Endoscopic Excision of Symptomatic Simple Bone Cyst at Skull Base
Prashant Gunawat1, Salman Tehran Shaikh2, Vikram Karmarkar3, Chandrashekhar Deopujari4, Nishit Shah5
1 Consultant Neurosurgeon, Department of Neurosurgery, Bombay Hospital Institute of Medical Sciences, Mumbai, Maharashtra, India.
2 Senior Resident, Department of Neurosurgery, Bombay Hospital Institute of Medical Sciences, Mumbai, Maharashtra, India.
3 Consultant Neurosurgeon, Department of Neurosurgery, Bombay Hospital Institute of Medical Sciences, Mumbai, Maharashtra, India.
4 Professor and Head of Department, Department of Neurosurgery, Bombay Hospital Institute of Medical Sciences, Mumbai, Maharashtra, India.
5 Consultant ENT Surgeon, Department of ENT, Bombay Hospital Institute of Medical Sciences, Mumbai, Maharashtra, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Salman Tehran Shaikh, V-1, Row House II, Sector 6, Vashi Navi, Mumbai-400703, Maharashtra, India.
E-mail: shaikhsalman25@gmail.com
Seizure is a classical feature of intra axial brain parenchymal lesion. Simple bone cyst is an unusual bony pathology at skull base presenting with unexpected symptoms of complex partial seizures. Skull base neuro-endoscopy has managed such lesions more effectively with reduced post-operative morbidity as compared to transcranial approach. This case report discusses a 20-year-old male who presented with 3 episodes of seizure over a time period of 10 months. MRI brain revealed T1 hypo and T2 hyper intense cystic lesion in middle cranial fossa with no enhancement on contrast administration. CT scan showed cystic lesion involving greater wing and pterygoid plate of sphenoid on left side. CT cisternographic evaluation showed CSF outpouching in the sphenoid air sinus. Excision of the cystic lesion was carried out through endoscopic transmaxillary transpterygoid approach. Histopathological examination showed the lesion to be a simple bone cyst.
Endoscopic transmaxillary transpterygoid approach, Seizure, Simple bone cyst, Unicameral
Case Report
A 20-year-old male was referred to Department of Neurosurgery for evaluation of 3 episodes of seizure over 10 months. His neurological examination, fundus examination, higher mental functions, sensory and motor examination of limbs were normal. He was started on Levetiracetam drug therapy (500 mg twice a day) as a symptomatic measure prior to investigations.
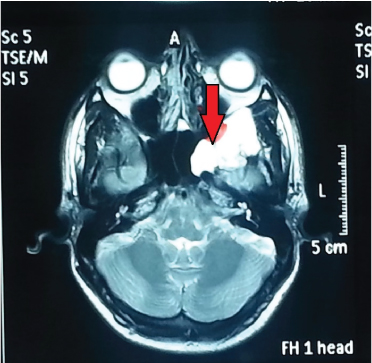
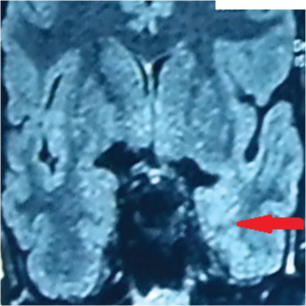
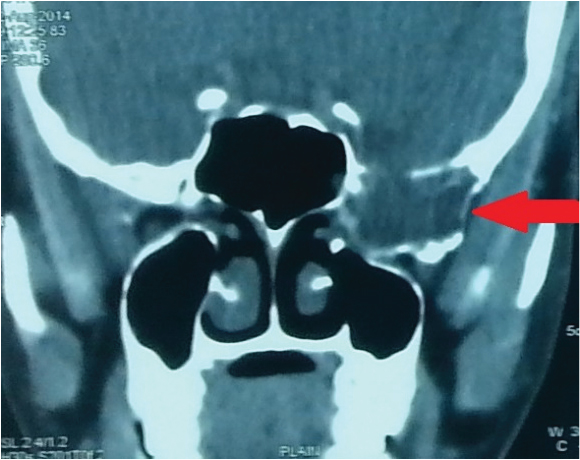
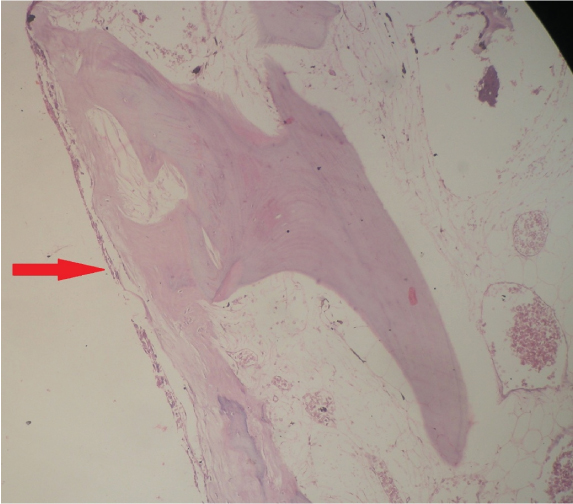
MRI brain revealed T1 hypo and T2 hyper intense cystic lesion in middle cranial fossa with no enhancement on contrast administration [Table/Fig-1,2]. CT scan showed a cystic lesion involving greater wing and pterygoid plate of sphenoid on left side [Table/Fig-3]. CT cisternographic evaluation had shown CSF outpouching in the sphenoid air sinus. We were unable to determine nature of lesion based on preoperative scans. Provisionally, diagnosis was suspected to be fibrous dysplasia eroding the bone and presenting as meningo encephalocele. Excision of the cystic lesion was carried out through endoscopic trans-maxillary trans-pterygoid approach. Intra operatively a cystic lesion involving pterygoid and greater wing of sphenoid was demonstrated. Small encephalocele was seen in the widened Foramen Rotundum. Repair of encephalocele was done using fat, free fascia and vascularized naso-septal flap. Histopathological examination was suggestive of a simple bone cyst [Table/Fig-4]. Patient had made good post-operative recovery and had no seizure episodes during the follow up period of 12 months. He was asked to continue Levetiracetam in the post-operative period for 6 months.
T2 weighted MRI image showing cystic hyper-intense lesion at skull base with no enhancement on administration of contrast.
FLAIR coronal image showing signal changes in left temporal lobe.
Non contrast CT coronal view showing erosion of greater wing of sphenoid bone.
icroscopic image showing thin fibrous cyst lining with haemosiderin pigments along the bone. (Haematoxylin-eosin stain 4X).
Discussion
Simple bone cyst (Unicameral bone cyst) was first described by Jaffe and Lichtenstein in 1943 [1]. Simple bone cysts are typically benign, fluid filled cystic lesion which can virtually affect any bone. Typical location for simple bony cyst is proximal humerus and proximal femur [2]. Though literature states that simple bone cyst can occur in the ends of long bones, rarely, if at all, do they occur at skull base [2]. Mode of presentation of simple bone cyst varies like an incidental finding, pain and swelling at involved site, seizure episodes or pathological fracture of involved site [3]. Radiologically it appears as a radiolucent lesion at the end of long bone. Magnetic Resonance Imaging (MRI) could be used to diagnose simple bone cyst at unusual location like skull base. On MRI it may appear as a fluid filled lesion isointense on T1 and hyperintense on T2 weighted images. The alternative differential diagnosis based on clinical and radiological features is aneurysmal bone cyst. Based on MRI aneurysmal bone cysts are expansile, lytic, eccentric showing septations and a double density [4]. Treatment of simple bone cyst is not uniformly followed. Different techniques such as percutenous injection of steroids and autologous bone graft, open curettage and grafting, minimal invasive instrumentation have been studied with good results [5,6].
This patient presented for evaluation of seizures and MR imaging showed a cystic lesion at skull base involving pterygoid plate of sphenoid bone. Extent of this bony lesion was clearly demonstrated on CT scan. FLAIR MR Images showed signal intensity changes in medial temporal lobe adjacent to the lesion. It is uncommon for bony skull base lesion to present with seizures as the primary symptom. Cause of seizure in this patient may be attributed to erosion of bone at the base and herniation of brain parenchyma through a small encephalocele.
Extended endoscopic approach and temporal zygomatic craniotomy wide skull base approach were the treatment modalities in contention. Para-median skull base location and cystic nature of lesion were two important factors favouring endoscopic surgery rather than transcranial skull base approach. Endoscopic approach allows us to reduce the encephalocele, plug the dural defect and repair the skull bone in a single procedure without interfering with brain parenchyma [7]. Transnasal extended endoscopic approach for lesion at the ventral skull base is gaining wide acceptance in neurosurgery [8]. We decided to approach this lesion with transnasal transmaxillary transpterygoid approach rather than cranial approach [9] to avoid extensive skull base dissection, brain retraction and difficult skull base reconstruction which if failed may have led to a very debilitating CSF fistula.
Conclusion
Simple bone cyst is a rare occurrence at skull base which can be managed with a less invasive endoscopic procedure effectively. This case report stands distinct for the unusual presentation i.e. seizure and unusual location i.e. skull base of this pathology and the effectiveness of endoscopic approach in such cases.
Conflict of Interest
The author(s) declare(s) that there is no conflict of interests regarding the publication of this paper.
[1]. Jaffe HL, Lichtenstein L, Solitary bone cyst with emphasis on the roentgen picture, the pathologic appearance and the pathogenesisArch Surg 1942 44:1004-25. [Google Scholar]
[2]. Wilkins RM, Unicameral bone cystsJ Am Acad Orthop Surg 2000 8(4):217-24. [Google Scholar]
[3]. Pretell-Mazzini J, Murphy RF, Kushare I, Dormans JP, Unicameral bone cysts: General characteristics and management controversiesJ Am Acad Orthop Surg 2014 22(5):295-303. [Google Scholar]
[4]. Sullivan RJ, Meyer JS, Dormans JP, Davidson RS, Diagnosing aneurysmal andUnicameral bone cysts with magnetic resonance imagingClin Orthop Relat Res 1999 366:186-90. [Google Scholar]
[5]. Kadhim M, Thacker M, Kadhim A, Holmes L Jr, Treatment of unicameral bone cyst: systematic review and meta-analysisJ Child Orthop 2014 8(2):171-91. [Google Scholar]
[6]. Hou HY, Wu K, Wang CT, Chang SM, Lin WH, Yang RS, Treatment of unicameral bone cyst: a comparative study of selected techniquesJ Bone Joint Surg Am 2010 92(4):855-62. [Google Scholar]
[7]. Yildirim AE, Ekici I, Cagil E, Divanlioglu D, Belen AD, Pure endoscopic endonasal removal of unusual anterior skull base aneursymal bone cyst extending to the frontal lobeJ Craniofac Surg 2015 26(3):e232-34. [Google Scholar]
[8]. Salmasi V, Blitz AM, Ishii M, Gallia GL, Expanded endonasal endoscopic approach for resection of a large skull base aneurysmal bone cyst in a pediatric patient with extensive cranial fibrous dysplasiaChilds Nerv Syst 2011 27(4):649-56. [Google Scholar]
[9]. Wasano K, Yamamoto S, Tomisato S, Kawasaki T, Ogawa K, Modified endoscopic transnasal-transmaxillary-transpterygoid approach to parapharyngeal space tumor resectionHead Neck 2016 38(6):933-38. [Google Scholar]