The removal of impacted teeth is one of the most common procedures performed by Oral and Maxillofacial Surgeons [1]. This procedure is generally accompanied by post-operative side effects such as pain, swelling and trismus. Reduction of discomfort post-operatively and efficient local anaesthesia are imperative for success in surgical practice. Lignocaine 2% with adrenaline 1:100,000 is regarded as the standard to which all local anaesthetics are compared. Multimodal (balanced) analgesia is a recent approach to pain management strategy, in which more than one agent or class of agents at low doses is used, thereby reducing adverse effects and achieving better pain relief through multiple mechanisms.
Various adjuvants to local anaesthetics have been used to prolong the duration of analgesia. These include non-steroidal anti-inflammatory agents, opioid analgesics, alpha-2-adrenergic agents and ketamine. Ketamine is a well-known general anaesthetic, short-acting intra-operative analgesic and anti-inflammatory agent that has been in use for over four decades. However emergence delirium, hypertension, tachycardia were limitations for its use [2]. It is clear that high-dose ketamine acts as an intravenous general anaesthetic and that low-dose ketamine acts as an analgesic [3].
At small doses (0.1-0.5 mg/kg), ketamine has a noticeable analgesic action, which can be used to supplement local anaesthesia with minimal side effects. A number of studies have suggested that administration of ketamine before the noxious stimuli occurs is even more efficacious. This effect is referred to as pre-emptive analgesia [4].
The proposed study was designed to assess the clinical efficacy of sub-anaesthetic ketamine as an adjunct to local anaesthesia for the relief or prevention of post-operative pain, swelling and trismus after surgical removal of impacted mandibular third molars.
Materials and Methods
A total of 25 patients (13 male and 12 female) reporting to the Department of Oral and Maxillofacial Surgery, Bharati Vidyapeeth Deemed University Dental College and Hospital, Katraj, Pune between November 2014 and October 2015 with asymptomatic bilaterally symmetrical impacted mandibular third molars requiring surgical removal under local anaesthesia were included in the split mouth prospective controlled clinical study.
The inclusion criteria were patients aged between 18-50years of age irrespective of gender with bilaterally symmetrical impacted mandibular third molars confirmed by panoramic radiograph (Representative OPG- [Table/Fig-1]). Patients were clinically evaluated prior to selection, to rule out presence of infection and subsequently radiographically evaluated with an OPG to ensure the impacted mandibular 3rd molars were bilaterally symmetrical. The molars had the same angulation/spatial relationship and the same difficulty of operative procedure based on the pederson difficulty index [5]. The patients selected were classified as American Society of Anaesthesiologist (ASA) Physical Status 1 [6] and were non-smokers.
The exclusion criteria were patients with poor vital sign stability (hypoxia, hypotension, hypertension, heart rate, respiratory rate), patients with known drug allergies to ketamine or any of the medications used in the study, subjects with known systemic diseases namely untreated hypertension, severe cardiac failure, glaucoma, hyperthyroidism, raised intracranial pressure, neurotic traits or psychiatric illness or those with a history of cerebrovascular accident. Pregnant or lactating mothers were excluded from the study. Individuals under intoxication of alcohol or on drug therapy which may interfere with wound healing were also excluded.
All the selected patients were informed and explained about the experimental nature of the study, the possible complications and their co-operation solicited. An informed written consent along with additional documentation required for research and/or academic purposes was obtained from all the patients. The study protocol was reviewed and approved by the institutional review board.
The patients had bilaterally symmetrical impacted mandibular third molars which were removed at an interval of 15 days. The face of each patient was painted with povidone iodine solution and standard draping was done using sterile drapes. Intraoral preparation was done with povidone iodine solution. Anaesthesia was secured through inferior alveolar nerve block, lingual nerve block and long buccal nerve block techniques. Neither pre-medication nor topical anaesthetic was given to the patients before, during or after surgery. A standard Terrance Ward incision was placed and a full thickness mucoperiosteal flap was reflected to expose the site of the impacted tooth. Bone removal was carried out with a straight fissure bur by removing a gutter of bone around the tooth leaving buccal cortical plate intact. Odontomy was performed whenever necessary to facilitate tooth removal. After an adequate amount of bone was removed, the tooth was delivered from the socket by using an elevator. Sharp bony edges were smoothened with a bone file and the socket was irrigated with povidone iodine and saline to remove debris. Complete haemostasis was achieved before wound closure. Wound was closed with 3-0 silk suture (Mersilk 3–0, Johnson & Johnson Ltd., Aurangabad, India) using a simple interrupted suture technique and every patient was given the same set of post-operative instructions and medication. (Cap. Amoxicillin 500 mg TID for 5 days and Tab. Diclofenac Sodium 50 mg + Paracetamol 400 mg TID for 3 days).
The third molar sites of all patients enrolled in the trial were randomly assigned into 2 groups: Local Anaesthesia (Lignocaine) Alone (LAA) and Local Anaesthesia plus Ketamine (LAK). Five ml of local anaesthetic (Lignocaine Hydrochloride 2% with epinephrine 1:100,000) was injected in the ‘LAA’ group while the ‘LAK’ group received 5ml of local anaesthetic plus 0.2mg/kg ketamine. Patients were blinded to the solution used and the operator recorded the group (LAA or LAK) and the respective site (right or left) for analysis. Procedures were performed by a single surgeon to avoid bias.
The patients’ participating in the clinical study were explained the Visual Analog Scale (VAS) proforma pre-operatively. After surgery, the patients were asked to score overall pain on a 10-point VAS: 0-no pain; 10-excessive pain) at 1, 2 and 7 days after surgery. All side effects occurring during the procedure and during the 24-hour post-operative period were recorded.
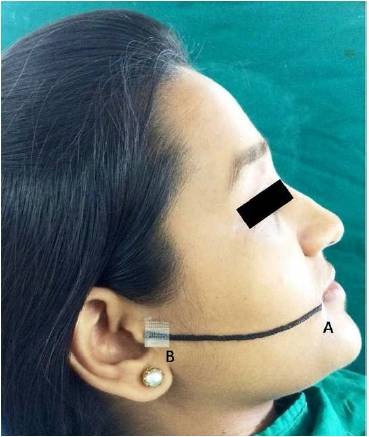
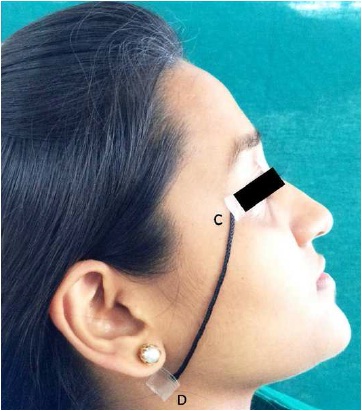
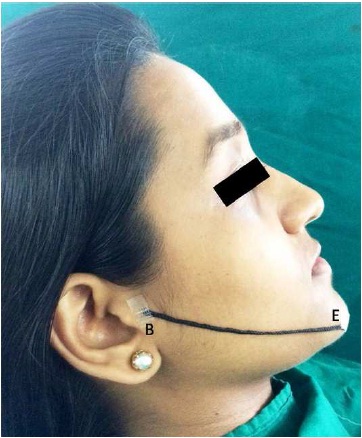
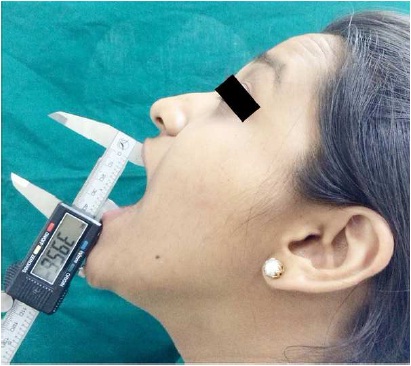
The level of facial swelling was determined by a modification of the tape-measure method described by Gabka and Matsumara [7] as depicted in [Table/Fig-2,3 and 4]. Pre-operatively, and on the 1st, 2nd and 7th day post-operative day, 3 measurements were made between 5 reference points: tragus (B), soft tissue pogonion (E), lateral corner of the eye (C), angle of the mandible (D), and outer corner of the mouth (A). The sum of the 3 pre-operative measurements was considered to be the baseline for that side of the face. The difference between each post-operative measurement and the respective baseline value indicated the extent of facial swelling on that day. Baseline mouth opening was evaluated pre-operatively while the degree of trismus was assessed on the 1st, 2nd and 7th post-operative day by measuring the distance between the mesio-incisal corners of the upper and lower right central incisors at maximum opening of the jaws as depicted in representative [Table/Fig-5]. The difference between the respective post-operative and pre-operative measurements indicated the degree of trismus on that day.
Orthopantomograph (OPG) representative of bilaterally symmetrical impacted mandibular 3rd molars.

Demonstrates how degree of swelling was assessed, A- outer corner of the mouth; B-Tragus of ear.
Demonstrates how degree of swelling was assessed, C- lateral corner of the eye; D- angle of the mandible.
Demonstrates how degree of swelling was assessed, E- soft tissue pogonion; A- outer corner of the mouth.
Depicts how mouth opening was measured using a vernier caliper.
The statistical significance of difference of qualitative characteristics between two study groups (inter-group comparison) was tested using Chi-square test. The statistical significance of difference of several quantitative variables across two study groups (inter-group comparisons) was tested using independent sample t-test after confirming the underlying normality assumption. The pre-op and post-op differences in each group (intra-group comparisons) were done using paired t-test after confirming the underlying normality assumption of pre-op and post-op difference of the variables studied. The significance level was set at p less than 0.05.
Results
Twenty-five patients with a mean age of 31 years (age range 18 to 50 years) and bilaterally symmetrical impacted mandibular third molars as confirmed by a panoramic radiograph were enrolled in the study.
Pain: Pain scores were highest during 1st post-operative day in both LAA and LAK group and gradually decreased on 2nd and 7th day. The scores on the VAS at 1st and 2nd post-operative days after surgery were significantly higher in the LAA group than in the LAK group (p-value<0.05). [Table/Fig-6] shows the inter-group comparison of pain score.
The inter-group comparison of pain score.
| Pain Score | Lignocaine(n=25) | Lignocaine + Ketamine(n=25) | Inter Group Comparisons(p-value*) |
|---|
| Day 1 | 6.0 ± 1.6 | 4.4 ± 1.3 | 0.001 |
| Day 2 | 4.2 ± 1.7 | 2.7 ± 1.7 | 0.004 |
| Day 7 | 1.0 ± 0.7 | 0.8 ± 0.6 | 0.462 |
Values are Mean ± Standard Deviation.
*p-values by independent sample t-test. p-value<0.05 is considered to be statistically significant.
Swelling: In both LAA and LAK groups, swelling after the surgical removal was increased on 1st post-operative day and then decreased gradually to pre-operative level on the 7th post-operative day. The average day 1 post-op swelling score was significantly higher in LAA group compared to LAK group (p-value<0.05). No significant statistical difference in swelling was found between two groups on 2nd and 7th post-operative days. [Table/Fig-7] shows the comparison of post-operative swelling score across the 2 study groups.
The inter-group comparison of swelling score.
| Swelling Score | Lignocaine(n=25) | Lignocaine + Ketamine(n=25) | Inter Group Comparisons(p-value)* |
|---|
| Pre-op | 37.8 ± 1.1 | 37.5 ± 1.9 | 0.483 |
| Day 1 | 39.2 ± 1.1 | 38.3 ± 1.7 | 0.036 |
| Day 2 | 38.4 ± 1.1 | 37.9 ± 1.8 | 0.302 |
| Day 7 | 37.9 ± 1.1 | 37.6 ± 1.8 | 0.357 |
| Difference at Day 1† | 1.40 ± 0.39 | 0.84 ± 0.56 | 0.001 |
| Difference at Day 2† | 0.62 ± 0.39 | 0.49 ± 0.33 | 0.209 |
| Difference at Day 7† | 0.19 ± 0.18 | 0.11 ± 0.10 | 0.166 |
| % Difference at Day 1‡ | 3.7% | 2.3% | 0.001 |
| % Difference at Day 2‡ | 1.7% | 1.3% | 0.251 |
| % Difference at Day 7‡ | 0.5% | 0.3% | 0.214 |
* Values are Mean ± Standard Deviation. p-values by independent sample t-test. p-value<0.05 is considered to be statistically significant.
† Difference is calculated using formula = Post op – Pre op.
‡ %Difference is calculated using formula = (Post op – Pre op) x 100 /(Pre op).
Trismus: Limitation in the mouth opening was maximum on 1st post-operative day in both LAA and LAK groups. No significant statistical difference was seen between the two groups on the following post-operative days. [Table/Fig-8] shows the intergroup comparison of mouth opening.
The inter-group comparison of mouth opening score.
| Mouth Opening Score | Lignocaine(n=25) | Lignocaine + Ketamine(n=25) | Inter Group Comparisons(p-value)* |
|---|
| Pre-op | 48.9 ± 3.5 | 47.6 ± 4.4 | 0.247 |
| Day 1 | 26.6 ± 5.7 | 26.8 ± 9.0 | 0.940 |
| Day 2 | 31.2 ± 5.8 | 30.9 ± 8.9 | 0.881 |
| Day 7 | 40.8 ± 4.5 | 40.3 ± 6.5 | 0.724 |
| Difference at Day 1† | 22.2 ± 5.8 | 20.8 ± 9.7 | 0.515 |
| Difference at Day 2† | 17.6 ± 6.1 | 16.3 ± 10.2 | 0.581 |
| Difference at Day 7† | 8.0 ± 4.6 | 7.3 ± 4.3 | 0.637 |
| % Difference at Day 1‡ | 45.4% | 43.4% | 0.646 |
| % Difference at Day 2‡ | 36.0% | 34.5% | 0.740 |
| % Difference at Day 7‡ | 16.3% | 15.0% | 0.704 |
* Values are Mean ± Standard Deviation. p-values by independent sample t-test. p-value<0.05 is considered to be statistically significant.
† Difference is calculated using formula = (pre-op mouth opening) – (Post-op mouth opening)
‡ %Difference is calculated using formula = (Pre op – Post op) x 100 /(Pre op)
Discussion
Assessment of difficulty of third molar surgery is fundamental to forming an optimal treatment plan in order to minimize complications. A compilation of both clinical and radiological information is necessary to make an intelligent estimate of the time required to remove a tooth.
It has been suggested that patient factors also have an important impact on increasing difficulty of third molar surgery; particularly age, gender, size and ethnic background, but only age has been previously linked with increased surgical time and complications [8]. The same operating surgeon carried out surgical removal of bilaterally symmetrical impacted 3rd molars in the same patient in this split mouth clinical controlled study to eliminate operator bias and bias due to patient factors.
The surgical removal of impacted mandibular third molars is a commonly performed dento-alveolar procedure by oral surgeons and is often accompanied post-operatively with varying degrees of discomfort. Pain, swelling and trismus are the most common post-operative complaints and these influence patients’ quality of life in the days after surgery. Minimizing post-operative pain, swelling and trismus allows patients having undergone the surgical procedure for removal of the third molars to return to normal work-related and social activities in a shorter time.
The availability of a myriad number of potent local anaesthetic solutions makes satisfactory analgesia possible during dental surgical procedures. The conventional local anaesthetics though adequate, are of short duration; however in most oral surgical procedures, a prolonged duration of analgesia would be desirable. It has been emphasized previously that total or optimal pain relief allowing normal function cannot be achieved by a single drug or method, therefore, combined analgesic regimens or a multimodal approach to the treatment of post-operative pain is recommended [2,4,9]. The rationale for this strategy is achievement of sufficient analgesia due to synergistic effects of different analgesics with concomitant reduction of side effects of each individual agent.
The present study compared the efficacy of low dose ketamine as an adjunct to lignocaine in reduction of post-operative pain, facial swelling and trismus after surgical removal of impacted mandibular third molars. Ketamine is the only anaesthetic available that has analgesic, hypnotic and amnesic effects. It produces a state of dissociative anaesthesia resulting from electrophysiological dissociation between the limbic and cortical systems. When used correctly, it is a very useful and versatile drug [10].
Ketamine is a well known general anaesthetic and when given in low doses it has analgesic [1,2,4] and anti-inflammatory effects [11]. It has been shown that addition of ketamine in a sub-anaesthetic dose to local anaesthetic prolongs the duration of regional anaesthesia and post-operative analgesia [2,4,12].
Satılmis et al., used 0.3mg/kg ketamine in combination with articaine HCl for mandibular anaesthesia; their results showed that the combination of a local anaesthetic and sub-anaesthetic doses of ketamine during surgical extraction of third molars produced good local anaesthesia, while providing a comfortable procedure for the patient and good post-operative analgesia, with less swelling and significantly less trismus [13].
Mazar et al., stated that the anti-inflammatory effects of ketamine were mediated by the release of adenosine and were effective only at the initial stage of sepsis [14]. They also pointed out that the administration of sub-anaesthetic doses of ketamine might be advantageous in patients who undergo elective surgery or other invasive procedures with a high risk for bacteraemia.
The peri-operative administration of low-dose ketamine, given intravenously or by peritonsillar infiltration, provides effective pain relief without side effects in children undergoing adeno-tonsillectomy [15]. Ketamine infiltration into the tonsillar region is an easy and effective way of providing a high level of analgesia for pain management after tonsillectomy [16]. Tan et al., concluded that pre-incisional, subcutaneous ketamine infiltration can suppress post-operative pain and decrease post-operative early analgesic requirements [17].
Ketamine when combined with local anaesthetic shows less post-operative pain, swelling and trismus after 3rd molar extraction [13]. Pain after third molar surgery can be of varying intensity and has been found to co-relate with the duration of the procedure and the amount of surgical trauma. Pain is usually more severe during first post-operative day [18]. In view of this, there appears to be a definite place for use of long acting local anaesthetics.
In the present study, pain intensity in both the groups was compared through Visual Analog Scale (VAS) scores at 1st, 2nd and 7th day post-operatively. Pain scores were highest during 1st post-operative day in both groups and gradually decreased on 2nd and 7th day. Pain score was higher on 1st and 2nd post-operative day in LAA group than LAK group and was statistically significant. (p-value<0.05). In our study, using the combination of local anaesthetic and sub-anaesthetic ketamine during surgical extraction of third molars produced long lasting post-operative pain control.
Post-operative swelling was measured by the tape measurement method described by Gabka and Matsumara in which sum of three measurements was taken between five reference points on face and difference was measured between pre-operative and post-operative values [7]. In both the groups, swelling after the surgical removal was increased on first post-operative day and then decreased gradually to pre-operative level on 7th post-operative day. The average day 1 post-op swelling score was significantly higher in LAA group compared to LAK group (p-value<0.05). No significant statistical difference however in swelling was found between the two groups on 2nd and 7th post-operative days.
Trismus was calculated by measuring distance between mesial-incisal corners of right upper and lower central incisors and difference was calculated from pre-operative measured values. Limitation in the mouth opening was maximum on 1st day post-operatively in both the groups. No significant statistical difference was seen between two groups on any post-operative days.
The present results show a statistically significant decrease in patient’s pain perception on first and second post-operative day and a significant decrease in post-operative swelling on first post-operative day in LAK group. This is related to the synergistic action of ketamine in potentiating analgesia.
The relief of pain is in tune with the conclusion of a recent study by Hadhimane et al., which concluded that pain scores on VAS at 30 minute, 1, 4, 12 hour and 1 day post-operatively were significantly lower in the Test group than in the Placebo group (p<.05). However with respect to facial swelling and mouth opening in their trial the Test group and Placebo group showed overall no statistically significant difference (p>.05) on the 1st, 3rd and 7th post-operative days [19].
Contrary to the present study Kumar et al., concluded that there was a statistically significant difference in mouth opening between their LAA and LAK group and a significant difference in terms of facial swelling in the immediate post-operative period and post-operative day one between the two groups. However in their study the dosage of ketamine injected was slightly higher than ours at 0.3mg/kg [20].
As the dosage in dental study of these solutions is far below than used in medical practice, the risk involved may be considered low. It is employed as an agent for induction of anaesthesia by the intravenous/intramuscular route. Slow intravenous injection at the dose of 1-2mg/kg over a period of 60 seconds produces surgical anaesthesia within 1-2 minutes which may be expected to last 5 to 10 minutes. At the dose of 6-8mg/kg by deep intramuscular injection surgical anaesthesia results within 3-5 minutes and may be expected to last up to 25 minutes. Following induction, as above, serial doses of 50% of the original intravenous dose or 25% of the intramuscular dose are administered as required [21].
Classical side effects after ketamine anaesthesia are amnesia, altered short-term memory, decreased ability to concentrate, decreased vigilance, altered cognitive performance, hallucinations, nightmares, headache, dizziness, nausea and vomiting, blurring of vision, excessive salivation and lacrimation [4]. However in sub-anaesthetic doses, these reactions are infrequent. In our study, transient dizziness and headache was noticed in four patients in LAK group soon after administering the solution. No adverse reaction was reported in LAA group.
Limitation
Relatively smaller sample size and the fact that patients were from a different demography are the main limitations of the study. A more stringent criterion for standardization of the type of impaction with perhaps a more comprehensive index could have also been applied. High quality randomized controlled clinical trials with different minor surgical procedures and a significantly larger sample size with follow-up on the pain relief of low dose ketamine are imperative to corroborate this study. Further randomized studies will highlight the best administration technique and dose for ketamine in dental surgery.
Conclusion
Ketamine is known to exert anti-inflammatory effects and this anti-inflammatory property of ketamine has a distinct advantage during third molar removal. There is a demonstrable need to have several adjunctive analgesics and alternative modalities for analgesia at our disposal and low dose ketamine is an additional tool that can be added to our belt. The use of ketamine in patients where the administration of opioids may be problematic (opioid tolerance, opioid-induced hyperalgesia, true allergy) is another indication for this promising drug.
To conclude, the role of ketamine in low doses as analgesic and anti-inflammatory is evident in our study. The combination of a local anaesthetic and sub-anaesthetic doses of ketamine injected for surgical removal of impacted third molars provides good local anaesthesia while alleviating post-operative sequelae for the patient by providing a degree of post-operative analgesia with less swelling.
Funding: This research received no specific grant from any funding agency in the public, commercial, not-for-profit sectors.
The Author(s) declare(s) that there is no conflict of interest.
Values are Mean ± Standard Deviation.
*p-values by independent sample t-test. p-value<0.05 is considered to be statistically significant.
* Values are Mean ± Standard Deviation. p-values by independent sample t-test. p-value<0.05 is considered to be statistically significant.
† Difference is calculated using formula = Post op – Pre op.
‡ %Difference is calculated using formula = (Post op – Pre op) x 100 /(Pre op).
* Values are Mean ± Standard Deviation. p-values by independent sample t-test. p-value<0.05 is considered to be statistically significant.
† Difference is calculated using formula = (pre-op mouth opening) – (Post-op mouth opening)
‡ %Difference is calculated using formula = (Pre op – Post op) x 100 /(Pre op)