Introduction
Magnetic Resonance Imaging (MRI), being a technique with huge potential, has become the primary diagnostic investigation for many clinical problems. Its application now has been successfully used in dentistry to maximize the diagnostic certainty.
Aim
The present review aims to analyze the applicability, feasibility and efficacy of MRI in the field of dentistry.
Materials and Methods
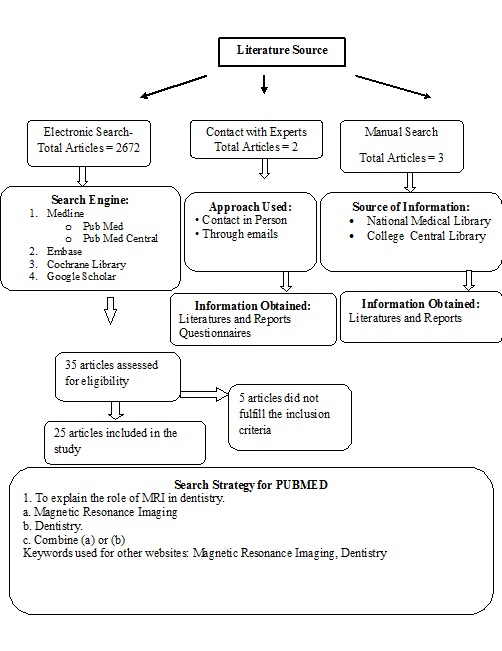
A literature search was performed in main databases like Pub Med Central, Cochrane Library, Embase and Google Scholar from 1970 up to December 2015. The 2672 titles that appeared, 25 fulfilled the criteria and were included in the review. Two articles were hand searched and three articles through e-mail were also included.
Results
The review highlights the increasing role of MRI in dentistry. In the available literature, it was found that T1 and T2 weighted images were the acceptable diagnostic images for detection of dental related diseases.
Conclusion
MRI can be used in diagnosis and treatment planning of implants, jaw lesions, diseases of Temporomandibular Joints (TMJ), orthodontic treatment, endodontic treatment etc., to achieve better prognosis.
Dental Implant, Magnetic Resonance Imaging, Stainless steel, Temporomandibular joint
Introduction
Tooth is one of the hardest substance of human body which comprises mainly of three components such as Enamel, Dentin and Pulp. Dentistry has witnessed tremendous advances in all its branches over the past four decades in diagnosis and treatment planning but dentistry has relied substantially on technological aids [1]. The technological aids such as Computed Tomography (CT), Cone Beam Computed Tomography (CBCT), Magnetic Resonance Imaging (MRI) and Ultrasonography have an important place in modern dentistry.
MRI is a non-invasive method to detect the internal structures, differentiate between soft tissues and hard tissues and certain aspects of functions within the body. The principle behind MRI is the use of non-ionizing radio frequency electromagnetic radiation in the presence of controlled magnetic fields, to obtain high quality cross-sectional images of the body [2].
MRI technique has evolved through the years [Table/Fig-1]. The first nuclear magnetic resonance image was produced by Lauterbur in 1973 [3].
Evolution of MRI technique [2,4].
| 1857-1952 | Sir Joseph Larmor gave the Larmor relationship. |
| 1882 | Nicola Tesla for the first time discovered the rotating magnetic field in Budapest. |
| 1937 | Isidor Isaac Rabi described for the first time phenomenon of nuclear magnetic resonance i.e., based on the emission of radio waves by the atomic nuclei when exposed to strong magnetic field. |
| 1956 | Tesla Unit proclaimed by the International Electro-technical Commission-Committee of Action |
| 1946 | Bloch and Purcell recorded the magnetic resonance in the bulk materials such as liquids and solids. |
| 1973 | First magnetic resonance image produced by Paul Lauterbur. |
| 1977 | First human scan made as MRI prototype by Peter Mansfield. |
| 1977 | Raymand Damadian completed the first MR scanner. |
| 1980 | Bottomley produced the first localized MRS image of heart and brain. |
| 2003 | Nobel Prize - Lauterbur and Mansfield |
MRI techniques are currently being used in dentistry for diagnosis of temporomandibular joint diseases which may lead to a degeneration of the discs, inflammatory conditions of the facial skeleton, and in examination of the salivary glands, maxillary sinuses, masseter muscles, in the detection of early bone changes such as tumors, fractures, inflammatory conditions and hematoma. The growth of the facial skeleton can also be monitored by MRI with the help of control points. More recently MRI has found application in the implant dentistry by providing more precise information regarding the bone height, bone density and contour [5]. Recently, new approaches to the application of MRI in various branches of dentistry have been proposed (endodontics, prosthodontics, orthodontics and diagnosis of salivary gland tumors, facial swellings and jaw lesions) [1].
Initially its implementation was only up to the neuro-axis but in recent times it extends to all parts of the body including the oral cavity, either solely or in combination with other techniques, to achieve highest diagnostic accuracy [2].
The rapid growth in clinical applications has been accompanied by numerous technologic advances in MR imaging over the past few years. These advances have affected imaging techniques, image quality, sitting considerations, safety concerns and several other aspects of the clinical applications of MR imaging [3].
Principle of Working: MRI works by obtaining a resonance signal from the hydrogen nucleus, and therefore, is essentially an imaging of water in the tissue. Spin echo and inversion recovery are the two most commonly used imaging sequences whose modifications have resulted in enhancement of signal-noise ratio, contrast resolution and imaging time. Multi-slice, multi-echo spin-echo imaging has become the major MR imaging technique used for clinical imaging; a standard spin-echo examination includes one set of spin-lattice relaxation time (Tl)-weighted images, short repetition time (TR) and one set of spin-spin relaxation time (T2)-weighted images (long TR) [3].
Physics of Image Production by MRI: The magnetic field is produced by three electromagnetic coils within the circle of imaging magnet. The coils surround the patient and produce magnetic field that oppose and redirect the magnetic flux in three right angled directions to delineate individual volume of tissues (vowels), which are subjected to magnetic fields of higher strength. The local magnetic field with all hydrogen protons is segregated, at specific pixel to the same resonant frequency which is known as selective excitation. Initially when a Radio Frequency (RF) pulse with a range of frequencies is used, it leads to the excitation of a pixel array of tissue at certain frequency and this excited pixel array radiates that typical frequency which recognizes and localizes it. The slice thickness is decided by the band width or spectrum of frequencies of the RF pulse. Finally, the visual image of the part of the body that has been scanned is produced by the computer which is transferred to a film [2].
MRI has a vital role in formulating diagnosis of soft tissue elements, vascular components, and intra-cranial involvement, tumors or complicated inflammatory conditions, abnormalities involving the skull base can be specifically detected. MRI is clinically indicated in retrocochlear sensorineural hearing loss, facial nerve paralysis, and vertigo [6].
Need for the Study: Though studies have been done on the use of MRI in medical field, very few studies have been reported on the role of MRI in dentistry. Hence, due to scanty literature which is available, the present review was done with an aim of assessing the applicability, feasibility and efficacy of MRI in the field of dentistry.
Materials and Methods
Eligibility Criteria: The articles which were published in English, dated from the year 1970 to 2015 were included in this review. The search terms for articles were the terms either in the title or abstract. Full text original research articles were considered. Unpublished articles in press and personal communications were excluded.
Inclusion Criteria
Studies evaluating the use of MRI in dentistry (Only original research articles were included to eliminate the potential bias due to the difference in the inclusion and exclusion criteria and also due to the possibility of difference in the objectives of other review articles).
Studies evaluating the role of MRI in endodontic treatment, dental prosthetics, oral cavity lesions, facial swellings, orthodontic treatment and Temporomandibular Joint (TMJ) were only selected for the review.
Exclusion Criteria
Review articles, case reports, case series and pilot studies were excluded.
Studies without MRI diagnostic test were excluded.
Search Method for Identification of Studies: For the identification of the studies included in this review, we devised the search strategy for each database. The search strategy used a combination of controlled vocabulary and free text terms. The main database was PubMed, PubMed Central, Cochrane Review, Embase and Google Scholar [Table/Fig-2].
Electronic Searches
Pub Med (1970-2015)
Pub Med Central (1970-2015)
Cochrane Review (1970-2015)
Embase (1970-2015)
Google Scholar (1970-2015)
Other Sources: The search also included the hand search of the journals fulfilling the inclusion criterion for the review.
Results
In-vivo and in-vitro studies have been presented in tabular form [Table/Fig-3,4].
| Study,Author Name,Year | Objective | Type of View | Sample Size | Age Group | Interpretation |
|---|
| Kumar R et al., (2015) [7] | To evaluate whether MRI findings of various degrees of disk displacement could be correlated with the presence or absence of clinical signs and symptoms of temporomandibular disorders in symptomatic and asymptomatic subjects. | Combined imaging in the sagittal and coronal planes | 44 patients | 20-40 years | Disk displacement on MRI correlated well with presence or absence of clinical signs and symptoms of temporomandibular disorders with high sensitivity (90%) and specificity (83.3%) respectively. |
| Jung YW et al., (2015) [8] | To assess the role of MRI in predication of pain and limited mouth opening in patients with Temporomandibular Joint (TMJ) Internal Derangement (ID). | Oblique-sagittal plane image | 48 patients | 10-65 years | Significant correlation was found between clinical symptoms and MRI findings of internal derangement. The degree of anterior disc displacement was found to be useful for predicting pain in patients with TMJ ID. |
| Oda M et al., (2014) [9] | To assess the use of functional Magnetic Resonance Imaging (fMRI) in the quantification of changes in brain activity during experimental occlusal interference. | Axial and coronal T1-weighted images | 16 healthy volunteers | Mean age, 33.3 years; Age range, 25–46 years | The findings of the study suggested that adjustments for experimental occlusal interference can be objectively evaluated using MRI. |
| Chavan SJ et al., (2014) [10] | To evaluate and compare temporomandibular joint changes especially disk-condyle-fossa relationship following functional treatment of skeletal Class II division 1 malocclusion using Twin Block and Bionator appliances. | Sagittal T1 images | 30 patients (13 males and 17 females) | 9-14 Years | The MRI findings at the end of 6 months follow-up period suggested that the condyles acquired a more anterior position in the fossa while the disk moved more posteriorly in relation to the condyle when compared to the pre-treatment positions of the condyle and disc |
| Hsieh LC et al., (2014) [11] | To develop MRI indicators to predict trismus outcome for post-operative oral cavity cancer patients who received adjuvant Intensity-Modulated Radiation Therapy (IMRT). | Axial T1 weighted image (T1W), coronal T2 weighted image (T2W), axial T2W with fat saturation, sagittal, coronal T1W post-gadolinium and axial T1W post-gadolinium with fat saturation sequences. | 22 patients | | The Signal Abnormality (SA) score, as determined using MRI, was found to reflect the severity of the radiation injury and trismus severity in the oral cancer patients receiving intensity modulated radiation therapy. |
| Gunzinger J M et al., (2014) [12] | To evaluate new MRI sequences with multi-acquisition variable-resonance image combination (MAVRIC SL) in comparison to conventional high-bandwidth techniques. | T1w fast spin-echo sequence | 25 patients with dental implants | | The findings revealed that MAVRIC-fast could become useful for artifact reduction in PET/MR for patients with dental implants. This might improve diagnostic accuracy especially for patients with tumors in the oropharynx and substantially improve accuracy of PET quantification. |
| Davachi B et al., (2014) [13] | To evaluate the efficacy of magnetic resonance imaging (MRI) and color doppler ultrasonography parameters in the diagnosis and differentiation of benign and malignant salivary gland tumors. | 0.5 Tesla | 22 | Mean age 46.59±13.97 years | Both MRI and ultrasonography were found to have high accuracy in the localization of tumors. In the MRI image well-identified border was found to be sign of benign tumors and invasion to adjacent structures was a predictive factor for malignancy. |
| Koh KJ et al., (2013) [14] | To evaluate the relationship between anterior disc displacement and effusion in Temporomandibular Disorder (TMD) using MRI | T1- and T2-weighted images with para-sagittal and para-coronal images | 253 patients | Mean age 28.5 Years | The anterior disc displacement was not related to the MRI findings of effusion in TMD patients |
| Makdissi J et al., (2013) [15] | To determine the prevalence of incidental findings in MRI of the TMJ | Sagittal oblique proton density and T2 weighted imaging | 730 patients | | Out of the 730 patients incidental findings were reported in 53 (7.3%) patients out of which 11 (1.5%) were intracranial and 42 (5.7%) were extracranial findings. The extracranial findings consisted of paranasal sinuses, mastoid air cells, muscle hypertrophy, lymphadenopathy and salivary glands. |
| Ogura I et al., (2012) [16] | To evaluate the MR characteristics of TMJ disc displacement in elderly patients. | T2 weighted sagittal imaging | 847 patients | 50 years and under aged 51 years | The study suggests that MR characteristics of TMJ disc displacement in elderly patients included reduction, joint effusion and osteoarthrosis. While difference between the elderly group and control group was found to be statistically significant for reduction (p=0.003) and osteoarthrosis (p=0.001), the results were non –significant for joint effusion (p=0.602) |
| Candirli C et al., (2012) [17] | To investigate the effect of the Autologous Blood Injection (ABI) for chronic recurrent TMJ dislocation using MRI. | Oblique sagittal T1-weighted spin echo and also oblique sagittal T2-weighted fast spin echo. | 14 patients | 17-74 years | In pre-injection MRI evaluation, it was identified that the patients had unilateral or bilateral condyles anterior to the eminence with their mouths in the open position. In the first month after the injection, significant changes were recorded in the MRIs with condyle position either at the apex of the eminence or posterior to it. |
| Gokce SM et al., (2012) [18] | To evaluate the swallowing-induced vertical and horizontal displacements of the hyoid bone in subjects with 2 different magnitudes of skeletal Class III malocclusion. | | 55 patients | Mild Class III group comprised 19 subjects (11 males, 8 females; age range, 18 - 25 years; mean age, 21.5 years); the severe Class III group, 16 subjects (10 males, 6 females; age range, 17 - 25 years; mean age, 19 years); and the Class I group, 20 patients (10 males, 10 females; age range, 17 - 24 years; mean age, 19.5 years). | At all stages of swallowing, the vertical position of the hyoid bone in the severe Class III malocclusion group was significantly lower than those in the mild Class III and Class I malocclusion groups. Similarly, the horizontal displacement of the hyoid bone was found to be significantly associated with the severity of malocclusion, i.e., the degree of Class III malocclusion, while the amount of anterior displacement of the hyoid bone decreased with an increase in the severity of the Class III deformity |
| Yildirim D et al., (2011) [19] | To determine the elasticity of the disc by measuring the amount of elongation during mouth opening using MRI. | Coronal T1 and multiplane oblique T2 weighted and sagittal oblique images. | 49 patients | | The degree of deformation in the disc and severity of the symptoms (pain, limitation of movement, restlessness, sensitivity) increased as the ER value declined. |
| D’Ippolito SM et al., (2010) [20] | To evaluate the visibility of the Lateral Pterygoid Muscle (LPM) in TMJ images obtained by MRI, using different projections and to compare image findings with clinical symptoms of patients with and without Temporomandibular Disorders (TMD). | Oblique sagittal and axial images Oblique sagittal and axial images | 50 | | The oblique sagittal and axial images of the TMJ clearly showed the lateral pterygoid muscle. Hypertrophy (1.45%), atrophy (2.85%) and contracture (2.85%) were the abnormalities found in the lateral pterygoid muscle. TMD signs, such as hyper mobility (11.4%), hypo mobility (12.9%) and disc displacement (20.0%), could be seen in TMJ images. |
| Pompa V et al., (2010) [21] | To evaluate the reliability of MRI compared with Computed Tomography (CT) for dental implant planning in respect to bone measurements. | T2-weighted and Tl-weighted Images | 30 | | The bone heights measured at different points using MRI and CT scan varied between 0.4mm to 0.11mm. There was no statistically significant difference in MRI and CT scan findings for the bone height measurements. |
| Zhang SY et al., (2010) [22] | To evaluate the post-surgical success of this technique to reposition and stabilize the TMJ articular discs. | 3T | 81 Patients | 23-74 Years | Post-operative MRIs provided confirm that procedure has successful repositioning of the articular discs in unilateral TMJ ID at one to seven days post-surgery. |
| Study, Author Name, Year | Objective | Type of View | Sample Size | Interpretation |
|---|
| Kajan ZD et al.,(2015) [23] | To compare the metal artifacts from common metal orthodontic brackets in magnetic resonance imaging. | Three different sequences of coronal and axial images were obtained: spin-echo T1-weighted images, fast spin-echo T2-weighted images, and fluid-attenuated inversion recovery images. | Dry mandible with 12 intact premolars | The findings from the MRI revealed that the 3M and Dentaurum brackets with NiTi wires induced smaller artifacts along all axes than those with SS wires. |
| Gorgulu S et al., (2014) [24] | To evaluate the heating and magnetic field interactions of fixed orthodontic appliances with different wires and ligaments in a 3-T MRI environment and to estimate the safety of these orthodontic materials. | T1 weighted axial sequencing | 40 non-carious maxillary teeth | The temperature changes of the specimens were considered to be within acceptable ranges. With regard to magnetic field interactions, brackets were considered MR safe. |
| Akgun OM et al., (2014) [25] | To compare the effect of Magnetic Resonance Imaging (MRI) on microleakage of Class II bonded amalgam versus classical amalgam restorations. | 1.5T superconductive unit | Class II cavities 40 permanent molar teeth | The findings of the study revealed that the occlusal and gingival surface microleakage did not increased after MRI exposure. Similar findings were observed for the teeth with bonded amalgam filling. |
| Tymofiyeva O et al., (2013) [26] | To investigate the potential influence of standard dental materials on dental MRI (dMRI) by estimating the magnetic susceptibility with the help of the MRI-based geometric distortion method | T2 weighted images | Dental materials such as composite, gold alloy, titanium alloy etc. | MRI detect relatively strong distortions materials and they classified as compatible I such as composite, amalgam, gold alloy, gold- ceramic crowns, titanium alloy and NiTi orthodontics wires and another were classified as non-compatible materials such as stainless steel orthodontic appliances and CoCr. |
| Yilmaz S et al., (2013) [27] | To evaluate the effects of 3 T magnetic field on microleakage of amalgam restorations containing three different types of silver (Ag). | T1 weighted, 3T | 60 extracted teeth | An MRI of 1.5 T is known to be safe for amalgam restorations. However, our research indicates that MRI is not completely devoid of any effects on amalgam restorations. |
| Hasegawa M et al., (2013) [28] | To estimate the risk of injury from Radio Frequency (RF) heating of metallic dental devices in use during 3.0 T MRI. | 3.0 T MRI | Three unit bridges, a full-arch fixed dental prosthesis and an orthodontic appliance | Relatively minor RF heating of dental casting material-based prostheses and orthodontic appliances may exhibit RF heating above the industrial standard. |
| Klinke T et al., (2012) [29] | In-vitro study was to identify and evaluate the artifacts produced by different dental restoration materials in CT and MRI images | T1-weighted spin-echo sequence and T2-weighted turbo spin-echo sequence | 44 different materials (metal and non-metal) | In MRI, 13 out of 44 materials produced artifacts, while in CT 41 out of 44 materials showed artifacts. Artifacts produced in both MRI and CT images were categorized according to the size of the artifact. |
| Idiyatullin D. et al., (2011) [30] | To assess the feasibility of a recently developed MRI technique, called Sweep Imaging with Fourier Transform (SWIFT), to visualize dental tissues. | 9.4T system and 4T system | 6 teeth | It has the potential to image minute dental structures within clinically relevant scanning times. This technology has implications for endodontists since it offers a potential method to longitudinally evaluate teeth where pulp and root structures have been regenerated. |
| Tanasiewicz M et al., (2010) [5] | Possibility to use 3D spin echo magnetic resonance imaging techniques in the dentistry within the scope of a dimensional imaging of the inner spaces of teeth during an prosthetic procedure. | 4.7T | 6 extracted molar teeth | MRI made it possible to compare the quality of internal tooth space after preparation for inner root canal fixations constructed using both classical methods (polymer mass impression) and non-impressional methods (MRI representation). |
Discussion
MRI has a promising approach in dentistry. It has become one of the best methods in recent decades because of its non-invasiveness, non-ionizing radiation and its ability to differentiate between the soft and hard tissues. In the recent past the MRI has found widespread usage in dentistry despite the high cost, differential and limited accessibility of the MRI equipment. MRI being a non-invasive technique with the use of non–ionizing radiation has been used in diagnosis of TMJ disorders, soft tissue pathologies and bone topography for the placement of the dental implants [21].
MRI is the new modality in the diagnosis of TMJ disorders. MRI demonstrates the internal structure of TMJ with great precision and contrast resolution. TMJ dysfunction is a common condition that is best evaluated with MRI. The MRI findings in terms of functional aspect of disc position, degree of disc displacement, disc deformity, joint effusion, and osteoarthritis has been used for the prediction of Temporomandibular Dysfuction (TMD) symptoms in patients with and without TMJ disorders. The anterior disc displacement as seen in the MRI correlates well with the presence and absence of the symptoms of TMJ disorders. The findings are in agreement with study conducted by Kumar et al., [7]. Furthermore, the greater the degree of anterior disc displacement, greater are the chances of pain and limited mouth opening, the findings are in agreement with the study conducted by Jung et al., who demonstrated greater degree of disc displacement in patients with severe pain related to TMD [8]. The alteration in the shape of the disc secondary to disc displacement as examined in the MRI scans has also been recognized as the important feature of internal derangement of TMJ as seen in study conducted by Chavan SJ et al., [10]. Deformation most commonly begins with thickening and enlargement of the posterior band of the disc. There are few studies related to TMJ conducted by Chavan SJ et al., to compare the changes in TMJ by using Twin block and Bionator appliance therapy using T1 weighted images and found that condyles occupied a more anterior position in the fossa to its pre-treatment position, while the disk moved more posteriorly in relation to the condyle [10]. According to the study conducted by Ogura I et al., on elderly patients; the MR characteristics of TMJ disc displacement was assessed by T2 weighted images and found reduction, joint effusion and osteoarthrosis on MRI [16]. Makdissi J et al., in 2013 conducted a study to determine the prevalence of intra-cranial and extra-cranial incidental findings in MRI of the TMJ using T2 images and found early detection of incidental findings using MRI can play a significant role if timely reported and communicated to a clinician [15]. Similarly the study by Candirli C et al., to investigate the effect of the Autologous Blood Injection (ABI) for chronic recurrent TMJ dislocation using T1 and T2 weighted images of MRI [17].
MRI plays an important role in the pre–implant evaluation than CT for a successful implant therapy as seen in study conducted by Pompa V et al., in 2010, where the reliability of MRI compared with CT for dental implant planning in respect to bone measurements was done by T1 and T2 weighted images was more when compared to CT scan [21].
MRI is an accurate technique in diagnosis and differentiating between the malignant and benign salivary gland tumors than color doppler ultrasonography. Davachi B et al., conducted a study to evaluate the efficacy of MRI and color doppler ultrasonography parameters in the diagnosis and differentiation of benign and malignant salivary gland tumors [13]. MRI showed a well-identified border which was a sign of benign tumors and invasion to adjacent structures was a predictive factor for malignancy.
MRI can also be used on amalgam restoration. Yilmaz S et al., found that an MRI of 1.5-T is known to be safe for amalgam restorations [27]. MRI can also be used on orthodontic materials as seen in study conducted by Gorgulu S et al., who assessed the heating and magnetic field interactions of fixed orthodontic appliances in a 3-T MRI environment and found orthodontic appliances to be safe for MRI [24].
In present scenario MRI is considered better than CT, since it has the advantage of lower radiation exposure along with lesser dimensional error and no detrimental effects.
Applications in Dentistry: MRI plays a significant role in diagnosis and management of diseases. It has many advantages, along with few drawbacks [Table/Fig-5]. In dentistry, MRI has been found to be extremely useful in elucidating the exact anatomical location and extent of the disease. Moreover, ultrasonography cannot show the associations between tumor and adjacent structures, and thus, it is indicated to use MRI whenever tumors are big or judged to have higher possibility for malignancy or intruded to adjacent structures [13]. The additional advantage of MRI is the lack of ionizing radiation and excellent soft-tissue contrast. Involvement of condyle of mandible is not apparent on radiographs or CT images. MRI has an important role in examining the true extent of the lesions and there may be slight changes in RF in areas which looks normal on radiographs or CT.
Advantages and disadvantages of MRI.
| ADVANTAGES | DISADVANTAGES |
|---|
| 1. Non-invasive. | 1. Claustrophobia. |
| 2. No detrimental effect as it uses non- ionizing radiation. | 2. Expensive and very noisy. |
| 3. Helps to differentiate soft tissue from one another due to contrast resolution. | 3. Contraindicated in patients with cardiac pacemakers, implantable defibrillators etc. |
| 4. Multiplanar image (sagittal, coronal, oblique) can be obtained. | 4. Bone marrow gives signal but not bone. |
| 5. Safe in pregnant ladies and children. | 5. Distinction between malignant and benign tumors is difficult. |
| 6. Artifacts with dental filling are not seen. | |
| 7. Manipulation of image can be done. | |
In case of malignancy prediction, MRI shows the presence of invasion to adjacent structure was an acceptable parameter. MRI is the preferred imaging technique when information regarding the articular disc or the presence of adhesions, perforations, or joint effusion is desired. Despite MRI having the benefit of creating an image without using ionizing radiation, it is not used broadly by Orthodontist due to being more costlier [31]. The advantages and the disadvantages of MRI have been summarized in [Table/Fig-5].
Conclusion
MRI has a promising future in dentistry. It can be used in implant dentistry, diagnosis and treatment planning, jaw lesion, diseases of TMJ, orthodontic treatment, endodontic treatment etc., to achieve better prognosis. There are few exceptions of medical counter-effects, MR is a valid alternative to CT; it is biologically safe (does not use ionizing radiation), provides clear images of the implant sites, TMJ, salivary gland tumors and it also allows the use in more complex cases of TMJ. This technique has not pursued for the higher risk of magnetic susceptibility artifacts that we have with the gradient-echo images, and also for the scan time in regard to the two-dimensional spin-echo sequences, with the associated risk of degradation of the image due to movement of the patient. MRI gives better results in TMJ related diseases. MRI technology has been reported to produce tooth surface digitization with an accuracy and precision sufficient for production of dental restorations and to detect root resorption in orthodontic cases. The results that have been achieved indicate the possibility to employ techniques of MRI in dentistry.
[1]. Shah N, Bansal N, Logani A, Recent advances in imaging technologies in dentistryWorld J Radiol 2014 6(10):794-807. [Google Scholar]
[2]. Katti G, Ara SA, Shireen A, Magnetic resonance imaging (MRI) – A reviewInt J Dent Clinics 2011 3(1):65-70. [Google Scholar]
[3]. Scherzinger AL, Hendee WR, Basic principles of magnetic resonance imaging-An update, In High-tech medicine [Special Issue]West J Med 1985 143:782-92. [Google Scholar]
[4]. Sobol WT, Recent advances in MRI technology: Implications for image quality and patient safetySaudi J Ophthalmol 2012 26:393-99. [Google Scholar]
[5]. Tanasiewicz M, Magnetic resonance imaging in human teeth internal space visualization for requirements of dental prostheticsJ Clin Exp Dent 2010 2(1):e6-11. [Google Scholar]
[6]. Blickman JG, Parker BR, Barnes PD, Pediatric Radiology: The Requisites 2009 3rd edMosby Elsevier:297-338. [Google Scholar]
[7]. Kumar R, Pallagatti S, Sheikh S, Mittal A, Gupta D, Gupta S, Correlation between clinical findings of temporomandibular disorders and MRI characteristics of disc displacementOpen Dent J 2015 9:273-81. [Google Scholar]
[8]. Jung YW, Park SH, On SW, Song SII, Correlation between clinical symptoms and magnetic resonance imaging findings in patients with temporomandibular joint internal derangementJ Korean Assoc Oral Maxillofac Surg 2015 41:125-32. [Google Scholar]
[9]. Oda M, Yoshino K, Tanaka T, Shiiba S, Makihara E, Miyamoto I, Identification and adjustment of experimental occlusal interference using functional magnetic resonance imagingBMC Oral Health 2014 14:124 [Google Scholar]
[10]. Chavan SJ, Bhad WA, Doshi UH, Comparison of temporomandibular joint changes in twin block and bionator appliance therapy: A magnetic resonance imaging studyProgress in Orthod 2014 15:57 [Google Scholar]
[11]. Hsieh L-C, Chen JW, Wang L-Y, Tsang Y-M, Shueng P-W, Liao LJ, Predicting the severity and prognosis of trismus after intensity-modulated radiation therapy for oral cancer patients by magnetic resonance imagingPLoS ONE 2014 9(3):e92561 [Google Scholar]
[12]. Gunzinger JM, Delso G, Boss A, Porto M, Davison H, Gustav K von Schulthess GKV, Metal artifact reduction in patients with dental implants using multispectral three-dimensional data acquisition for hybrid PET/MRIEJNMMI Physics 2014 1:102 [Google Scholar]
[13]. Davachi B, Imanimoghaddam M, Majidi MR, Sahebalam A, Johari M, Langaroodi AJ, The efficacy of magnetic resonance imaging and color doppler ultrasonography in diagnosis of salivary gland tumorsJ Dent Res Dent Clin Dent Prospect 2014 8(4):246-51. [Google Scholar]
[14]. Koh KJ, Park HN, Kim KA, Relationship between anterior disc displacement with/without reduction and effusion in temporomandibular disorder patients using magnetic resonance imagingImaging Sci Dent 2013 43:245-51. [Google Scholar]
[15]. Makdissi J, Pawar RR, Radon M, Holmes SB, Incidental findings on MRI of the temporomandibular jointDentomaxillofac Radiol 2013 42:20130175 [Google Scholar]
[16]. Ogura I, Kaneda T, Mori S, Sakayanagi M, Kato M, Magnetic resonance characteristics of temporomandibular joint disc displacement in elderly patientsDentomaxillofac Radiol 2012 41:122-25. [Google Scholar]
[17]. Candirli C, Yüce S, Cavus UY, Akin K, Cakir B, Autologous blood injection to the temporomandibular joint: Magnetic resonance imaging findingsImaging Sci Dent 2012 42:13-18. [Google Scholar]
[18]. Gokcea SM, Gokceb HS, Gorgulua S, Karacayc S, Akcad E, Olmeza H, Relationship between Class III malocclusion and hyoid bone displacement during swallowing: a cine-magnetic resonance imaging studyKorean J Orthod 2012 42(4):190-200. [Google Scholar]
[19]. Yildirim D, Dergin G, Tamam C, Moroglu S, Gurses B, Indirect measurement of the temporomandibular joint disc elasticity with magnetic resonance imagingDentomaxillofac Radiol 2011 40:422-28. [Google Scholar]
[20]. D’Ippolito SM, Wolosker AMB, D’Ippolito G, de Souza BH, Pereira MF, Evaluation of the lateral pterygoid muscle using magnetic resonance imagingDentomaxillofac Radiol 2010 39:494-500. [Google Scholar]
[21]. Pompa V, Galasso S, Cassetta M, Pompa G, Angelis FD, Carlo SD, A comparative study of magnetic resonance (MR) and computed tomography (CT) in the pre-implant evaluationAnnali di Stomatologia 2010 I(3-4):33-38. [Google Scholar]
[22]. Zhang SY, Liu XM, Yang XJ, Yang C, Chen MJ, Haddad MS, Temporomandibular joint disc repositioning using bone anchors: an immediate post-surgical evaluation by magnetic resonance imagingBMC Musculoskeletal Disorders 2010 11:262 [Google Scholar]
[23]. Kajan ZD, Khademi J, deh AA, Hemmaty YB, Roushan ZA, A comparative study of metal artifacts from common metal orthodontic brackets in magnetic resonance imagingImaging Sci Dent 2015 45:159-68. [Google Scholar]
[24]. Gorgulu S, Ayyıldız S, Kamburoglu K, Gokçe S, Ozen T, Effect of orthodontic brackets and different wires on radiofrequency heating and magnetic field interactions during 3-T MRIDentomaxillofac Radiol 2014 43:20130356 [Google Scholar]
[25]. Akgun OM, Polat GG, Illca AT, Yildirim C, Demir P, Basak F, Does magnetic resonance imaging affect the microleakage of amalgam restorations?Iran J Radiol 2014 11(3):e15565 [Google Scholar]
[26]. Tymofiyeva O, Vaegler S, Rottner K, Boldt J, Hopfgartner AJ, Proff PC, Influence of dental materials on dental MRIDentomaxillofac Radiol 2013 42:20120271 [Google Scholar]
[27]. Yilmaz S, Misirliŏglu M, The effect of 3 T MRI on microleakage of amalgam restorationsDentomaxillofac Radiol 2013 42:20130072 [Google Scholar]
[28]. Hasegawa M, Miyata K, Abe Y, Ishigami T, Radiofrequency heating of metallic dental devices during 3.0 T MRIDentomaxillofac Radiol 2013 42:20120234 [Google Scholar]
[29]. Klinke T, Daboul A, Maron J, Gredes T, Puls R, Jaghsi A, Artifacts in magnetic resonance imaging and computed tomography caused by dental materialsPLoS ONE 2012 7(2):e31766 [Google Scholar]
[30]. Idiyatullin D, Corum C, Moeller S, Prasad HS, Garwood M, Nixdorf DR, Dental MRI: Making the invisible visibleJ Endod 2011 37(6):745-52. [Google Scholar]
[31]. Quintero JC, Trosien A, Hatcher D, Kapil S, Craniofacial imaging in orthodontics: Historical perspective, current status, and future developmentsAngle Orthod 1999 69:491-506. [Google Scholar]