Treatment Emergent Agranulocytosis with Skin and Gingival Lesions in a Chronic Lymphocytic Leukemia Patient: A Case Report
Ramesh Amirisetty1, Varun Zade2, Meenakshi Boddun3, Rolly Gupta4, Micky Kumari5, Hema Suryawanshi6
1 Professor, Department of Periodontology, Chhattisgarh Dental College and Research Institute, Rajnandgaon, Chhattisgarh, India.
2 Lecturer, Department of Periodontology, Chhattisgarh Dental College and Research Institute, Rajnandgaon, Chhattisgarh, India.
3 Lecturer, Department of Periodontology, Chhattisgarh Dental College and Research Institute, Rajnandgaon, Chhattisgarh, India.
4 Reader, Department of Oral Pathology and Microbiology, Chhattisgarh Dental College and Research Institute, Rajnandgaon, Chhattisgarh, India.
5 Postgraduate Student, Department of Periodontology, Chhattisgarh Dental College and Research Institute, Rajnandgaon, Chhattisgarh, India.
6 Professor and Head, Department of Oral Pathology and Microbiology, Chhattisgarh Dental College and Research Institute, Rajnandgaon, Chhattisgarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ramesh Amirisetty, Chhattisgarh Dental College and Research Institute, Sundara, Rajnandgaon-491441, Chhattisgarh, India.
E-mail: rameshperio@icloud.com
Chronic Lymphocytic Leukaemia (CLL) is a monoclonal lymphoid malignancy characterized by progressive accumulation of small, mature but functionally incompetent neoplastic lymphocytes in the peripheral blood, bone marrow and lymphoid organs. Patients present a variable course and may not require early intervention unlike other malignancies. Patients with rapidly deteriorating blood counts, and organomegaly need treatment. Alkylating agent live Bendamustine combined with Rituximab, anti-CD 20 monoclonal antibody have shown promising results in such patients. Anaemia, neutropenia and thrombocytopenia have been reported as treatment emergent events with this combination therapy. Neutrophils are the major innate defense and their depletion can result in a wide range of opportunistic infections. This case report discusess the oral and dermal lesions which emerged with the Rituximab and Bendamustine combination therapy in a patient with CLL and their management.
Bendamustine, Gingival necrosis, Neutropenia, Rituximab
Case Report
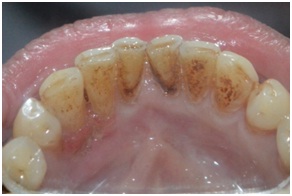
A 51-year-old male was referred to the Department of Periodontics with unusual discolored gingiva in the left lower front teeth region since four days. The lesion developed as a pinpoint size and grew rapidly and there was discomfort and mild pain associated with it. On extra-oral examination there was no gross facial asymmetry and the lymph nodes were palpable. Papulomacular rashes were observed on the forearms and palms. Intra-oral examination revealed diffuse gingival involvement on labial and lingual aspects of tooth #22, 23 and 24 around 25mmx 8mm [Table/Fig-1,2]. Gingiva was pale and soft in consistency with good scalloped contours and pyramidal papilla with a pseudo membranous slough. The lesion was clearly demarcated from the uninvolved mucosal tissue, and no fetid odour was appreciated. The lesion was attached to the underlying bone in the interdental papilla of tooth #22 and 23. Medical history revealed that the patient had fever and vomiting along with skin manifestations three days before he noticed this gingival lesion for which he was admitted in the hospital and given intravenous antibiotics. The skin lesions were treated with DERMAL-K, a herbal clarifying skin cream, by the physician. Six months earlier he went to the physician with complaint of fever, weakness, swellings in the neck and sudden weight loss. CD45, CD5, CD20, CD23, CD38 and IgM were tested positive. Trisomy 12 was negative. Deletion of 17p13 was positive and patient was diagnosed as stage 1 Chronic Lymphocytic Leukaemia (CLL). Patient underwent five cycles of chemotherapy with combination regimen which consisted of Bendamustine and Rituximab. Each cycle consisted of Inj. Ikdar (Rituximab) 600μg on day 1, Inj. Bendamustine 200μg on day 1 and 100μg on day 2, Inj. Pegasta (Pegfilgrastim) 6μgm subcutaneous on day 3. Patient’s blood picture at various cycles of chemotherapy and at the time of patient’s dental visit is outlined in [Table/Fig-3] and at evaluation visits after treatment is outlined in [Table/Fig-4]. The blood reports showed marked depletion of neutrophils one week before the visit. Based on the history, clinical examination and the blood reports a provisional diagnosis of neutropenia associated acute gingival necrosis was made.
Diffuse gingival involvement of the lesion in tooth #22, 23 and 24- labial side.

Diffuse gingival involvement of the lesion in tooth #22, 23 and 24-lingual side.

Complete blood picture at various chemotherapy cycles and at dental visit. (0) day represents dental visit and (–) values represent the before days of the dental visit.
| Date | Day | Hb(gm %) | WBC | Differential Count(N*L†,E‡,M§, B||) | Platelets |
|---|
| 06.04.2015(1st cycle) | 0 day (-164) | 9.6 | 69000 | 09,88,2,1,0 | 174000 |
| 20.04.2015 | 15th day (-149) | 7.4 | 14500 | 24,73,2,1,0 | 160000 |
| 03.05.2015(2nd cycle) | 30th day (-134) | 9.0 | 7300 | 25,70,3,2,0 | 151000 |
| 20.05.2015 | 45th day (-119) | 9.2 | 5200 | 53,44,2,1,0 | 130000 |
| 03.06.2015(3rd cycle) | 60th day (-104) | 8.7 | 4500 | 39,58,2,1,0 | 150000 |
| 04.07.2015(4th cycle) | 90th day (-74) | 11.2 | 3600 | 39,55,6,0,0 | 130000 |
| 03.08.2015(5th cycle) | 120th day (-44) | 11.1 | 3800 | 22,70,3,5,0 | 126000 |
| 10.09.2015 | 156th day (-8) | 7 | 4900 | 03,95,1,1,0 | 131000 |
| 18.09.2015 | 164th day (0) | 9.2 | 5400 | 05,93,1,1,0 | 153000 |
Complete blood picture at dental visit and at evaluation visits. (0) day represents dental visit and (+) values represent the after days of the dental visit.
| Date | Day | Hb(gm %) | WBC | Differential Count(N*L†,E‡,M§, B||) | Platelets |
|---|
| 18.09.2015 | 164th day (0) | 9 | 5400 | 05,93,1,1,0 | 153000 |
| 22.09.2015 | 170th day (+4) | 9.4 | 7000 | 40,56,2,2,0 | 318000 |
| 2.01.2016 | 280th day(+114) | 11.5 | 13000 | 18,75,4,3,0 | 166000 |
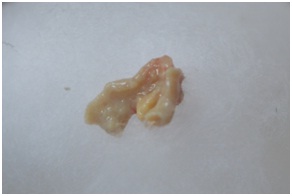
Blood investigations were advised to rule out thrombocytopenia for the removal of the necrotic tissue as an emergency management. Topical anesthesia was given on the affected gingiva and the involved tissue [Table/Fig-5] was removed completely using non-toothed Adsons forceps and sent for histopathological examination. The area was gently swabbed with cotton pellets moistened by 3% hydrogen peroxide to remove the membrane and unattached debris. Scaling and root planning at the local site was done using hand instruments. The patient was treated with a gel containing Metronidazole 1% w/w and Chlorhexidine 0.25%w/w/1g application at the affected site twice a day for one week.
Tissue which was removed as one unit.
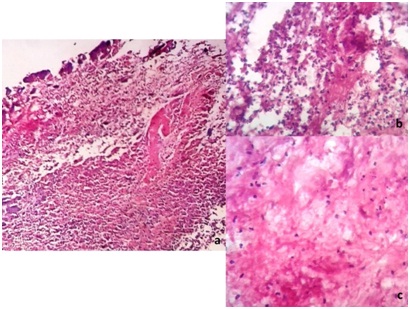
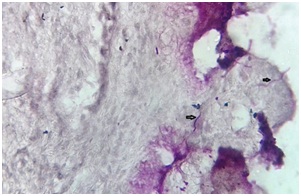
Microscopically H&E stained tissue section under x100 magnifications [Table/Fig-6a] reveals necrotic slough and underlying connective tissue stroma comprising of loose and haphazardly arranged collagen fibers, dense inflammatory infiltrate, blood vessels and extravasated red blood cells. At x400 magnification in [Table/Fig-6b,c] the histological section shows connective tissue with fibroblasts, neutrophils, plasma cells and atypical lymphocytes. At x400 magnification PAS stained section revealed Candidal hyphae in the loose connective tissue stroma [Table/Fig-7]. Based on the histopathological findings and presence of a pseudomebranous slough which could be removed easily leaving an erythematous mucosa without associated fetid odour and the patient did not have severe pain associated with the lesion a final diagnosis of Acute Pseudomembranous Candidiasis associated with Neutropenia was made. On 3rd day the patient was recalled and the oral gel application was substituted with a clotrimazole 1% gel application at the affected site four times in a day for seven days.
(a) At x100 magnifications the histological section reveals necrotic slough and underlying connective tissue stroma comprising of loose and haphazardly arranged collagen fibers, dense inflammatory infiltrate, blood vessels and extravasated red blood cells. (b,c): At x400 magnification the section shows connective tissue with fibroblasts, neutrophils, plasma cells and atypical lymphocytes.
At x400 magnification PAS stained section revealed Candidal hyphae in the loose connective tissue stroma.
The patient was reviewed four days thereafter and the healing was found uneventful. Patient complained of slight pain over the exposed bone surface [Table/Fig-8,9]. Routine blood investigations were advised at all recall visits. The patient was recalled at one month and three months interval for evaluation. There was a definite improvement in the neutrophil count four days after treatment and after three months [Table/Fig-4].
1st week visit - The lesion site - labial side.

1st week visit - The lesion site - lingual side. Exposed bone could be noticed.

At one month the healing was found satisfactory and the exposed bone was covered by gingival tissue in tooth # 22 and 23 [Table/Fig-10,11]. There was improvement in the position of the gingiva. At three months visit there was complete resolution of the exposed bone and no symptoms of pain and discomfort in the gingiva while eating [Table/Fig-12,13]. The gingiva was stable with no signs of recurrence. There was a slight improvement in the gingival position at 3rd month visit than the first month visit. The skin lesions on the forearms also showed good improvement from first dental visit [Table/Fig-14a] and at one month review visit [Table/Fig-14b]. The lesions on palms resolved completely as evident in [Table/Fig-15a] (first visit), [Table/Fig-15b] (one month) and [Table/Fig-15c] (3 months visit).
At one month visit-The lesion site- Labial side.

At one month visit - The lesion site - lingual side.
At one month visit - The lesion site - labial side.

At one month visit-The lesion site - lingual side.

(a) Skin lesions on the forearms at first dental visit; (b) Skin lesions at one month review

(a) The lesions on palms at first dental visit. (b) At one month visit. (c) At three months visit complete resolution noticed.

Discussion
The clinical course of CLL is variable. Patients who don’t develop symptoms may not require interventional treatment for many years. In these patients observation and periodic evaluation is the management strategy. Few patients have an aggressive course and need chemotherapy. Based on clinical and laboratory features such as presence of lymphocytosis, lymphadenopathy, hepatosplenomegaly, anaemia and thrombocytopenia the decision for treatment initiation is made [1]. In this patient the oncologist decided the need for chemotherapy and combination drug therapy which constituted of Rituximab, Bendamustine and prophylactic Pegfilgrastime.
Rituximab, a monoclonal CD 20 antibody has variable effects on cell cycle progression and cell signaling and causes reduction in the circulating B cell [2]. Bendamustine is an alkylating agent and acts by cytotoxic effects. Bendamustine and Rituximab combination have a synergistic effect against various types of leukaemia [3]. Both Bendamustine and Rituximab have been shown to cause neutropenia when used as a single drug regimen or in combination [4,5]. Pegfilgrastim is a G-CSF agonist which improves the neutrophil count and was administered at each cycle to counteract neutropenia which may occur because of the combination therapy.
Agranulocytosis is evident in this patient after five cycles of chemotherapy. The patient had fever and vomiting initially followed by skin and gingival lesions which are typical signs of agranulocytosis [6]. It can cause severe skin and gingival necrosis and opportunistic infections [7]. In this patient the sloughing and peeling of gingiva till the bone surface on the lingual aspect and the skin lesions led us to a provisional diagnosis of neutropenia associated Acute Gingival Necrosis. We initiated the emergency treatment by removal of necrotic tissue and gave local Metronidazole and Chlorhexidine gel application. The diagnosis was confirmed as the PAS staining showed the presence of hyphae thereby opportunistic candidiasis associated with the necrosis. Microscopic sections of pseudomembranous candidiasis are characterised by extensive white pseudomembranes with desquamated epithelial cells, fibrin, and fungal hyphae. These type of lesions occur on the surface of the labial and buccal mucosa, hard and soft palate, tongue, periodontal tissues, and oropharynx. Erythematous mucosa can be noted after the membrane is scraped. These type of lesions can be diagnosed with relative ease as they account for one third of the oropharyngeal candidiasis. Diagnosis can be confirmed microbiologically either by staining a smear from the affected area or by culturing a swab from an oral rinse. Extremes of age, diabetes mellitus, patients who have HIV/AIDS or leukaemia, those using steroid aerosol inhalers, broad spectrum antibiotics, and psychotropic drugs, and patients who are terminally ill are more susceptible for these opportunistic infections [8]. In the present case there is an associated leukaemia and the patient was given antibiotic therapy three days before the onset of the gingival lesion and this could have predisposed the patient for an opportunistic candidiasis. The lesion was easily peeled off from the surface leaving an erythematous mucosa confirming the diagnosis.
As per the final diagnosis the drugs were substituted with Clotrimazole cream for candidiasis. Candidal infections are mostly superficial occurring on moist mucosal surfaces in individuals with a mild debilitation. Our early intervention might have helped in avoiding a more generalized distribution as per the rapid growth history given by the patient.
Although neutropenia is one of the common adverse events associated with chemotherapy there is no case mentioned in the literature regarding the necrotic gingival lesions and their management. Similar extensive generalized gingival necrosis associated with neutropenia was seen with other drugs like methimazole, an anti thyroid drug and was treated with filgrastim injections with success [9]. The gingival crevice is the main source of leukocytes, and these granulocytes respond to bacterial plaque. In neutropenia, bacterial infections are not contained and rapid progression of the lesions is observed with cellular and connective tissue disintegration, and rampant necrotizing gingival lesions [10].
Extensive agranulocytosis is the most serious side effect of deferiprone, which is routinely used in medicine for the treatment of iron overload in thalassaemia patients. Necrotizing gingivostomatitis, an oral manifestation of agranulocytosis secondary to deferiprone use involving the gingiva and palatal mucosa of a thalassaemia major patient was reported in the literature [11].
In our case we removed the necrotic tissue to establish repair and regeneration. Oral hygiene was reinforced. Four days after the treatment blood picture revealed an improvement in the neutrophil count. At three months visit the gingival condition was stable and the blood examination revealed good neutrophil counts. The patient was further referred to the oncologist for further chemotherapy and management.
Conclusion
Chemotherapy in CLL patients can lead to neutropenia which can predispose to opportunistic infections. Careful history taking and examination is essential for proper diagnosis. Targeting the right aetiological factors play a major role in management of such cases.
[1]. Pinilla-Ibarz J, McQuary A, Chronic lymphocytic leukaemia: putting new treatment options into perspectiveCancer Control 2010 17(2suppl):4-15.quiz 16 [Google Scholar]
[2]. Reff ME, Carner K, Chambers KS, Depletion of B cells in vivo by a chimaeric mouse human monoclonal antibody to CD 20Blood 1994 83:435-45. [Google Scholar]
[3]. Rummel MJ, Bendamustine in chronic lymphocytic leukaemia and refractory lymphomaSemin Hematol 2008 45(3 Suppl 2):S7-10. [Google Scholar]
[4]. Kouroukis CT, Crump M, MacDonald D, Larouche JF, Stewart DA, Johnson J, An open-label expanded-access trial of bendamustine in patients with rituximab-refractory indolent non-Hodgkin lymphoma or previously untreated chronic lymphocytic leukaemia: BEND-ACTCurr Oncol 2015 22(4):260-71. [Google Scholar]
[5]. Dunleavy K, Tay K, Wilson WH, Rituximab-associated neutropeniaSeminars in hematology 2010 47(2)WB saunders:180-86. [Google Scholar]
[6]. Maciejewski JP, Tiu RV, Acquired disorders of red cell, white cell, and platelet production in Hoffman R, Benz EJ Jr, Silberstein LE, et alHematology: Basic Principles and Practice 2012 6th edPhiladelphia, PAElsevier Saunders [Google Scholar]
[7]. Ohishi M, Oobu K, Miyanoshita Y, Yamaguchi K, Acute gingival necrosis caused by drug-induced agranulocytosisOral Surg Oral Med Oral Pathol 1988 66(2):194-96. [Google Scholar]
[8]. Akpan A, Morgan R, Oral candidiasisPostgrad Med J 2002 78(922):455-59. [Google Scholar]
[9]. Kim EC, Park JB, Hong JY, Kang KL, Extensive gingival necrosis and sequestration of the alveolar bone caused by methimazole-induced neutropenia and three-year follow-upJ Periodontal Implant Sci 2015 45(2):76-80. [Google Scholar]
[10]. Miller DR, Lamster IB, Chasens AI, Role of the polymorphonuclear leukocyte in periodontal health and diseaseJ Clin Periodontol 1984 11:1-15. [Google Scholar]
[11]. Tewari S, Tewari S, Sharma RK, Abrol P, Sen R, Necrotizing stomatitis: A possible periodontal manifestation of deferiprone-induced agranulocytosisOral Surg Oral Med Oral Pathol Oral Radiol Endod 2009 108(4):e13-19. [Google Scholar]