O’Brien’s Granuloma- A Case Report
Pratik Mukesh Thacker1, Kashinath Nayak2, Flora Dorothy Lobo3, Pavithra Govindasamy4
1 Resident, Department of Dermatology, Kasturba Medical College, Mangaluru, Karnataka, India.
2 Associate Professor, Department of Dermatology, Kasturba Medical College, Mangaluru, Karnataka, India.
3 Professor, Department of Pathology, Kasturba Medical College, Mangaluru, Karnataka, India.
4 Resident, Department of Dermatology, Kasturba Medical College, Mangaluru, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kashinath Nayak, Associate Professor, Department of Dermatology, Kasturba Medical College, Mangaluru-575001, Karnataka, India.
E-mail: kashi.nayak@manipal.edu
Actinic granuloma is a self-limiting chronic disorder with elastolytic granulomas, mainly of the sun exposed skin and unknown pathogenesis. We report a case of a middle aged woman with multiple annular erythematous lesions. Histopathology revealed degenerated elastic fibres with histiocyte aggregates surrounded by multiple giant cells suggestive of elastolytic granulomas. She also had associated dyslipidemia and hypothyroidism. Actinic granuloma is relatively rare in the Indian population and needs to be differentiated from conditions like sarcoidosis and granuloma annulare.
Actinic, Annular plaques, Elastolysis
Case Report
A 46-year-old South Indian lady complained of asymptomatic ring-like raised lesions over upper limbs and upper back since 2 years. The lesions started as small papular eruptions which slowly enlarged to form annular plaques. There was history of partial improvement with an unknown topical medication about 18 months back followed by recurrence in 6 months. The patient was a known hypothyroid on thyroxine. There were no other associated complaints or co-morbidities.
On examination, erythematous raised annular plaques ranging from 0.5 to 2.5cm over sun exposed areas of bilateral upper limbs and upper back were seen. Lesions were non-scaly, non-oozy and non-tender [Table/Fig-1,2 and 3]. There were no other significant findings on physical examination. Laboratory investigations revealed an elevated Erythrocyte Sedimentation Rate (ESR) (43mm/hr), dyslipidemia (total cholesterol 296mg/dl) and an elevated thyroid stimulating hormone (20.66μIU/ml). Rest of the routine investigations were normal. Based on these findings, clinical differential diagnoses of granuloma annulare, actinic granuloma and sarcoidosis were made.


Annular lesions on upper back.

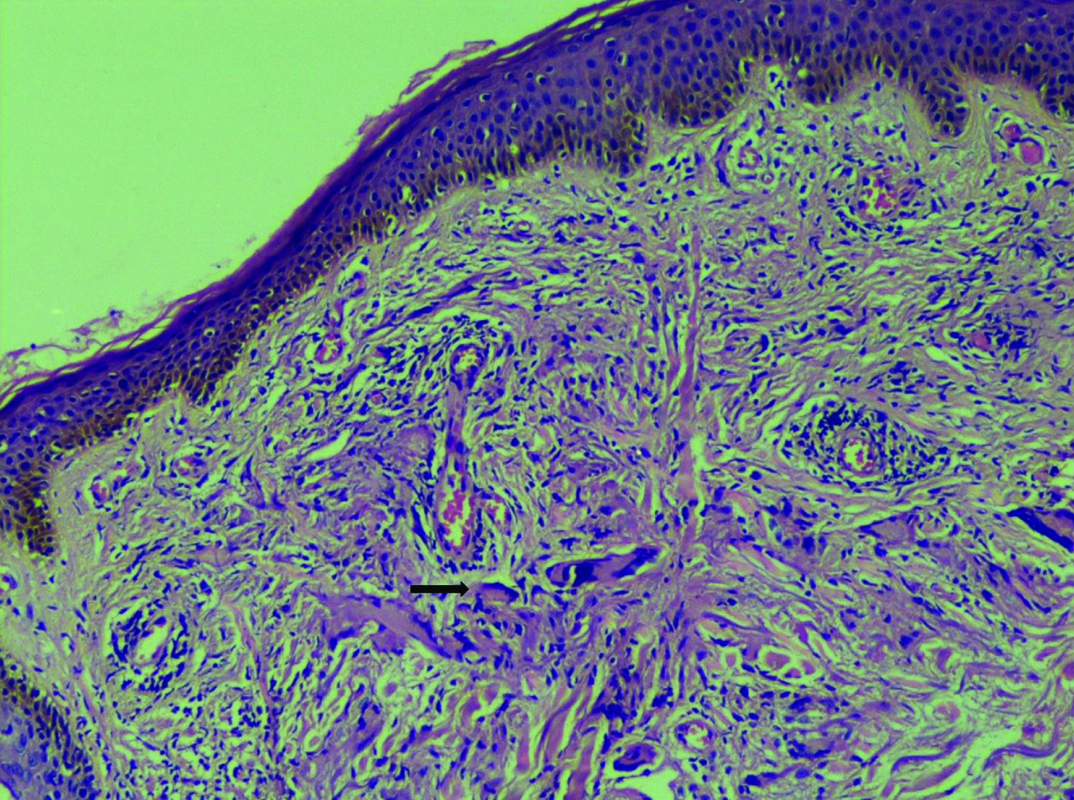
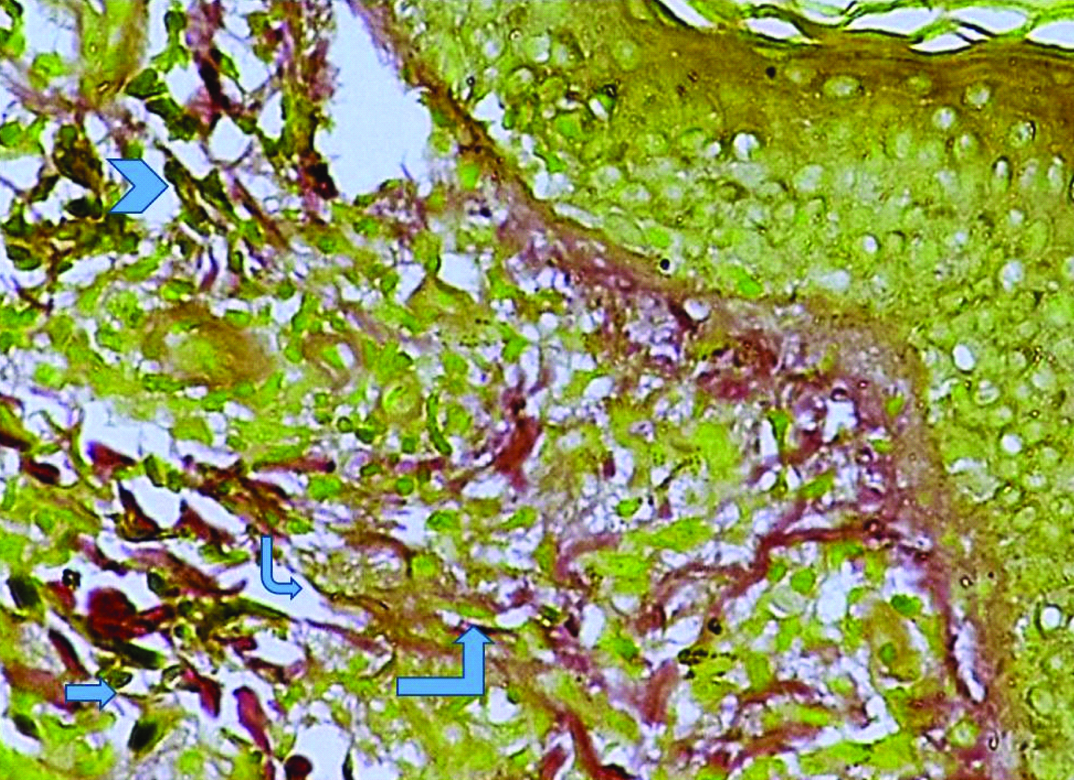
Histopathological examination with H & E stain revealed epidermis with focally thinned out areas upper and middle dermis with histiocytic aggregates surrounded by multiple giant cells. Focal areas of chronic inflammatory cells were seen [Table/Fig-4]. PAS stain was negative for fungal elements. Verhoeff van Gieson stain showed some degenerate elastic fibres [Table/Fig-5].
Thinned epidermis with degenerated elastic fibres with histiocyte aggregates surrounded by multiple giant cells. [H & E stain. x100].
Showing some degenerated elastic fibres (blue arrow). [Verhoef van Gieson stain x400].
Since our patient could not afford acitretin, she was advised strict sun protection. She was counselled regarding clothing which was sun protective. Patient was also started on Dapsone 100mg once a day, but lost to follow-up after the initial visit.
Discussion
Actinic granuloma, also known as annular elastolytic giant cell granuloma was first described by O’Brien in 1975 [1]. It is characterised by annular inflammatory lesions over sun-exposed areas with histopathology showing a giant cell dermal infiltrate, elastolysis and elastophagocytosis. Till date, there is a controversy whether it is a distinct entity or a variant of granuloma annulare. However, most authors are of the opinion that it is a distinct entity due to its characteristic histopathological findings [2]. Its aetiology and associations are poorly understood, hence it is important to report more cases in literature.
Actinic granuloma affects mainly sun exposed areas in adults without any sex predilection [3]. It is seen more commonly in fair skinned individuals and those living in sunny countries. Lesions typically start as small erythematous papules and progress insidiously to form erythematous annular plaques. The borders are usually serpiginous, approximately 3mm in diameter and pearly to reddish-brown. Centre of the lesions may be atrophic or depigmented. Number of lesions is highly variable from single to multiple [1,4,5]. There have been reports of involvement of sun covered areas as well [6,7]. Although lesions are mostly asymptomatic, mild erythematic and irritation may be seen on sun exposure. It has a slow but self-limiting course and may take up to 10 years to resolve.
According to O’Brien’s actinic hypothesis, solar damage to the elastic fibres is the initial event in pathogenesis, which provides an antigenic trigger for a CD4 mediated immune granulomatous reaction [1,8,9]. Due to reports of lesions on covered areas of the skin and no definite proof of role of sunlight in its causation, some authors preferred the descriptive term giant cell elastolytic granuloma over actinic granuloma [10]. However, the actinic hypothesis was further strengthened by finding of lesions in affected skin of vitiligo patients [11].
The histopathology of actinic granuloma is characterised by three zones- the central zone, an elevated border and the skin peripheral to the ring [1,4,5]. The central zone shows near total to total absence of elastic fibres whereas the peripheral zone shows increased amount of elastotic material best appreciated by elastic stains like Verhoeff-van Gieson stain. The raised border shows granulomatous infiltrate with histiocytes either arranged interstitially between collagen bundles or less commonly in a palisading fashion. Multinucleated histiocytes may be seen with elastotic fibres adjacent to or within the giant cells. Mucin is absent.
Several authors have claimed actinic granuloma as a variant of granuloma annulare and not a separate entity [12]. Although some amount of elastolysis is seen in granuloma annulare, complete loss of elastic tissue in the central zone of actinic granuloma separates the two conditions [4]. Other differentiating features differentiating the two include the presence of larger, more abundant giant cells and absence of mucin in actinic granuloma [2]. Other important differential diagnosis includes necrobiosis lipoidica which differs by absence of elastolysis, presence of collagen degradation and involvement of lower dermis and subcutis rather than upper and mid dermis.
Certain conditions that were initially believed to be separate conditions, now considered forms of actinic granuloma are atypical necrobiosis lipoidica of the face and scalp [13], Meischer’s granuloma of the face [5], and granuloma multiforme [4]. A few unproven associations have been proposed; these include diabetes mellitus, polymyalgia rheumatica, relapsing polychondritis, pseudoxanthoma elasticum and vitiligo. Our case had hypothyroidism and dyslipidemia as comorbidities; none of which are known associations of actinic granuloma. Actinic granulomas in presence of dyslipidemia have been previously reported [14]. Also, their response to Dapsone has been reported in literature which formed the basis for us to treat our patient with Dapsone, however its response could not be assessed as the patient was lost to follow-up [15]. Due to lack of clarity of its associations and relatively uncommonn occurance of this condition in general population, we feel this case is worth reporting.
Conclusion
Annular elastolytic granuloma(O Brien’s Granuloma), is not a frequently encountered entity in Indian scenario. So there is a high chance of missing such cases, if a thorough clinical and histopathological evaluation is not done.
[1]. O’Brien JP, Actinic granuloma. An annular connective tissue disorder affecting sun- and heat-damaged (elastotic) skinArch Dermatol 1975 111(4):460-66. [Google Scholar]
[2]. Al-Hoqail IA, Al-Ghamdi AM, Martinka M, Crawford RI, Actinic granuloma is a unique and distinct entity: a comparative study with granuloma annulareAm J Dermatopathol 2002 24(3):209-12. [Google Scholar]
[3]. Doulaveri G, Tsagroni E, Giannadaki M, Bosemberg E, Limas C, Potouridou I, Annular elastolytic giant cell granuloma in a 70-year-old womanInt J Dermatol 2003 42(4):290-91. [Google Scholar]
[4]. Steffen C, Actinic granuloma (O’Brien)J Cutan Pathol 1988 15(2):66-74. [Google Scholar]
[5]. Mehregan AH, Altman J, Miescher’s granuloma of the face. A variant of the necrobiosis lipoidica-granuloma annulare spectrumArch Dermatol 1973 107(1):62-64. [Google Scholar]
[6]. Sina B, Wood C, Rudo K, Generalized elastophagocytic granulomaCutis 1992 49(5):355-57. [Google Scholar]
[7]. Ozkaya-Bayazit E, Büyükbabani N, Baykal C, Oztürk A, Okçu M, Soyer HP, Annular elastolytic giant cell granuloma: sparing of a burn scar and successful treatment with chloroquineBr J Dermatol 1999 140(3):525-30. [Google Scholar]
[8]. Lau H, Reid BJ, Weedon D, Actinic granuloma in association with giant cell arteritis: are both caused by sunlight?Pathology 1997 29(3):260-62. [Google Scholar]
[9]. Stein JA, Fangman B, Strober B, Actinic granulomaDermatol Online J 2007 13(1) [Google Scholar]
[10]. Hanke CW, Bailin PL, Roenigk HH, Annular elastolytic giant cell granuloma. A clinicopathologic study of five cases and a review of similar entitiesJ Am Acad Dermatol 1979 1(5):413-21. [Google Scholar]
[11]. de Paz NM, Rodríguez-Martín M, Bustínduy MG, Martín-Herrera A, Noda-Cabrera A, Strict Anatomical Colocalization of Vitiligo and Elastolytic GranulomasCase Rep Dermatol 2010 2(1):13-17. [Google Scholar]
[12]. Ragaz A, Ackerman AB, Is actinic granuloma a specific condition?Am J Dermatopathol 1979 1(1):43-50. [Google Scholar]
[13]. Lynch M, Callagy G, Mahon S, Murphy LA, Arcuate plaques of the face and scalpClinical and Experimental Dermatology 2010 35(7):799-800. [Google Scholar]
[14]. Coutinho ID, Ramos LI, Brites MM, Tellechea O, O’Brien actinic granuloma: A case report and brief review of literatureIndian J Dermatol 2015 60:391-93. [Google Scholar]
[15]. Igawa K, Maruyama R, Katayama I, Nishioka K, Anti-Oxidative Therapy with Oral Dapsone Improved HCV Antibody Positive Annular Elastolytic Giant Cell GranulomaThe Journal of Dermatology 1997 24(5):328-31. [Google Scholar]