Broad based exostosis | 1 year |
| Paksoy y et al., [9] | 30 | Female | humerus | Present | 2002 | Painful swelling | Soft tissue swelling with periosteal reaction | Long duration (non specified) |
| Verma RR eta al., [10] | 38 | Male | Femur | Absent | 2002 | Pain with no swelling | Smooth scalloping of cortex | 4 years |
| Singh V et al., [11] | 28 | Female | Ulna | Absent | 2005 | Painful swelling | Cystic lesion with Well defined sclerotic margin | Long duration (non specified) |
| Patro BP et al., [12] | 35 | Male | Femur | Absent | 2014 | Painful swelling | Normal | 2 years |
| Present case | 34 | Male | Pelvis | Absent | 2016 | Painful with no swelling | Illdefined lytic lesion | 3 months |
Schwannoma can involve bone by three mechanisms: 1) secondary erosion by an extraosseous tumour; 2) tumour arising from a nerve coursing through a canal in a bone and causing erosion of the bone, creating a dumbbell-shaped configuration; or 3) tumour arising centrally (intramedullary) in a bone [2,5,7,14–16]. The first two mechanisms occur most frequently. But in our case the there is fourth mechanism of subperiosteal origin as seen in MRI section. The periosteum has numerous nerve fibres explaining the subperiosteal location of schwannoma in our present case. But it is difficult to explain the rarity of such lesion in the literature. The clinical presentation and the imaging findings are insufficient for definitive diagnosis. These are only confirmed after the histological studies. Therefore, such lesions in the subperiosteal location need to be excised en block completely to minimize the chances of recurrence or malignant change.
Conclusion
Subperiosteal schwannoma in the pelvis is very rare. It is difficult to clinically diagnose it due to deep location and non-specific symptoms. Subperiosteal schwannoma should be included in the differential diagnosis in the patient with diffuse pain around the pelvis.
[1]. Enzinger F, Weiss SW, Benign Tumours of Peripheral Nerves. In: Weiss SW, Goldlum JR, editorsSoft tissue tumours 2008 St LouisMosby:853-69. [Google Scholar]
[2]. Fawcett KJ, Dahlin DC, Neurilemmoma of boneAm J Clin Pathol 1967 47:759-66. [Google Scholar]
[3]. Mangulkar VH, Brunetti VA, Gould ES, Howell N, Unsually large pedal schwannomaJ Foot Ankle Surg 2007 46:398-402. [Google Scholar]
[4]. Aoki J, Tanikawa H, Fujioka F, Shii K, Seo GS, Karakida O, Intraosseous neurilemmoma of the fibulaSkeletal Radiol 1997 26(1):60-63. [Google Scholar]
[5]. Gine J, Calmet J, Sirvent JJ, Domenech S, Intraosseous neurilemmoma of the radius: a case reportJ Hand Surg [Am] 2000 25(2):365-69. [Google Scholar]
[6]. Vora RA, Mintz DN, Athanasian EA, Intraosseous schwannoma of the metacarpalSkeletal Radiol 2000 29(4):224-26. [Google Scholar]
[7]. Mutema GK, Sorger J, Intraosseous schwannoma of the humerusSkeletal Radiol 2002 31(7):419-21. [Google Scholar]
[8]. Suvarna SK, Smith JHF, Barrington NA, Periosteal neurofibroma mimicking osteochondromaClin Radiol 1995 50:800-02. [Google Scholar]
[9]. Paksoy Y, Sahin M, Avunduk MC, Aksoy F, Odev K, Solitary juxtacortical neurofibroma of the humerusSkeletal Radiol 2002 31:112-15. [Google Scholar]
[10]. Verma RR, Khan MT, Davies AM, Mangham DC, Grimer RJ, Subperiosteal schwannomas of the femurSkeletal Radiol 2002 31:422-25. [Google Scholar]
[11]. Singh V, Grimer R, Subperiosteal schwannoma of the ulnaThe Internet Journal of Orthopedic Surgery 2005 3(1) [Google Scholar]
[12]. Patro BP, Patra SK, Panda S, Jagatjit Sahu MC, Atypical presentation of subperiosteal neurilemomaInt J Pharm Sci Rev Res 2014 27(2):387-88. [Google Scholar]
[13]. Seeger LL, Lawrence Y, Eckardt JJ, Surface lesions of boneRadiology 1998 206:17-33. [Google Scholar]
[14]. de la Monte SM, Dorfman HD, Chandra R, Malawer M, Intraosseous schwannoma: histologic features, ultrastructure, and review of the literatureHum Pathol 1984 15(6):551-58. [Google Scholar]
[15]. Palocaren T, Walter NM, Madhuri V, Gibikote SJ, Schwannoma of the fibulaBone Joint Surg Br 2008 90(6):803-05. [Google Scholar]
[16]. Sufian Z, Mazhar A, Lateef JZ, Rana SK, Intraosseous schwannoma of head of first metatarsal: A rare entityIndian J Pathol Microbiol 2009 52:286-88. [Google Scholar]