Evaluation of Hospitalized Intractable Epileptic Children with SPECT Scan in Ahvaz, South West of Iran
Ali Akbar Momen1, Faramarz Ahmadi2, Arash Malekian3, Hannaneh Davoodzadeh4, Hossein Kabirinia5
1 Pediatric Neurologist, Department of Pediatrics, Golestan Hospital, Ahvaz Jundishapour University of Medical Sciences, Ahvaz, Iran.
2 Nuclear Medicine Specialist, Department of Nuclear Medicine, Golestan Hospital, Ahvaz Jundishapour University of Medical sciences, Ahvaz, Iran.
3 Neonatologist, Department of Pediatrics, Golestan Hospital, Ahvaz Jundishapour University of Medical Sciences, Ahvaz, Iran.
4 Faculty, Department of Anesthesiology, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran and Clinical Research Development Unite, Golestan Hospital, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Iran.
5 General Practitioner, Clinical Research Development Center, Golestan Hospital, Ahvaz Jundishapour University of Medical Sciences, Ahvaz, Iran.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Ali Akbar Momen, Pediatric Neurologist, Department of Pediatrics, Golestan Hospital, Ahvaz Jundishapur University of Medical Sciences, Ahvaz, Postal code: 61357-15794, Iran.
E-mail: momen_ali@yahoo.com
Introduction
Seizures are the most frequent neurologic disorder seen in childhood. Epilepsy is a group of disorders that includes an abnormally increased susceptibility to seizures.
Aim
To examine the effectiveness of SPECT (Single Photon Emission Computerized Tomography) in detecting seizure foci in 21 Iranian children who had medically refractory epilepsy.
Materials and Methods
Children between 2 to 15 years of age with uncontrolled seizures were investigated using SPECT scan as a standardized protocol.
Results
In 16 cases (76.2%), likely seizure foci were evident, as were seen in the form of decreased regional blood flow, while in 5 cases (23.8%), SPECT scan results were normal. Left temporal lobe was the most common area which had decreased regional blood flow.
Conclusion
SPECT scan can potentially be used to investigate children with uncontrolled seizures.
Electroencephalography, Seizure, 99mTc-ECD radionuclide
Introduction
Seizure disorders are the most frequent neurologic disorders seen in childhood [1,2]. Epilepsy is a group of disorders that include an abnormally increased susceptibility to seizures [3]. A positive history of at least one seizure, along with a predisposition, is required to establish the presence of epilepsy. According to new definitions, changes in EEG (Electroencephalography) patterns alone are not enough to determine epilepsy [4].
Researches show that 4 to 10% of children, will suffer at least one seizure before 16 years of age. Children in the ages of less than 3 years, show higher rates of this problem as compared to others. Approximately 150,000 children endure an initial unprovoked seizure per year and 20% of them develop epilepsy [5]. Anti-Epileptic Drugs (AEDs) are often used to manage epilepsy; however, in approximately 20%-30% of patients, seizures are not controlled. Refractory epilepsy is defined as a failure in controlling seizures after the use of two properly chosen and tolerated AED regimens (as monotherapy or polytherapy) [6,7].
Diagnostic criteria and management play an important role in childhood epilepsy outcomes. The use of epilepsy surgery for treatment of refractory seizures is widespread. Evidence indicates that the benefit of surgery depends on how early surgery is performed after the diagnosis [2,8]. The first step in managing such patients is to obtain an accurate seizure history and a clinical examination [9]. Paraclinical procedures are used as the next step in its management. Ictal Electroencephalograms (EEGs) are used in detecting seizure foci; however their accuracy rates are only 40%-70%. Other diagnostic techniques are also used in detecting the sources of seizures, such as Computerized Tomography scan (CT scan) and Magnetic Resonance Imaging (MRI), but they also are not reliable in determining the extents of the epileptogenic zones [10,11].
The gold standard which can be used for detecting the seizure foci is the use of intracranial EEGs, which is difficult, expensive and invasive. Single Photon Emission Computed Tomography (SPECT) is an effective and non-invasive procedure that has been shown to be safe in children [12]. Furthermore, research has shown that when used with MRI, it could have a sensitivity rate of 90%. In this technique, the increase or decrease of cerebral blood flow in affected areas can be detected [10,13].
As a result, if appropriate candidates can be found, their quality of life can be improved with epilepsy surgery and long term costs of treatment can be decreased. On the other hand, by determining positive predictive values in SPECT scans, the efficacy of nuclear medicine and its interaction with other wards can be measured. The main objective of this study was to examine the effectiveness of SPECT in detecting seizure foci in children with medically refractory epilepsy among patients of Golestan hospital in Ahvaz, south west of Iran.
Materials and Methods
After obtaining ethical approval from Ahvaz Jundishapur University of Medical Sciences study was performed in Ahvaz Golestan hospital. Patients suffering from uncontrolled seizures despite taking anticonvulsants, were selected and SPECT scan was performed. After obtaining a detailed history and after physical examination, a questionnaire was completed by these patients. Then seizure symptoms, family history, prior history of disease, type of antiepileptic medication used, number of seizures per day and the duration of affecting to seizure disorder were answered by the parents in charge. Patients were examined and radioisotope of 99mTc-ethyl cysteinate dimer (99mTc-ECD 99mTc-ECD) was injected intravenously for brain imaging between seizures. The amount of substance absorbed is in proportion to cerebral blood flow. Brain uptake rate is 4.9%-6% of substance injection level. This substance reaches its maximum concentration within 5 minutes. Upto 20-40 mCi of this substance can be injected in adults. The amount of intravenous radioisotope for children was calculated by the formula:

In this formula "A" is an adult dose, equal to 20-40 mCi and "X" stands for the child’s age by years. Injection of the radioisotope agent in patients was done in a dark quiet environment without noise and without pain, while the patient’s eyes were completely closed, in order to prevent the stimulation of a specific sense which could cause increased blood flow in the cerebral cortex, which was associated in that sense. Then, imaging with gamma Siemens e-cam was done half an hour after 99mTc-ECD injection. After imaging, the data was computer recorded and evaluated by nuclear medicine specialists. The information derived from patients’ forms and nuclear medicine specialists’ reports in this descriptive study were analyzed by SPSS version 13.
Results
In this study, 21 patients suffering from uncontrolled seizures despite treatment with antiepileptic drugs, were selected. The mean age of the patients was 7 years and three months. The age range was 2 to15 years old. Sixteen participants were males (76.2%) and 5 (23.8%) were females [Table/Fig-1].
Patients characterizations.
| N | Characteristics |
|---|
| Patient’s Age (year) | Min | 2 |
| Average | 7.3 |
| Max | 15 |
| Parent’s Age (year) | Fathers | Min | 21 |
| Average | 32 |
| Max | 42 |
| Mothers | Min | 16 |
| Average | 25 |
| Max | 38 |
| Birth Weight (gr) | Min | 2000 |
| Average | 3087 |
| Max | 3700 |
| 21 | Gender | Male | 16 |
| Female | 5 |
| 21 | Age birth | Full term | 20 |
| Post term | 1 |
| 21 | Oxygenation during birth | Without Hypoxia | 17 |
| Hypoxia | 4 |
| 21 | Jaundice | Positive | 2 |
| Negative | 19 |
| 21 | Dominate Hand | Right | 17 |
| Left | 4 |
In present study, there was no significant correlation between birth weight and the occurrence of seizures (p=0.2). Two of the participants had Hyperbilirubinemia. The only participant with a birth weight under 2000 grams had an onset of hyperbilirubinemia on the third day of birth, that was successfully treated with phototherapy after 7 days. This patient had a normal MRI report but he showed a decreased blood flow in the right temporal lobe in the SPECT scan study.
In terms of gestational age at the time of birth, all were full term babies and only one participant was post-term. The child born post-term was delivered through a normal vaginal delivery and acquired a low Apgar score. MRI study of the patient’s brain revealed encephalomalacia of the right brain hemisphere. The patient’s right parieto-temporal lobe showed decreased perfusion in SPECT scan and it is possible that seizures and lesions seen in MRI may be due to insults surrounding the time of birth. Finally, our study did not show a statistically significant difference between gestational age and type of seizures or the occurrence of seizures in participants (p=0.4). Also, significant correlation between brain SPECT scan findings, brain MRI findings and the number of seizures per day was not seen (p=0.5). The average length of time from the diagnosis of seizures to the referral for SPECT scan, was 3.6 years with a minimum of 0.3 years and a maximum of 11 years. The maximum number of daily seizures was 12 and the minimum number was 2. However, a majority (10 participants) had 2-3 seizures per day. Distribution of positive family history is shown in [Table/Fig-2]; and distribution of abnormal EEG in patients with intractable epilepsy is shown in [Table/Fig-3]. [Table/Fig-4] shows that most of our patients had generalized tonic-clonic type seizures.
Frequency distribution of positive family history in patients with uncontrolled seizures studied by SPECT scan referred to Ahvaz Golestan Hospital.
| Family History | Number (Percent) |
|---|
| Immediate | 3(14.3%) |
| Second relatives | 4(19%) |
| Third relatives | 1(4.8%) |
| No family history | 13(61.9%) |
| Total | 21(100%) |
Distribution of number of abnormal EEG in patients with intractable epilepsy studied with SPECT scan referred to Ahvaz Golestan Hospital.
| EEG | Number (Percent) |
|---|
| Normal | 6(28.6%) |
| Mildly abnormal | 5(23.8%) |
| Moderately abnormal | 10(47.6%) |
| Total | 21(100%) |
Distribution of seizure types in patients with intractable epilepsy referred to Ahvaz Golestan Hospital.
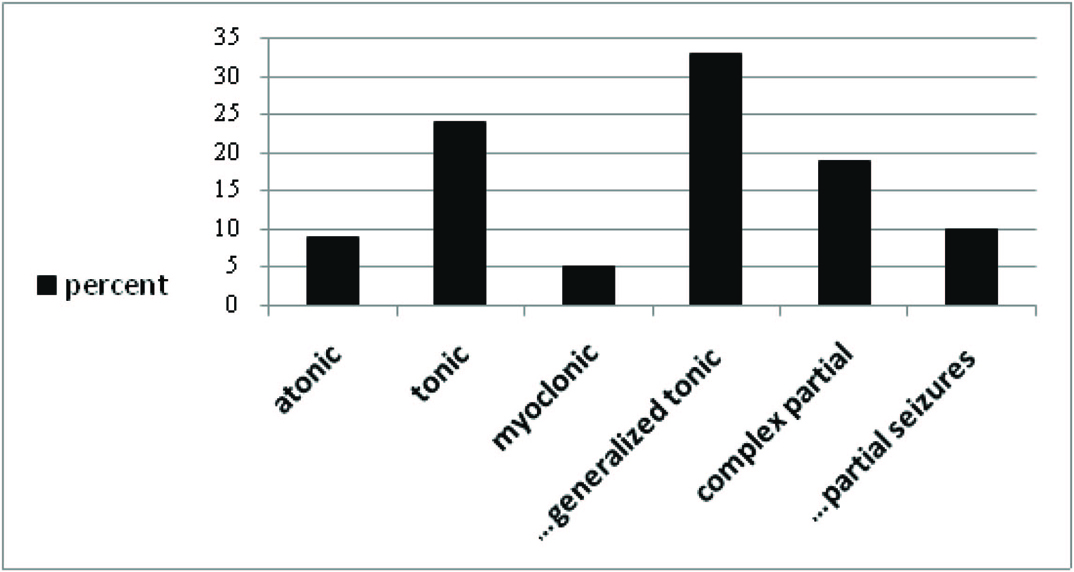
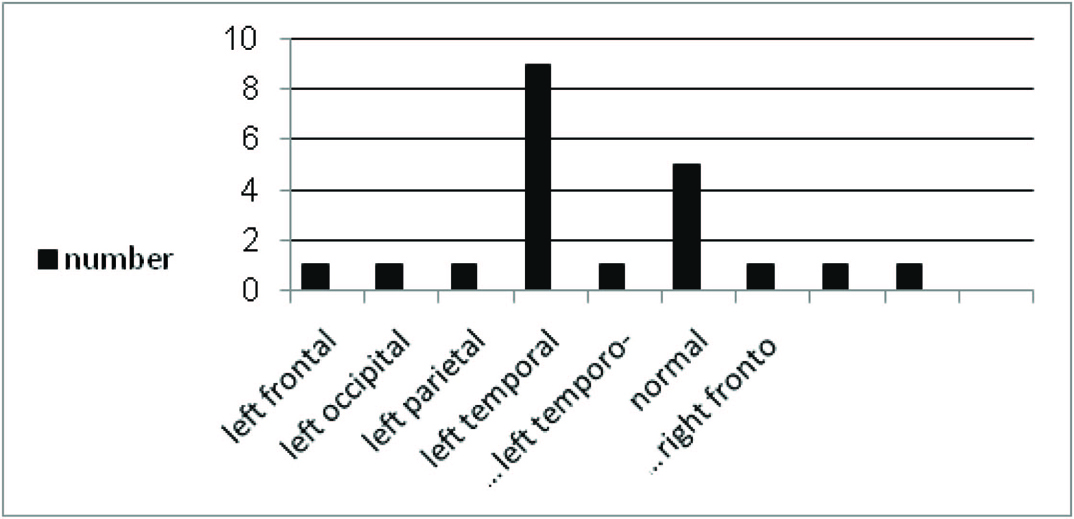
[Table/Fig-5] shows, the results obtained in patients’ SPECT scan. Among 21 patients who underwent SPECT scan, 16 (76.2%) were abnormal and 5 (23.8%) were normal. As seen in [Table/Fig-5], nine cases showed decreased perfusion of the left temporal lobes and the other cases showed reduced perfusion in other lobes. EEGs of 6 patients were normal and those of 15 were abnormal, of among these, 10 had moderate abnormalities and 5 had mild abnormalities. A significant difference was not seen between EEG abnormalities and SPECT findings (p=0.6) [Table/Fig-3]. Of the patients studied, 12 used three anticonvulsants, 4 used 4 anticonvulsant drugs and 2 participants used 2 anticonvulsant drugs to control seizures. All patients used at least one or two new drugs.
Frequency of decreased brain lobe perfusion in SPECT scan of patients with intractable epilepsy referred to Ahvaz Golestan Hospital.
Discussion
In this study, 21 patients suffering from intractable epilepsy, unresponsive to regular and new antiepileptic drug regimens, were included. Our study did not show a statistically significant difference between gestational age and type of seizures or the occurrence of seizures in participants (p=0.4). Whereas, in a study by Sheth et al., a relationship between gestational age and seizure incidence was seen [14]. Sun et al., also showed a correlation between gestational age and the occurrence of seizures [15].
Children with intrauterine growth retardation are more likely to suffer from birth injuries and decreased blood and oxygen supply to the brain, before and during birth, due to placental blood supply disorders [16]. As seen in Sun et al., study done in Denmark, low birth weight and intrauterine growth retardation were risk factors for the increase of seizure incidence [15]. However, in our study, a significant correlation was not seen between birth weight and the occurrence of seizures (p=0.2).
Although the chance of an existing lesion in partial seizures is more likely, in our study, a significant correlation was not seen between MRI findings and seizure types. Also, in our study, most cases of positive SPECT scan had temporal lobe seizures and a clear relationship was not found between seizure and SPECT findings. (p=0.7). The main part of our study was aimed at the results obtained from SPECT scan evaluation of the studied patients. In general, SPECT imaging is used during and between seizures. In ictal SPECT scans increased cerebral blood flow and in interictal SPECT scans decreased blood flow, were seen. The purpose of doing interictal SPECT scan was to identify the seizure foci before surgery.
In a study done by Kalarickal J. Oommen et al., which included 42 patients, 90% of the participants who underwent interictal SPECT scan showed focal temporal hypoperfusion and 65% of participants who underwent periictal SPECT scan showed focal hyperperfusion [17]. Another study also showed that ictal SPECT could find localized cortical hyperperfusion in 72% of participants [18]. In Robert C. Knowlton et al., study surgery outcome was compared to diagnostic imaging techniques in 160 patients [13]. This study found that in 27 patients who used three imaging techniques Magnetic Source Imaging (MSI), Positron Emission Tomography (PET) and Ictal SPECT) Ictal SPECT showed the highest overall diagnostic and predictive value. However, when the techniques were used separately in patients, all of them seemed to have similar diagnostic values [19]. In a study done by Sang Kun Lee and colleagues in Korea, ictal SPECT scan correctly located the epileptogenic lobe in 58.9% patients and it was found to be more valuable than other methods in locating temporo-occipital lobe seizure foci [20]. In 2001, Wright NB, reviewed 30 articles, in which the results of SPECT on different stages of seizures and between seizures were evaluated. The results of these articles showed that the sensitivity of interictal SPECT in finding the seizure foci in patients with refractory seizures was approximately 44% [21]. In another study done by Hyangwoon lee et al., on 61 patients aged 1 to 48-year-old, interictal SPECT was found to be positive in 68.9% of the cases [22].
In our study, interictal SPECT scan was performed. Of the 21 patients included in our study, 16 had abnormal and 5 had normal SPECT scan results. Therefore, positive predictive value was 76.2%, which was higher in comparison to values found in previously mentioned studies. Research performed at this center included more positive cases, which may be due to improved sample selection, the type of substance used in SPECT imaging and greater accuracy in recording and analysis of images.
Limitation
A limitation of our study was the small sample group. Analytical results and the sensitivity of interictal SPECT scan can only be obtained if surgery is performed in the affected lobe and the seizure foci are removed, to consider the control of seizure.
Conclusion
SPECT scan is a useful method which can be used in detecting seizure foci in evaluation of intractable epileptic children. It is also a helpful guide which can be used for investigating epileptic foci in lesionectomies done by pediatric neurosurgeons More research done on higher sample sizes can document the importance of this method and we suggest that other researchers use this method to improve our result.
[1]. Bechtel N, Weber P, Attention problems in children with epilepsy. How is the long-term outcome?European Journal of Paediatric Neurology 2015 19(3):383-85. [Google Scholar]
[2]. Wheless JW, Clarke DF, Arzimanoglou A, Carpenter D, Treatment of pediatric epilepsy: European expertEpileptic Disord 2007 9(4):353 [Google Scholar]
[3]. Stafstrom CE, Carmant L, Seizures and Epilepsy: An overview for neuroscientistscold spring harbor Perspectives in Medicine 2015 5(6):a022426 [Google Scholar]
[4]. Fisher RS, Boas WvE, Blume W, Elger C, Genton P, Lee P, Epileptic seizures and epilepsy: definitions proposed by the International League Against Epilepsy (ILAE) and the International Bureau for Epilepsy (IBE)Epilepsia 2005 46(4):470-72. [Google Scholar]
[5]. Friedman MJ, Sharieff GQ, Seizures in childrenPediatric Clinics of North America 2006 53(2):257-77. [Google Scholar]
[6]. Mani J, Combination therapy in epilepsy: what, when, how and what not!The Journal of the Association of Physicians of India 2013 61(8 Suppl):40-44. [Google Scholar]
[7]. Kwan P, Arzimanoglou A, Berg AT, Brodie MJ, Allen Hauser W, Mathern G, Definition of drug resistant epilepsy: consensus proposal by the ad hoc Task Force of the ILAE Commission on Therapeutic StrategiesEpilepsia 2010 51(6):1069-77. [Google Scholar]
[8]. Chugani HT, Ilyas M, Kumar A, Juhász C, Kupsky WJ, Sood S, Surgical treatment for refractory epileptic spasms: The Detroit seriesEpilepsia 2015 56(12):1941-49. [Google Scholar]
[9]. Tolaymat A, Nayak A, Geyer JD, Geyer SK, Carney PR, Diagnosis and management of childhood epilepsyCurrent Problems in Pediatric and Adolescent Health Care 2015 45(1):03-17. [Google Scholar]
[10]. Kaminska A, Chiron C, Ville D, Dellatolas G, Hollo A, Cieuta C, Ictal SPECT in children with epilepsy: comparison with intracranial EEG and relation to postsurgical outcomeBrain 2003 126(1):248-60. [Google Scholar]
[11]. De Vos M, Vergult A, De Lathauwer L, De Clercq W, Van Huffel S, Dupont P, Canonical decomposition of ictal scalp EEG reliably detects the seizure onset zoneNeuroImage 2007 37(3):844-54. [Google Scholar]
[12]. Lascano AM, Perneger T, Vulliemoz S, Spinelli L, Garibotto V, Korff CM, Yield of MRI, high-density electric source imaging (HD-ESI), SPECT and PET in epilepsy surgery candidatesClinical Neurophysiology 2016 127(1):150-55. [Google Scholar]
[13]. Knowlton RC, The role of FDG-PET, ictal SPECT, and MEG in the epilepsy surgery evaluationEpilepsy & Behavior 2006 8(1):91-101. [Google Scholar]
[14]. Sheth RD, Hobbs GR, Mullett M, Neonatal seizures: incidence, onset, and etiology by gestational ageJournal of Perinatology: Official Journal of the California Perinatal Association 1999 19(1):40-3. [Google Scholar]
[15]. Sun Y, Vestergaard M, Pedersen CB, Christensen J, Basso O, Olsen J, Gestational age, birth weight, intrauterine growth, and the risk of epilepsyAmerican Journal of Epidemiology 2008 167(3):262-70. [Google Scholar]
[16]. Knowlton RC, Elgavish RA, Bartolucci A, Ojha B, Limdi N, Blount J, Functional imaging: II. Prediction of epilepsy surgery outcomeAnnals of neurology 2008 64(1):35-41. [Google Scholar]
[17]. Oommen KJ, Saba S, Oommen JA, Francel PC, Arnold CD, Wilson DA, The relative localizing value of interictal and immediate postictal SPECT in seizures of temporal lobe originJournal of Nuclear Medicine 2004 45(12):2021-25. [Google Scholar]
[18]. Krsek P, Kudr M, Jahodova A, Komarek V, Maton B, Malone S, Localizing value of ictal SPECT is comparable to MRI and EEG in children with focal cortical dysplasiaEpilepsia 2013 54(2):351-58. [Google Scholar]
[19]. Fang S, Management of preterm infants with intrauterine growth restrictionEarly Human Development 2005 81(11):889-900. [Google Scholar]
[20]. Lee SK, Lee S-Y, Yun C-H, Lee H-Y, Lee J-S, Lee D-S, Ictal SPECT in neocortical epilepsies: clinical usefulness and factors affecting the pattern of hyperperfusionNeuroradiology 2006 48(9):678-84. [Google Scholar]
[21]. Wright N, Imaging in epilepsy: a paediatric perspectiveThe British Journal of Radiology 2001 74(883):575-89. [Google Scholar]
[22]. Lee HW, Hong SB, Tae WS, Opposite ictal perfusion patterns of subtracted SPECTBrain 2000 123(10):2150-59. [Google Scholar]