Breast is considered anatomically as modified sweat gland. In human beings the presence of more than two breasts with or without a nipple and areola is termed as Polymastia. It is synonymous with supernumerary or Ectopic Breast Tissue (EBT). It can be seen in up to 6% of the population. Supernumerary breasts are mostly seen along the milk line and commonly found in the axilla, chest wall, rarely in vulva. It may present as unilateral or bilateral swelling [1]. During the early weeks of embryonic development, the mammary milk lines shows two ectodermal thickenings along the sides of the embryo. It extends from the axilla to the inguinal region and upto the medial aspect of the thigh on either sides. The embryologic mammary ridge usually disappears, except for two segments in the pectoral region, which later becomes the breasts. The abnormality is harmless unless they cause discomfort, thus their recognition and distinction from other breast pathologies, either benign or malignant, is necessary [2].
Failure of any portion of the mammary ridge to involute can lead to ectopic breast tissue with (polythelia) or without (polymastia) a nipple-areolar complex [3]. The incidence of polythelia in the general population ranges between 0.22 to 5.6%, depending on factors such as inheritance and ethnicity. It is usually seen in males than females and more commonly occurs in blacks than whites [4]. In 2011, the American Society of Plastic Surgeons published an algorithm for treatment of axillary accessory breast tissue [Table/Fig-1] [5]. Incomplete excision of the glandular elements may result in a residual mass and necessitating a secondary procedure. Direct excision of larger masses result in long unsightly scars, disruption of numerous lymphatic channels and a significant amount of axillary dead space. Studies recommended a combination of surgical excision and liposuction, according to the features of the tissue [5]. As per our data collection from various articles searched in pubmed and Google, we assume that this is the largest series from India, a total of 32 cases of Benign Accessory Breast Disease (BABD).
To evaluate the presentation of symptoms, investigations required for diagnosis and the management to improve the treatment protocols in patients with breast diseases.
Materials and Methods
The study was conducted in Department of Surgery at MMIMSR, Mullana, Ambala. The data was studied retrospectively from January 2013 and January 2016 from the breast disease cases either benign or malignant. A total number of 32 cases were taken diagnosed as BABD. All the cases of age group (23-67 years) and gender of male and female were enrolled. Those cases diagnosed with other breast lesions than accessory breast were excluded from the study. All patients were subjected to routine blood investigations in addition to pre-operative imaging like ultrasonography, cytology and wherever necessary mammography was done. Family history was significant in one case only: one patient got operated for bilateral accessory breast in whom her child had similar disease as unilateral swelling but she refused further evaluation and treatment. Accessory breast tissue was excised under general anesthesia.
Results
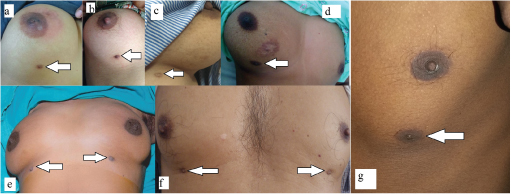
Out of total 200 breast cases, 32 cases diagnosed as accessory breast disease were included in this study. Out 32 cases, 1 (3.12%) female patient had accessory axillary fibroadenoma, 7(21.87%) had unilateral and 1(3.12%) had bilateral accessory nipple in females, 1(3.12%) male had unilateral and 1(3.12%) male had bilateral accessory nipples, 16(50%) had unilateral and 5(15.62%) cases were diagnosed as bilateral accessory axillary swelling [Table/Fig-2]. The age range of patients was 23-67 years. All cases presented with a swelling or heaviness in the axillary region or either as extra nipple. Out of 32, 15 (46.87%) cases had complaint of heaviness and pain in the axillary area, mastalgia (4 cases) and 7(21.87%) cases had breast hypertrophy. There were total 10 (31.25%) cases of supernummery nipple and all these patients came for routine checkup, cosmetic purpose and investigations did not reveal any abnormality. In 6(18.75%) cases, accessory nipple was located at inframammary fold and was about the size of 0 .5x1cm approx. In 3(9.37%) cases the nipple was present just above (2-3cm below the normal nipple) the inframammary fold along the milk line [Table/Fig-3a-g]. In one case there was inflammation to the peri-areolar region with accessory nipple [Table/Fig-3a]. There was one more interesting case of accessory nipple, she reported with a pain and enlargement of the right breast(non- lactating) as compared to left side which was unusual and in same case scar mark of previous surgery was also seen for fibroadenoma [Table/Fig-3d]. One male patient admitted for cosmetic reason with the extra nipple on left side. It was of I cm in size as accessory nipple in subcoastel area [Table/Fig-3g].
Details of the patient, clinical presentations and its treatment.
| Age and Gender (female) | Site | Clinical features /Chief Complaints | Treatment |
|---|
| 1 | 29 years (married) female | Left side, Unilateral axillary swelling | Unsightly bump noted 2 years back during pregnancy, On Examination non warm, non –tender, soft swelling 3x2x2 cm in Left Axilla without any overlying skin changes. | Excision with Z plasty. |
| 2 | 26 years (unmarried) female | Right sided, unilateral axillary swelling | Swelling recognized during adolescence at age of 14 years when she achieved puberty, which is slowly increasing in size. On Examination; non warm, non-tender, soft swelling 2x2.8x1 cm with normal overlying skin. | Surgery |
| 3 | 36 years (multiparous) female | Right sided, unilateral, axillary swelling | Swelling first noted during puberty 21 years back and increased in size during first pregnancy 15 years back On Examination 5x4x2 cm non warm non tender swelling axilla. | Excision with Z plasty |
| 4 | 35 years (married) female | Right sided, unilateral, axillary swelling | Swelling was present since birth small in size but increased during pregnancy- 4 years back. swelling was soft in consistency, of size 5x3x3 cm, non warm, non- tender in axilla. | Surgery, with Z plasty |
| 5 | 38 years (married) female | Left sided, unilateral axillary swelling | Swelling first noted 10 years back during pregnancy, On Examination 6x3x2 cm, pedunculated, firm, mild tenderness alongwith swelling in axilla . | Surgery, with Z plasty |
| 6 | 40 years (married) female | Left sided, unilateral, axillary swelling | Swelling noticed 15 years back, with gradual increase during every pregnancy (three pregnancies). On examination, it was non-tender, soft in nature of size 4x2x1.5 cm in axilla . | Elliptical excision |
| 7 | 45 years (married) female | Bilateral, axillary swelling | Swelling identified 12 years back during first pregnancy in bilateral axillary area. On examination- non-tender, soft swelling, 2.5x1.5x1.5 cm approx. | Surgery with z- plasty |
| 8 | 38 years (married) female | Right sided, unilateral axillary swelling | Swelling was present since puberty, increased during pregnancy. On examination; size- 5x3x3 cm, non tender, soft swelling axilla. | Excision |
| 9 | 56 years (married) female | Right sided, unilateral axillary swelling | Swelling noticed during first pregnancy 30 years back with gradual increase in size during all pregnancies (4), Examination 7x4x3 cm, soft, non warm, mildly tender swelling axilla. | Surgery with Z -pasty |
| 10 | 38 years (married) female | Right sided, unilateral | Swelling Noticed 24 years back, with occasional complaints of heaviness in axilla, On examination-3x 2x 2 cm non warm, non tender swelling axilla. | Elliptical Excision |
| 11 | 57 years (married) female | Bilateral axillary swelling | Swelling first noticed 33 years back, globular in shape, without any significant complaints except unsightly appearance. On Examination- 3x4x4 cm. firm, non-tender swelling axilla. | Elliptical incision |
| 12 | 55 years (married) female | Bilateral axillary swelling | Patient felt heaviness in axilla since teenage, and also increased since then. She has three children. Eldest 30 years (she is also having swelling in the axilla). On examination 7x4x4 cm non warm, non tender, soft swellings bilateral axilla without any skin changes. | Surgery with Z –pasty |
| 13 | 39 (married) female | Right sided, unilateral axillary swelling | Swelling since 13 years pregnancy noticed during first pregnancy, soft, mobile, non-tender, 1x 2.5 cm. | Excision |
| 14 | 37 year (married) | Bilateral, axillary swelling | Swelling in right axilla since 10 years and in left axilla since 6 months, with heaviness in both axilla. On examination-Left side- 6x 8 x 3 cm globular in shape swelling and on right sided – 4x3x2 cm swelling globular in shape. | Surgery with Z plasty |
| 15 | 22 years (Married) female | Right sided, unilateral axillary swelling | Swelling first observed during puberty 9 years back. Her husband objects to unsightly lump axilla. On examination- 3x4x3, non warm, non –tender, soft swelling axilla. | Excision |
| 16 | 36 years female (married) | Bilateral, swelling in axilla | Bilateral axillary swellings since 4 years. On Examination; Bilateral 3x3x3 cm non warm non tender swellings axilla without skin changes. | Excision |
| 17 | 28 year, female (Married) | Left axilla swelling | Swelling was noticed 2 years back during pregnancy; it was causing lot of discomfort to her with pain. On Examination; 4x3x3 cm non warm, mildly tender swelling axilla. | Excision |
| 18 | 22 year, female (married) | Left axillary swelling, | Swelling noticed 15 days back which was causing discomfortness and mild pain. On Examination- 3x2x2 cm, firm, non-tender swelling axilla. | Excision |
| 19 | 19 years (unmarried) | Axillary swelling, fibroadenoma | Pain in the breast and axilla alongwith swelling in axilla left sided. Size was 3x4x2 cm, firm, non-tender, and mobile. | Excision |
| 20 | 47 years female, married | Unilateral accessory swelling | Swelling noticed 12 years back when patient was pregnant and increased during same period, it was firm, non-tender, mobile, 2x1x2 cm in size | Excision |
| 21 | 56 years, married | Unilateral accessory swelling | A small swelling noticed during pregnancy in the axilla, it was soft, non-tender, 3x2x1 cm in size. | Excision |
| 22 | 39 years, female, married | Unilateral accessory swelling | A swelling noticed 15 years back during pregnancy and increased in size during two subsequent pregnancies. Swelling was 4x6x4 cm, non-tender, mobile, no lymph nodes felt. | Z – plasty |
| 23 | 36 age, female | Unilateral, nipple | Unsightly appearance of accessory nipple present at anterior axillary fold along embryonic milk line, since childhood. | Excision |
| 24 | 31 year, female | Unilateral, nipple | Extra nipple present along milk line just below the inframammary fold with a scar of previous surgery in outer lower quadrant of ipsilateral breast. | Excision |
| 25 | 43 year, female | Unilateral, nipple | Patient came with complaint of extra nipple present just 2 cm below the normal nipple areola complex with abnormal nipple discharge. | Excision |
| 26 | 46 year, female | Bilateral two accessory nipples (two normal) | Patient came with accessory nipples each present just below the inframammary fold along the milk line giving unsightly appearance on both sides. | Excision |
| 27 | 28 year, male | Unilateral nipple | This male patient came with complaint of discharge from abnormally located nipple at inframammary fold along milk ridge. | Excision |
| 28 | 35 year, female | Unilateral nipple | Accessory nipple present with discharge and mild tenderness and located 3cm just below the normal nipple areola complex. Periareoler inflammation was seen which was insignificant and resolved with anti inflammatory drugs. | Excision |
| 29 | 58 year, male | Bilateral accessory nipple | This male patient presented with accessory nipples bilaterally since his childhood with recent discharge and mild tenderness with unsightly appearance just above the subcostal region. | Excision |
| 30 | 38 years, female | Unilateral accessory nipple | Presence of extra nipple in left lateral chest wall along milk line. | Excision |
| 31 | 45 years, Female | Unilateral accessory nipple | Patient complained of unsightly appearance of extra nipple located near subcostal margin. | Excision |
| 32 | 27 years, Female | Accessory nipple, unilateral, | Unsightly appearance of extra nipple present on one side of chest wall with nipple discharge and recent increase in tenderness. | Excision |
Gross appearance of the unilateral and bilateral accessory nipples in inframammary and subcoastal area; d) Another gross picture revealed enlargement of the right breast with accessory nipple (marked with arrow); e) Showing bilateral nipples in female; f) Showing in male patient; g) Showing unilateral accessory nipple in male patient (marked with arrow).
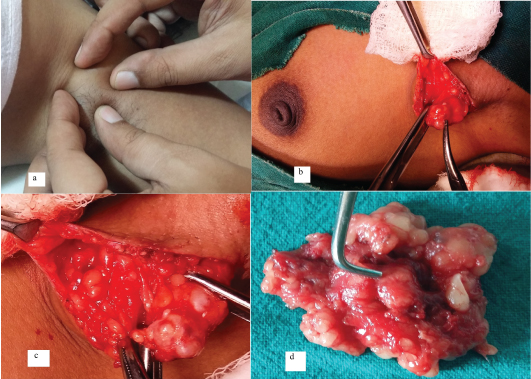
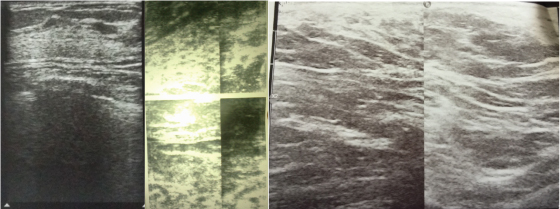
On examination of axillary swelling, it was non-tender, soft in consistency and transillumination test was negative. Total 5 cases presented as bilateral bulge in axillary area and 2 cases presented as pedunculated swelling. There was no discharge or extra nipple over axillary area. Swelling was not fixed to the underlying structures and maximum size was in the range of 3 x 4 cm – 6 x 8 cm. There were no enlarged axillary lymph nodes and neither any lesion found in the breast [Table/Fig-4]. In case of axillary fibroadenoma, her main complaint was pain and swelling in the axilla on left sided. It was 4x3x4 cm in size, firm in consistency, mobile in nature [Table/Fig-5a]. Skin over the swelling was normal and breast examination was normal. There was confusion regarding either it may be axillary lymph though rare entity but still we should keep all the possibilities in back of mind. On investigations as USG, Fine Needle Aspiration Cytology (FNAC), it came as axillary fibroadenoma. An elliptical incision was given to the surrounding area of the nodule with keeping in mind of minimal skin loss. Skin flaps raised, a nodule found alongwith accessory tissue [Table/Fig-5b]. It appeared as whitish in colour of size 6x5x4 cm [Table/Fig-5c,d]. Specimen sent for histopathology which revealed it as accessory axillary fibroadenoma. Swelling was increased in size during and within one month of the post pregnancy in all accessory breast cases. Breast hypertrophy was seen in 7 (21.87%) cases of accessory breast disease though not significant. These were studied clinically as well as by the help of imaging like ultrasound and mammography. Mammography was done in 4 cases to rule out malignancy as there was breast hypertrophy, pain in the breast along with serosanguinous discharge from the nipple which came to be normal. Ultrasonography of the axillary region revealed normal fibrofatty and fibrogladular tissue which is diagnostic of accessory breast [Table/Fig-6]. Abdominal ultrasound was also done in accessory nipple cases to rule out any other abnormalities in other organs which were normal.
Gross picture revealed bilateral and unilateral axillary accessory breast.

a) Swelling held in between the fingers on the left side of axilla; b) Gross appearance of the normal breast and dissected area of axilla showing swelling alongwith accessory tissue; c) Operative section revealed fibroadenoma held with the Allis forceps; d) Gross resected specimen.
On ultrasonography, there is evidence of the normal fibrofatty and fibrogladular tissue in axilla suggestive of accessory breast.
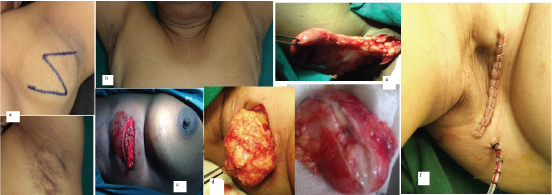
Patients were explained about the residual disease, recurrence, infection, nerve injury, and contracture formation. After the routine blood investigations, patients took for surgery under general anaesthesia. In axillary accessory breast cases, Z-shaped incision was made in 8(25%) cases in view of large size of the axillary lump to prevent the contracture formation and especially for cosmetic reason and postoperative healed scar mark without any contracture or skin loss [Table/Fig-7a,b]. In rest of the 21 (65.62%) cases, an elliptical incision was given over the axillary swelling and same at the accessory nipple site [Table/Fig-7c-e]. Skin incision was made, subcutaneous tissue dissected and flaps were raised. From the surrounding area tissue was identified and excised in toto. The excised tissue was greyish white in appearance with soft tissue consistency [Table/Fig-7d,e]. Incision was planned in such a way so that there was minimal loss of the skin to prevent contracture formation. In cases of axillary dissection, a small 12 Fr romovac suction drain was kept and skin was closed with skin stapler or either with ethiclon 2-0 suture [Table/Fig-7f]. Excised tissue was sent for histopathological examination. Postoperatively, sutures were removed on 10th to 12th day. Drains were removed when there was only 5 ml collection remaining in the bag, either on 5th or 7th day of the surgery. In 6 cases, the drain was kept upto 9th to 12th day of surgery as there was collection upto 20ml. In our study, wound dehiscence occurred in 3 (9.37%) cases, suture line infection in 2 (6.25%) cases, lymphoedema in 2 cases after the 17th day of surgery, and hypertrophy of the scar 2 (6.25%) case after the 13th day of surgery. All these patients were managed conservatively and got resolved with time.
a) Showed z shaped incision and postoperative healed scar mark in axilla; b) Gross appearance of the bilateral healed scar mark in axilla; c&d) an elliptical incision showing yellowish white in colour tissue held in Allis forcep; e) Operative picture showing accessory tissue and gross appearance of the specimen; f) Skin closed with staples and drain in situ.
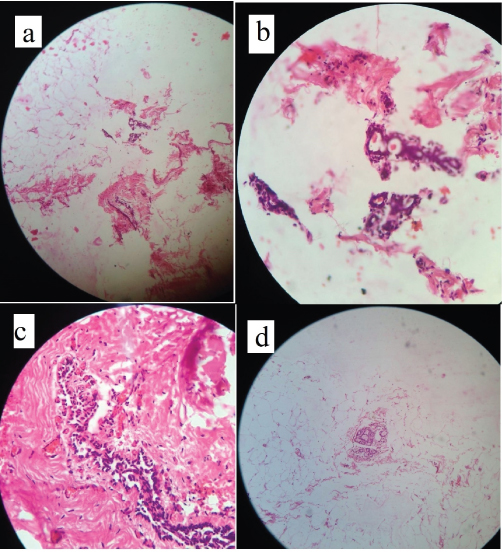
In case of axillary fibroadenoma, FNAC showed short staghorn pattern and myoepithelial cells in sheets, papillary structures and scattered singly. The smear showed bimodal population of benign duct epithelium and cells revealed mild nuclear pleomorphism. Background shows benign bare bipolar nuclei [Table/Fig-8a]. On histology of axillary fibroadenoma, it revealed presence of breast parenchyma in accessory breast lump and the ducts are lined by a bilayered epithelial and myoepithelial layer. The stroma was composed of spindle cells and shows myxoid changes at places [Table/Fig-8b,c]. On histopathology of the accessory breast, there were appearance of the mammary ducts and lobules embedded in fibrocollagenous adipose tissue stroma [Table/Fig-9a]. There was appearance of the benign breast tissue surrounded by fibrocollagenous stroma [Table/Fig-9b]. Other section shows mammary duct along with fibrocollagenous stroma and blood vessels on 100 X zoom H&E [Table/Fig-9c,d]. Other sections revealed normal appearance of the mammary ducts and lobules surrounded by adipose tissue on 40 x section. There were appearance of the benign breast tissue alongwith dilated blood vessels surrounded by fibrocollagenous & adipose tissue [Table/Fig-10a-c]. In excised specimen of the nipple, the histopathology revealed normal breast parenchyma in form of ducts, fibrotic stroma and adipose tissue. The ducts are lined by bilayered epithelial and myoepithelial layer (H & E, X 40) [Table/Fig-10d].
a) fine needle cytology showed fibromyxoid stroma and bare nuclei confirmed as accessory breast fibroadenoma (MGG; X- 100); b&c) histopathology showed a well defined tumour composed of ductular and stromal proliferation. The ducts are lined by a bilayered epithelial and myoepithelial layer (H & E x 100).
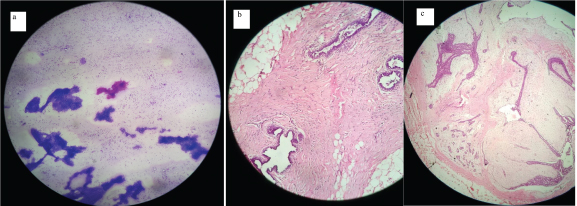
On histopathology – a - section shows mammary duct and lobules embedded in fibrocollagenous adipose tissue stroma {a) H & E 40 X; b&c) on 100 x zoom}; d) shows benign breast tissue surrounded by fibrocollagenous stroma and mammary duct (H & E 40 X).
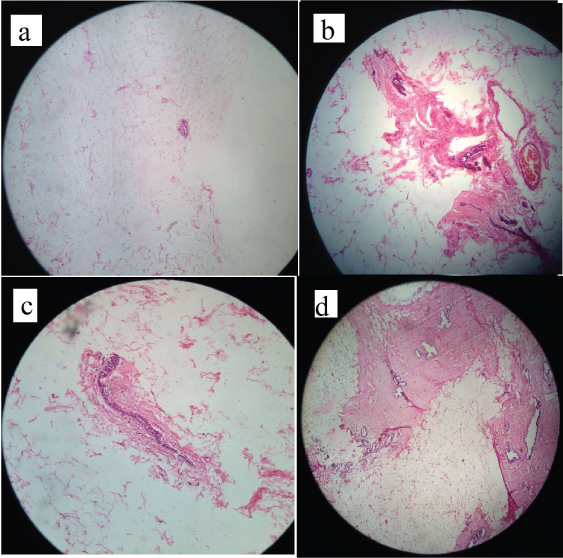
On histopathology a) section shows fibroadipose tissue along with focal area reveal benign breast lobules and ducts (H & E 40 x zoom); b & c) section reveal benign breast tissue along with dilated blood vessel (H & E 40 x zoom); d) Showing normal breast parenchyma in form of ducts, fibrotic stroma and adipose tissue. The ducts are lined by bilayered epithelial and myoepithelial layer (H & E x 40).
Postoperatively, patients were in followed up upto 6 to 8 months after 15 days. Patients were examined for the complications like residual disease, tenderness, lymphoedema, and contracture formation or any restriction in the limb movements at shoulder joint [Table/Fig-11]. In first month of follow-up, there was no collection, residual tissue or restriction of the arm or any discomfort. There was neither pain in the axillary or the breast area. Lymphoedema was seen in 2 cases after one month of the surgery which was treated conservatively. It was managed with the antibiotics, anti-inflammatory drugs, limb elevation and elastic crepe bandage. Suture line infection in the form of seroma was treated with antibiotics, regular dressings. Hypertrophic scar was seen in 2 cases, which were managed by giving intralesional steroids in 3 sittings. In rest of the cases, there were no complications was observed and did well.
Details of the postoperative complications.
| Complications | Number | Percent age (%) |
|---|
| Haematoma | 0 | 0 |
| Wound dehiscence | 3 | 9.37 |
| Contracture | 0 | 0 |
| Suture line infection | 2 | 6.25 |
| Residual swelling | 0 | 0 |
| Malignancy | 0 | 0 |
| Restriction in movements | 0 | 0 |
| Hypertrophy of the scar | 2 | 6.25 |
| Lymphoedema of the Arm | 2 | 6.25 |
| Nerve injury | 0 | 0 |
| Necrosis | 0 | 0 |
Discussion
The occurrence of more than two breasts as accessory or ectopic glandular tissue is known as polymastia which is the second most common form of supernumerary breast tissue. The incidence of Polymastia (supranumerary breasts) and polythelia (supranumerary nipples) is around 2-6% among the female population [6]. Accessory nipples are commonly seen as benign congenital anomaly which may be functional or non-functional [7]. In a study by Aydogan F, the ages of the patients at the time of surgery ranged from 19 to 54 years and mean age were 28.8 years [7]. Our study also showed similar results.
Patient complaints with cosmetic reasons, pain and swelling during menstruation, or milk secretion. Axillary breast tissue can be represented by ectopic tissue not connected to the breast. It may also be connected to the external part of thoracic breast (the axillary tail of Spence).
Accessory breasts found on the left side of the body are usually seen just below the inframammary crease. In 67% cases it is seen in the thoracic or abdominal portions of the milk line, another 20% in the axilla and the remaining occur anywhere along the milk line. It may enlarge during pregnancy or lactation because of its sensitivity to estrogen and its size can change during the menstrual period, as seen in our study. Aberrant or EBT has been reported to arise from extra sites, including the face, posterior neck, chest, buttock, vulva, hip, shoulder, posterior and/or lateral thigh, perineum, as well as the midback. EBT especially when found in the axilla is located in the subcutaneous tissue and deep dermis of the skin, were it often mingles with normal skin appendage glands [8].
There are rare diseases among the accessory breast as bilateral accessory breasts, axillary fibroadenoma, bilateral accessory nipple which are not commonly found; our study came across such rare entity (a rural center); 5 cases as bilateral; 16 cases as unilateral swelling in axilla; one rare case was of axillary fibroadenoma in female; 1 case as unilateral and 1 case as bilateral accessory nipple in males and 7 cases were unilateral and one case as bilateral accessory nipple in females.
Accessory mammary carcinoma is thought to account for 0.3–0.6% of all breast cancer cases, usually manifesting as an axillary mass [9]. It may be asymptomatic or associated with pain, decreased arm movement, cosmetic reasons or anxiety. It has been described that accessory or ectopic breast may occur with benign cystic changes, benign tumours (adenomas and fibroadenomas) and malignancy. Medullary breast cancer, cystosarcoma phylloides, extramammary Paget’s disease and papillary carcinoma have all been reported in accessory mammary tissue. The morbidity can occur in the form of intercostobrachial nerve damage, late healing, lymphoedema of the arm, which could be due to improper dissection in the axilla, as it is still unclear about the lymphatic drainage from ectopic breast tissue [10].
The most common condition in the accessory breast is breast carcinoma followed by mastopathy and fibroadenoma. There may be associated complications as urinary abnormalities such as supernumerary kidneys, failure of renal formation, renal adenocarcinoma, hydronephrosis, polycystic kidney disease, duplicate renal arteries and ureteric stenosis in relation to EBT cases, especially in polythelia patients. It can occur due to failure of development of mammary tissue and genitourinary system [11]. In the present study, no such associated abnormalities or any malignancy was found. In one case of accessory nipple, inflammation was present in the surrounding area of the areola. We also came across such rare entity diagnosed as axillary accessory breast fibroadenoma which was excised and followed up for 6 months without any recurrence. There were no palpable lymph nodes in the region.
Ultrasonography is useful tool and with the help of the real-time gray-scale and colour Doppler imaging, we can differentiate accessory breast tissue mass from other diseases. Sonography reveals a mass like abnormality and echogenic density that corresponds to that of the normal breast parenchyma. The differential diagnoses of an axillary mass are lipoma, lymphadenopathy or lymphadenitis, epidermal cyst, vascular malformation, fibroadenomas, schwannomas and malignancy [12].
On mammography, axillary accessory breast tissue appears to be normal glandular parenchyma which is located away from the breast, but in contradiction the axillary tail of Spence, which is a continuation of the breast tissue that leads into the axilla.
On MRI, accessory breast tissue can be seen as a subcutaneous ill-defined mass or a region that has signal intensity and contrast enhancement similar to the rest of the breast parenchyma but is discontinuous with the normal breast tissue [13]. In the present study, ultrasonography revealed fibro-fatty and fibrogladular tissue in all the cases. There were no features of carcinoma. In four cases, mammography was done as these cases had breast hypertrophy and nipple discharge. Mammography showed normal appearance of the breast without any malignant changes.
On histopathology of aberrant breast tissue, it may appear to have a typical stroma, lobules and ducts, but may be poorly structured [14]. We encountered a case where a cytopathological examination of the bilateral axillary masses revealed adenosis with fibrocystic changes. Therefore, the patient was managed with only a modified radical mastectomy on the left side, and an unnecessary right mastectomy could be avoided.
Excision is recommended prior to puberty or at any age when the condition is recognized and becomes a concern to the individual. The commonly reported complications after removal of accessory breast are incomplete removal, poor scar, intercostobrachial nerve injury and lymphedema of arm [10]. We recommend that either for the cosmetic reason or for the other lesion of the breast, accessory breast should be excised as early as diagnosed.
In our study, wound dehiscence occurred in three cases, 2 patients had suture line infection and two patients had oedema of the arm which was managed conservatively. There was also hypertrophy of the scar in two cases. In present study, there were no other complications like restriction in the movement of the arm, any contracture formation and cosmetically results were encouraging.
Another retrospective study found 16 patients diagnosed as unilateral; 13 patients as bilateral accessory breasts; of which 21 patients underwent excision of breast tissue, 5 had liposuction, and 3 had both. The authors conclude that in patients with concomitant macromastia, reduction mammaplasty and removal of accessory breasts can be performed at the same time with no additional morbidity. They found that excision, liposuction, or both showing satisfactory results [7]. It could also be removed for cosmetic purposes as in our study it was removed for cosmetic reason in 10 cases.
We did Z-plasty in 8 cases where swelling was large in size and it showed satisfactory outcomes. The direct excision allows proper excision but there may be chances of ugly scar and formation of dead space. The only drawback in liposuction is difficult to remove the fibro-glandular breast tissue resulting in incomplete dissection, thus leaving behind a visible core of breast tissue. The use of a microdebrider (powered shaving rotary device) is a potential solution to this problem for accessory breast tissue [15].
Another study did a unilateral reduction mammoplasty for supernumerary breast and rectified the breast asymmetry. The medial pedicle wise technique was used for en bloc resection of the ectopic breast, including the nipple-areola complex together with the upper outer breast quadrant [16]. They showed satisfactory results.
From the study results we recommend that self observation and clinical examination always play an important role in breast diseases for early detection and hence are the cornerstone. USG and FNAC are the diagnostic tools in BABD or to rule out malignancy. The choice of treatment is surgery for confirmatory diagnosis and cosmetic reasons. Liposuction can also be done but we do not recommend as with this technique, chances of incomplete dissection are there.
Conclusion
Accessory breasts occur more frequently in females, more commonly on the left side of the body. Unilateral accessory breasts are more common than bilateral polymastia. It remains a dilemma in asymptomatic cases without any nipple which present only as a swelling in the axilla. After evaluating a series of 32 cases in rural area, we recommend that there should be an awareness program regarding proper check-up for such axillary swellings. We found that majority of the cases reported for cosmetic reasons. Proper assessment of the disease gives relief to the patient from the discomfort and rules out the probability of malignancy.