A Large Pregnancy Tumor of Tongue – A Case Report
U. Arunmozhi1, R. Shanmuga Priya2, R. Kadhiresan3, Govindarajan Sujatha4, Shaik M Shamsudeen-SS5
1 Professor, Department of Periodontics, Sri Venkateshwara Dental College and Hospital, Chennai, Tamil Nadu, India.
2 Reader, Department of Periodontics, Sri Venkateshwara Dental College and Hospital, Chennai, Tamil Nadu, India.
3 Reader, Department of Periodontics, Sri Venkateshwara Dental College and Hospital, Chennai, Tamil Nadu, India.
4 Reader, Department of Oral and Maxillofacial Pathology, Sri Venkateshwara Dental College and Hospital, Chennai, Tamil Nadu, India.
5 Senior Lecturer, Department of Oral and Maxillofacial Pathology, Sri Venkateshwara Dental College and Hospital, Chennai, Tamil Nadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Govindarajan Sujatha, Reader, Department of Oral Pathology, Sri Venkateshwara Dental College and Hospital, Thalambur, Chennai– 600130, Tamil Nadu, India.
E-mail: gsuja@rediffmail.com
Pyogenic granuloma is a tissue overgrowth which commonly develops as a response to irritation or trauma which is usually localized. Though gingiva is said to be the common site, it also can occur on lip, tongue and buccal mucosa. Pathogenesis is unclear but trauma, infection and hormonal imbalance are attributed as reasons for occurrence. Histologically this reactive lesion is filled with immature fibroblastic connective tissue, profilerative blood vessels and inflammatory cells. This article presents a case of a large pyogenic granuloma of the tongue which is a rare site for this tumor in a 27 year old woman.
Irritation, Localized growth, Pyogenic granuloma, Trauma
Case Report
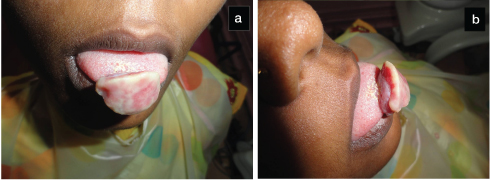
A 27-year-old female reported to a private clinic with a large painless swelling on the dorsal surface of tip of tongue for the past 14 months. She was unable to close her mouth due to the growth which was first noticed as a small growth 14 months back when she was two months pregnant. The swelling had increased to the present size in the due course and her family persuaded her to wait for treatment till her delivery. She was not very clear about any history of trauma. Her oral hygiene was poor. On intra-oral inspection the growth measured about 3 x 3cm in length and breadth, on palpation it was firm in consistency and pedunculated. [Table/Fig-1,2]. The surface did not show any ulceration and appeared pale in colour. History did not reveal any details of regression in size of tumor following her delivery. A provisional diagnosis of fibroma was given and the patient was advised for complete surgical removal. The patient had postponed removal fearing complications during pregnancy though she had difficulty in closing her mouth. She readily agreed for surgical removal.
Clinical photograph; (a) Front view, (b) Profile view.
Excised specimen in formalin.

Routine hemogram was found to be normal and a provisional diagnosis of fibroma was made considering the clinical appearance though the site appeared to be unusual. The differential diagnosis included pyogenic granuloma, peripheral ossifying fibroma, peripheral giant cell granuloma and hemangioma. Following oral prophylaxis, an excisional biopsy was carried out under local anaesthesia using a scalpel and blade and sutures were placed. The excised tissue was sent for histoplathological examination [Table/Fig-3]. The patient was recalled after one week for removal of sutures and healing was uneventful. The patient is under regular follow-up and till date (nine months) no recurrence has been reported.
Connective tissue stroma with numerous budding capillaries.
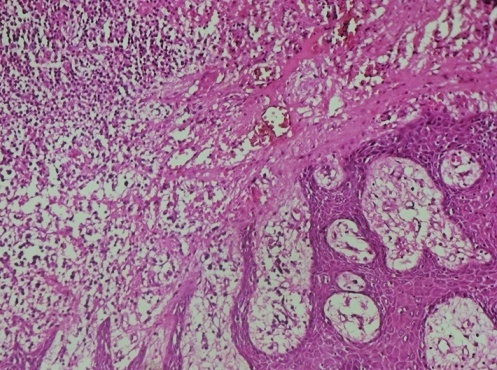
Histopathological examination revealed parakeratinsed stratified squamous epithelium which appeared hyperplastic. The connective tissue revealed a delicate fibrillar stroma with numerous budding capillaries and interspersed fibroblasts, collagen fibres and chronic inflammatory cells chiefly lymphocytes. Deeper sections showed a more fibrous picture with bundles of collagen fibres and reduced vascularity. The diagnosis of pyogenic granuloma was histologically confirmed.
Discussion
Pyogenic granuloma is considered as a neoplastic growth of the oral cavity [1]. This tumor like lesion includes 3.8 to 7% of all the biopsies of the oral cavity lesions [2]. This proliferative cellular and vascular tumor is thought to arise as a result of chronic local irritation, drug reaction, hormonal variations and response to grafts [3]. The gingiva being the commonest site in intra-oral granuloma, it can also be seen on lips, tongue, buccal mucosa, palate and floor of the mouth [4]. Clinically the lesion presents as a pink to reddish lobulated mass which is sessile or pedunculated. This article presents a case of unusually large pyogenic granuloma at an unusual site.
Poncet and Dor were the first to describe pyogenic granuloma in 1897 and called it botryomycosis hominis. Confusion preveals about the present name, which some believe to be given by Crocker in 1903 and Hartzell in 1904 [5,6]. The other names which had been given include Crocker and Hartzell’s disease, granuloma pyogenicum, granuloma pediculatum benignum, benign vascular tumor and granuloma gravidarum [7].
Various aetiological factors such as trauma, chronic irritation, hormones, drugs, eruption of teeth, defective fillings, periodontitis, tooth brush irritation etc., have been put forward in cases where patients reported with these findings [8]. Though, some authors originally believed that the lesion was due to infection, there is no evidence confirming the presence of infectious organisms in large groups [9]. The general agreement is that pyogenic granuloma arises as a result of minor trauma to the tissue which may provide a pathway for microorganism and it is the tissue response to this low virulent organism in the form of proliferating vascular type connective tissue. In our case hormonal imbalance due to pregnancy was believed to be the aetiological factor.
Tissue reaction to any irritant is usually to get stimulated or destructed. If many cells are present in a small volume of tissue and there is a reduced blood flow through the area as in inflammation, the concentration of the stimulating substance will be high and growth will be stimulated. Growth is retarded following maturation of cells and reduced concentration of stimulating substances. In contrast stimulus to vascular endothelial proliferation sustains over a long period of time because of the reduced destruction of cells in pyogenic granuloma [10].
The surge in estrogen and progesterone level in circulating blood during pregnancy exerts proliferative effect on the endothelium [11,12] [Table/Fig-4].
Role of sex hormones in pyogenic granuloma.
| Hormone | Cell and Effect | Mediators |
|---|
| Estrogen | Fibroblast – ProliferationMacrophage – ActivationEndothelial ProliferationKeratinocytes - Proliferation | Fibroblast Growth FactorTransforming Growth Factor Beta 1Nerve Growth FactorVascular Endothelial Growth FactorGranulocyte Macrophage Colony Stimulation Factor |
| Progestrone | Acute Inflammatory Cells – SuppressionChronic Inflammatory Cells –Proliferation | ---------------- |
Though the process of regression of pyogenic granuloma occurring during pregnancy is unclear it may be related to the absence of vascular endothelial growth factor and angiopoietin 2 causing the blood vessels to regress, leading to regression of the tumor [8].
Pyogenic granuloma occurs over a wide range of age from 4.5 yrs to 93 yrs with highest incidence being in second and fifth decade of life [12]. There was a definite female predilection with a female to male ratio of 2:1 and the reason was attributed to the vascular effect of female hormones that occur in women during puberty, pregnancy and menopause. The lesions tend to occur more commonly in the second and third trimester of pregnancy and were referred to as “Pregnancy Tumors” [13]. This coincides with the clinical case which we have reported with the patient being a female in third decade of her life. Though common in second and third trimester our patient gave a history of occurrence during the first trimester. Oral pyogenic granuloma which is a very common gingival tumor, occurs more often in the gingiva accounting for 75% of all pyogenic granulomas followed by lips, tongue and buccal mucosa. Its occurance is more in the maxillary anterior region than posterior and mandibular region [8].
The tumor which is usually sessile or pedunculated appears smooth or as an exophytic mass. The high vascularity of the lesion exhibits lobulated erythematous papaules which when ruptures presents as ulcerations with fibrinous membrane [14]. The color varies from red, reddish purple to pink depending upon the vascularity of the tumor [15]. Minor trauma causes the young tumors to bleed profusely due to vascularity; whereas, older lesions are more collaginised and pink [1]. The size of the tumor varies from few millimeters to several centimeters and is usually slow growing, painless and asymptomatic, but at times it grows rapidly [1,16]. The long duration of our lesion justifies the appearance of it being pale and firm which could be contributed to the collaginisation.
Histopathologically, pyogenic granuloma usually presents with granulation tissue in a delicate fibrillar stroma with inflammatory cells and proliferating capillaries and endothelial cells. Usually the duration of the tumor expresses the extent of vascularity and fibrosis [17]. The Lobular Capillary Haemangioma (LCH type) appears as lobular aggregates of proliferating blood vessels and the non-Lobular Capillary Haemangioma (non – LCH type) shows proliferating blood vessels as granulation tissue [18]. Mature pyogenic granuloma losses its vascularity and becomes more fibrous and resembles an irritation fibroma [14]. Our histopathological picture coincided with that of a long standing lesion. Immunohistochemical studies on pyogenic granuloma shows positivity to both factor VIII and Ulex europaeus. This later shows positivity to both endothelial cells lining large vessels and cellular aggregates with the former showing positivity only for endothelial cells. Increased expression of vascular endothelial growth factor and nitric oxide synthase with low apoptotic rate expression of Bax/Bcl-2 proteins were observed. There was no involvement of human papiloma virus and human herpes virus type. The other enhanced factors include bFGF, Tie – 2, anti- CD34 and vascular morphogenic factors such as angiopoietin-1, angiopoietin-2 [19].
Surgical excision is the treatment of choice for pyogenic granu-loma. Considering the high recurrence, excision involving normal tissue at its periphery with a depth to the periosteum and curettage of the underlying tissue after excision is recommended [20]. The unusual location of the lesion in our case required certain precautions. Tongue being a highly vascular organ, care was taken not to traumatize the major veins. Surgery was performed to the required depth taking into account the presence of nerves and muscles. The recurrence rate of 16% is observed in excised lesions and incomplete excision, failure to remove aetiological factors and trauma are attributed as reasons [21]. Other treatments include Nd;YAG laser, flash lamp pulsed dye laser, cryosurgery, intra-lesional injection of ethanol and sodium tetradecyl sulfate sclerotherapy [8].
Conclusion
Oral pyogenic granuloma is relatively a common lesion in the oral cavity which presents as an overgrowth of tissue. Various aetiological factors are considered for the occurance of this lesion. This paper highlights the unusual presentation of a large lesion in the tongue and the duration of lesion which leads to its size. Correct diagnosis with identification of aetiology and treatment planning along with patient education is essential.
[1]. Nevile BW, Damm DD, Allen CM, Bouquot JE, Oral and Maxillofacial Pathology 2004 2nd EditionW.B.Saunders:444-44. [Google Scholar]
[2]. Avelar RL, Antunes AA, Carvalho RWF, Santos TS, Neto PJO, Andrade ESS, Granuloma piogenico oral: Um estudo epidemiologico de 191 casos 2008 56:131-35. [Google Scholar]
[3]. Pereira CM, De Almeida OP, Correa ME, Souza CA, Barjas-Castro ML, Oral involvement in chronic graft versus host disease: A prospective study of 19 Brazilian patientsGen Dent 2007 55(1):48-51. [Google Scholar]
[4]. Parisi E, Glick PH, Glick M, Recurrent intraoral pyogenic granuloma with satellitosis treated with corticosteroidsOral Dis 2006 12(1):70-72. [Google Scholar]
[5]. Bhaskar SN, Jacoway JR, Pyogenic granuloma – Clinical features, incidence, histology and result of treatment: Report of 242 casesJ Oral Surg 1966 24:391-98. [Google Scholar]
[6]. Angelopoulos AP, Pyogenic granuloma of the oral cavity: Statistical analysis of its clinical featuresJ Oral Surg 1971 29:840-47. [Google Scholar]
[7]. Gomes SR, Shakir QJ, Thaker PV, Tavadia JK, Pyogenic granuloma of the gingival: A misnomer ? – A case report and review of literatureJ Indian Soc Periodontol 2013 17(4):514-19. [Google Scholar]
[8]. Jafarzadeh H, Sanatkhani M, Mohtasham N, Oral pyogenic granuloma: A reviewJ Oral Sci 2006 48:167-75. [Google Scholar]
[9]. Janier M, Infection and angiomatous cutaneous lesionsJ Mal Vasc 1999 24:135-38. [Google Scholar]
[10]. Shafer Hine Levy Shafer’s Textbook of Oral pathology 2006 5th edAmsterdamElsevier Health Sciences:459-61. [Google Scholar]
[11]. Whitataker SB, Bouquot JE, Alimario AE, Whitaker TJ Jr, Identification and semi quantification of estrogen and progesterone receptors in pyogenic granuloma of pregnancyOral Surg Oral Med Oral Pathol 1994 78:755-60. [Google Scholar]
[12]. Kamal R, Dahiya P, Puri A, Oral pyogenic granuloma: Various concepts of etiopathogenesisJ Oral Maxillofac Pathol 2012 16(1):79-82. [Google Scholar]
[13]. Sapp JP, Eversole LR, Wysocki GP, Contemporary oral and maxillofacial pathology 2004 2nd edMissouriMosby:318-19. [Google Scholar]
[14]. Regezi JA, Sciubba JJ, Jordan RC, Oral Pathology: Clinical Pathological Considerations 2003 4th edWb Saunders:115-16. [Google Scholar]
[15]. Mubeen K, Vijayalakshmi KR, Abhishek RP, Oral pyogenic granuloma with mandible involvement: An unusual presentationJ Dent Oral Hyg 2011 3:6-9. [Google Scholar]
[16]. Parisi E, Glick PH, Glick M, Recurrent intraoral pyogenic granuloma with satellitosis treated with corticosteroidsOral Dis 2006 12:70-72. [Google Scholar]
[17]. Muruganandan J, Sivakumar G, Sujatha G, A large pyogenic granuloma developing into a peripheral ossifying fibroma: A case report and discussionI Jou Mul Dent 2011 1:342-46. [Google Scholar]
[18]. Bouquot JE, Nikai H, Lesions of the oral cavity. Diagnostic surgical pathology of the head and neckWB Saunders 2001 :141-233. [Google Scholar]
[19]. Sato H, Takeda Y, Santoh M, Expression of the endothelial receptor tyrosine kinase Tie2 in lobular capillary haemangioma of the oral mucosa: An immunohistochemical studyJ Oral Path Med 2002 31:432-38. [Google Scholar]
[20]. Patil K, Mahima VG, Lahari K, Extragingival pyogenic granulomaIndian J Dent Res 2006 17:199-202. [Google Scholar]
[21]. Taira JW, Hill TL, Everett MA, Lobular capillary haemangioma (pyogenic granuloma) with satellitosisJ Am Acad Dermatol 192 27:297-300. [Google Scholar]