Cystadenoma in Retromolar Region: A Case Report
Sheetal1, V Ramesh2, PD Balamurali3, B Premalatha4, Monika Chaudhary5
1 Postgraduate Student, Department of Oral Pathology and Microbiology, Mahatma Gandhi Postgraduate Institute of Dental Sciences, Puducherry, India.
2 Dean and HOD, Department of Oral Pathology and Microbiology, Mahatma Gandhi Postgraduate Institute of Dental Sciences, Puducherry, India.
3 Professor, Department of Oral Pathology and Microbiology, Mahatma Gandhi Postgraduate Institute of Dental Sciences, Puducherry, India.
4 Senior Lecturer, Department of Oral Pathology and Microbiology, Mahatma Gandhi Postgraduate Institute of Dental Sciences, Puducherry, India.
5 Associate Professor, Department of Oral Pathology and Microbiology, Mahatma Gandhi Postgraduate Institute of Dental Sciences, Puducherry, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Monika Chaudhary, Mahatma Gandhi Postgraduate Institute of Dental Sciences, Gorimedu-605006, Puducherry, India.
E-mail: monikararh@gmail.com
Cystadenoma is a rare benign salivary gland epithelial tumor that is characterized by intraluminal papillary projection. Majority of the tumors are located in minor salivary glands and usually occur in palatal and buccal mucosa, but rarely found in retromolar area. Clinically it is difficult to differentiate it from other minor salivary gland tumors, and diagnosis is chiefly based on characteristic clinical features and immunohistochemistry. We present a case of Cystadenoma arising from the minor salivary gland in retromolar area of a 44 year old female patient with a special emphasis on the immunohistochemistry to rule out the metastatic follicular carcinoma of thyroid.
Benign, Minor salivary gland tumor, Immunohistochemistry
Case Report
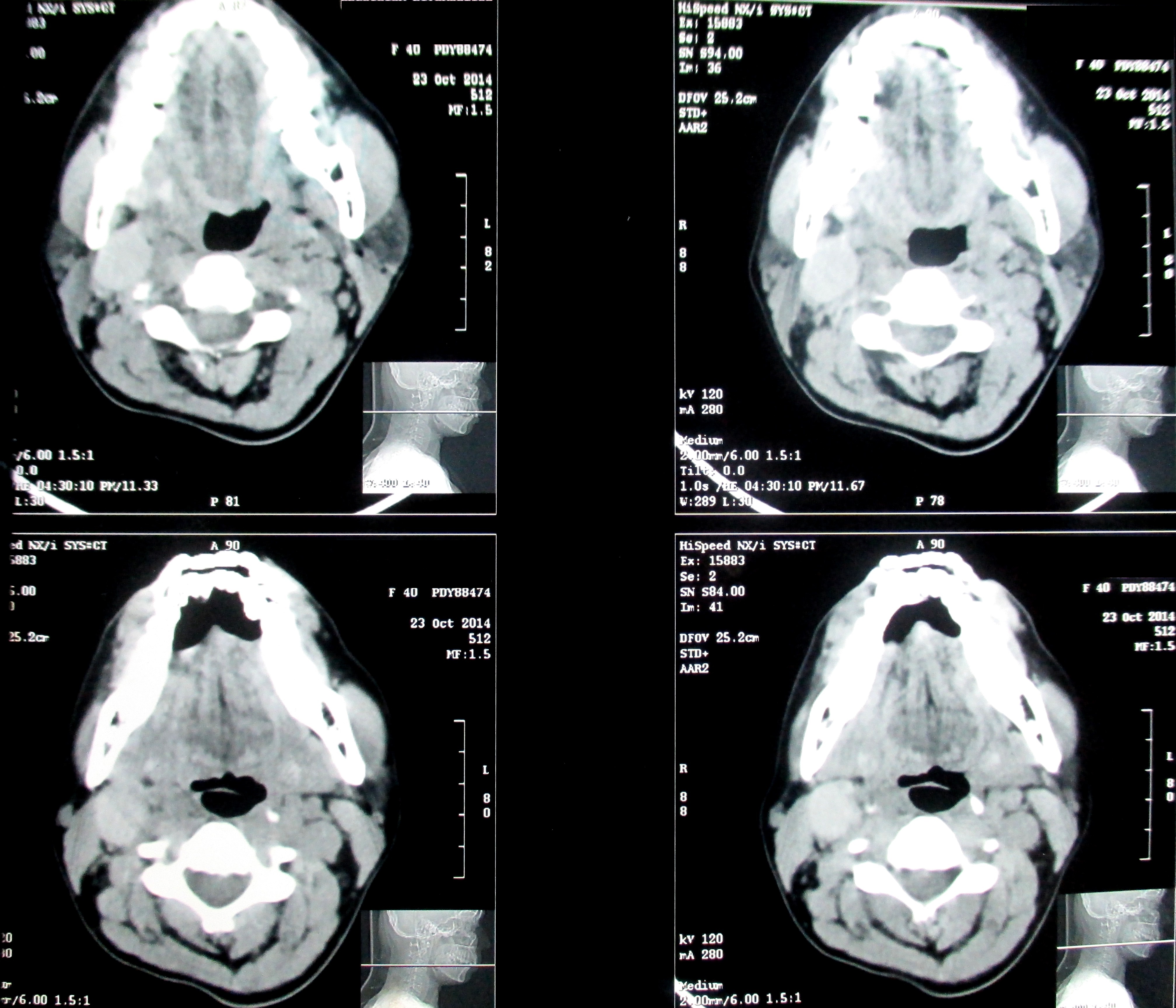
A 40 year old female patient reported with swelling in lower right molar region for past 15 years and pain since two months and no contributing medical or family history [Table/Fig-1]. Patient had the swelling for last 15 years but was asymptomatic and it was persistent in size throughout these years, except for a rare instance where stabbing type of pain was present. However, for the past two months there was an increase in the size of lesion. Clinical examination revealed a well-defined dome shaped mass of approximately 3cmX4cm, extending anteriorly from the distal aspect of tooth 47 to the retromolar region posteriorly, firm in consistency, color same as adjacent mucosa, borders well defined and tender on palpation. Single right submandibular lymph node was palpable approximate size 3cmX1.5cm, mobile and tender. CT scan revealed a well encapsulated hyper dense lesion of 60-70HU in the right submandibular region separated from right submandibular gland close to common carotid artery bifurcation [Table/Fig-2]. A provisional clinical diagnosis was made as pleomorphic adenoma. Incisional biopsy was done and reported as “reactive chronic inflammatory reaction accompanied by few giant cells and cholesterol cleft”.
Intraoral photograph showing dome shaped swelling in the retro molar area.

CT scan revealed a well encapsulated hyper dense lesion in the right submandibular region close to common carotid artery bifurcation.
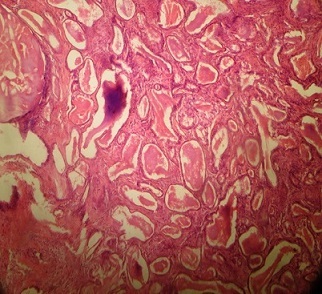
The histological examination showed epithelial and mesenchymal components. Epithelium was keratinized with dense fibrosis of underlying connective tissue but in some focal area there was a band of squamous epithelial proliferation into the connective tissue with eosinophilic content within it, with adjoining areas of chronic inflammatory cell infiltrate associated with foreign body type of giant cells. However the adjacent minor salivary gland showed few dilated duct and inflammatory cell infiltrate [Table/Fig-3,4].
Photomicrograph showing multiple duct like structures with central eosinophilic material (H&E, 100X).
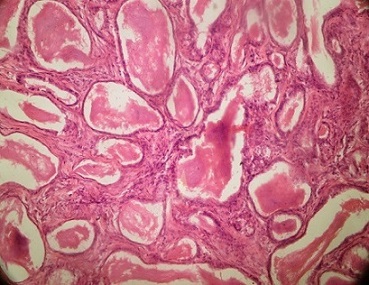
Cystic spaces lined by both columnar and flat epithelium with mucoid material within it (H&E, 400X).
It was planned to perform total excision under general anesthesia with nasotracheal intubation and the procedure was uneventful. The excised specimen was examined thoroughly and was reported as Cystadenoma.
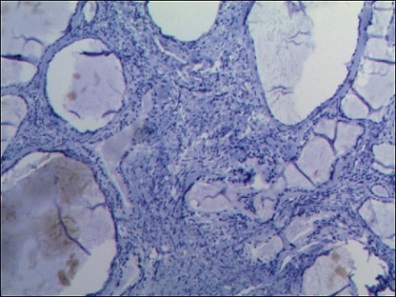
The histological examination showed dilated multicystic areas lined by both columnar and flat epithelium, containing mucoid material within the lumen. In some areas psammoma like calcified bodies were seen in the lumen with adjoining lining epithelium exhibiting squamous metaplasia. These multicystic areas were separated by hyalinized septa. Histopathology of l0esion was suggestive of Cystadenoma associated with sialolith and dilated duct with lining epithelium in periphery. Lumen consisted of a mixture of eosinophilic and dense basophilic material in the central region with lamellar calcified structure. The patient was followed up for four months and there was no evidence of recurrence. The immunohistochemistry for thyroglobulin was done to rule out the metastatic follicular carcinoma of thyroid and it came out negative [Table/Fig-5].
IHC showing negativity for thyroglobulin.
Discussion
Salivary gland tumors are heterogeneous group of lesions of great morphologic variation which accounts for less than 3% of head and neck tumor. Worldwide series shows minor salivary gland neoplasms of less than 25% of salivary gland tumors [1,2]. The most frequent location for this tumor in the oral cavity is hard palate, cheek and posterior region of tongue and it is sometimes also found in the retro molar area [3]. Cystadenoma is a slow, painless, enlarging salivary gland tumor that rarely exceeds 1.5cm in size and most commonly occurs in minor salivary glands. Older patient are affected with female predominance [4]. WHO has defined Cystadenoma as a “tumor containing multiple papillary projections into cystic spaces with and numerous types of lining epithelial cell with close resemblance to Warthin’s tumor without showing aggregates of lymphoid elements” [5]. The diagnosis of cystadenoma is strictly based on histopathology. On histopathological examination multiple cystic spaces of variable size and number often exhibiting intraluminal papillary projection and these cystic spaces are lined by double layer of cells with basally placed cuboidal cells and superficially placed columnar cells. Inflammatory infiltrate and squamous metaplasia in some of the areas was also reported. The histopathological pattern in our case was similar to this feature but to rule out any type of metastasis from thyroid gland pathology immunohistochemistry with thyroglobulin was done which was negative [6]. Surgical excision is the indicated treatment but lesion recurs if it is not removed appropriately [7].
Because of complexity and histomorphological variation of salivary gland tumor, Cystadenoma should be differentiated from Warthin’s tumor, Intraductal papilloma, Canalicular adenoma, Cyst adenocarcinoma and Low grade mucoepidermoid carcinoma.
Although Warthin’s tumor may be regarded as exclusively a parotid gland tumor, the presence of lymphoid aggregate sub-epithelially and double row of epithelium with inner cuboidal and outer tall columnar cells histopathologically confirms its nature. These features were not present in our case [8].
In Intraductal papilloma only single cystic space with papillary projections are present but in our case multiple cystic spaces lined by double layer of cells were observed [8].
Canalicular adenoma consists of large cystic space with papillary proliferation but the epithelium is of single layer of either cuboidal or columnar, with hypovascular loosely arranged connective tissue stroma [8].
Cystadenocarcinoma, Polymorphous low grade adenocarcinoma and papillary cystic variant of Acinic cell carcinoma were eliminated based on features of malignancy i.e., pattern of growth in focal area, mode of invasion, cellular atypical features, destruction of glandular lobe architecture and infiltration into underlying deeper tissue. None of these features were observed in our case.
In most cases of cystadenoma the most preferred treatment is surgical excision but recurrence is common if not excised fully and hence, follow up is necessary [8].
Conclusion
Cystadenoma is a rare benign salivary gland epithelial neoplasm that occurs most commonly on the hard palate, cheek and rarely in the retro molar region. The aim of this study was to document the rarely reported Cystadenoma arising from minor salivary gland in retro molar region. Regular follow up of the patient is necessary for early identification of the recurrence, which may occur due to incomplete excision.
[1]. Rai S, Rana AS, Gupta V, Jain G, Prabhat M, Mucinous cystadenoma: A rare entityDent Res J 2013 10:685-88. [Google Scholar]
[2]. Lingaraj SH, Munde AD, Biradar S, Shaikh SS, Papillary cystadenoma of parotid gland- an unusual entityPravara Med Rev 2014 6:21-23. [Google Scholar]
[3]. Tjioe KC, de Lima HG, Thompson LD, Lara VS, Damante JH, de Oliveira-Santos C, Papillary cystadenoma of minor salivary glands: report of 11 cases and review of the English literatureHead Neck Pathol 2015 9(3):354-59. [Google Scholar]
[4]. Shafer Hine Levy Tumor of salivary glandIn: Shafer’s textbook of oral pathology. Rajendran R, Sivapathasundharam B, editors 2012 7th editionElsevier health sciences:234 [Google Scholar]
[5]. Ananthaneni A, Kashyap B, Ram Prasad VVS, Srinivas V, Cystadenoma: A perplexing entity with subtle literature. DrNTR Uni Health Sci 2012 3:1-4. [Google Scholar]
[6]. Takahashi Y, Kawano K, Yanagisawa S, Yokoyama S, Cystadenoma arising from retromolar region: a case reportOral Science International 2008 5:61-64. [Google Scholar]
[7]. Ribeiro DA, Sales Nogueira Costa MR, Francisco de Assis G, Papillary cystadenoma of the minor salivary gland of the lower lipDermatology Online Journal 2015 1:1-2. [Google Scholar]
[8]. Santhos JND, Conceicao Barros A, Sarmento VA, Silva Gurgel CA, Ferriera de souza V, Cystadenoma: a rare tumor originated in minor salivary glandJ Bras Patol Med Lab 2008 44:205-08. [Google Scholar]