The classic triad of findings for a splenic abscess is fever, left upper quadrant pain and splenomegaly was proposed by Petroianu et al., [4]. It is reported that an abscess in spleen can develop by 4 ways: (i) Hematogenous: Most commonly by hematogenous seeding from other sites of infection. The two most common sources are the heart in endocarditis and direct introduction of bacteria into the blood with Intravenous Drug Use (IVDU); (ii) Trauma and subsequent ischemia creates an environment for bacteria to grow. Overt trauma is through external forces or microscopic trauma due to haemoglobinopathies; (iii) Contiguous focus of infection like pancreatic or subphrenic abscess, or from adjacent infected segments of bowel; (iv) Immuno-compromised state like Human Immunodeficiency Virus (HIV) infection or diabetes mellitus or transplant or neoplasia [4], by Sandra Jenneson et al., [5].
The most common organisms in most reported series have been aerobic microbes and particularly Streptococcus and Escherichia coli [6]. As there is no definite treatment for splenic abscess [7], traditional treatment includes appropriate antimicrobial therapy with or without splenectomy [2]. The success rate of Percutaneous Drainage (PCD) for splenic abscess has been reported between 67% and 100% [1]. However, it is recognized that PCD may be appropriate in unilocular, thin content and peripherally located abscess [8], but surgery remains the gold standard treatment [9]. The purpose of this study was to study the clinical profile of splenic abscess.
Materials and Methods
Case records of admitted patients with splenic abscesses, to Nizam’s Institute of Medical Sciences and Hospital which is a multispeciality, tertiary care referral hospital were collected over a period of 15 months (from March 2014 to May 2015).
Inclusion criteria was: 1) All patients diagnosed with Splenic Abscess. 2) Age above 12 years was included.
All the patients below 12 years were excluded. Information from case sheets of all patients recruited for analysis was reviewed. In the history, demographic details, symptoms with the duration, loss of appetite and weight were noted. The risk factors information tabulated were septicaemia, trauma, contiguous infection and immunocompromised status of patient.
Clinical findings specifically noted were presence of temperature, enlargement of spleen and pleural effusion.
The investigation reports of Haemogram, chest radiograph, abdominal ultrasonography (carried with MYLAB60 model, eSaote company from Ahmedabad), Contrast Enhanced Computed Tomography (CECT) of abdomen (carried with Philips Brilliance 16 model, 16 slice CT, PHILIPS company from Netherlands), Mantoux test, HIV ELISA, Electrocardiogram, trans-thoracic Echocardiogram, blood cultures and urine cultures were documented.
The treatment details like medical management including surgical procedures were also noted. Antibiotics dose and duration and wherever given antifungal antibiotics dose and duration of therapy were documented. Information on percutaneous drainage, subtotal/ total spleenectomy wherever done were noted.
The above data from all patients was tabulated and analysed retrospectively. The reports of CECT chest, Bone marrow study, Fine Needle Aspiration Cytology (FNAC)/ biopsy of lymphnode and/or spleen were also collected (wherever they were carried out depending on clinical profile).
The study was retrospective audit with no patient direct identifiers, hence consent was not taken. Hospital ethics committee was informed of the study.
Results
Total number of cases collected was nine. In the series age varied from 14 to 50 years with a mean of 33.5 years. Male to female ratio was 6:3. Duration of symptoms varied from 12 days to 180 days with a mean duration of 62.4 days. Commonest symptom was fever seen in eight out of nine patients. Other symptoms observed in our series with order of decreasing frequency were left hypo-chondrial pain in six, cough in three, loss of weight & appetite in three, vomiting in two, breathlessness in two, loose motions in one, jaundice in one, melena in one and pyemic cutaneous abscesses in one. There was no history of trauma in any of them.
Five out of nine had risk factors, three had HIV infection with significant immuno-suppression (CD4 cells below 100/ml), one had leukaemia (Acute Promyelocytic Leukaemia) and one had diabetes.
On clinical examination, all had anaemia & splenomegaly. Oral candidiasis indicating underlying immuno-suppression was seen in two patients (with HIV infection). However tender splenomegaly was noted in five. Hepatomegaly was seen clinically in two but by Ultrasound abdomen in five.
Moderate to severe anaemia was found in all but no significant leukocytosis in anyone. Thrombocytopenia as a part of Dissemi-nated Intravascular Coagulation was seen in one. Erythrocyte Sedimentation Rate (ESR) was elevated in all but four of them to an extent of >100mm/1st hour. Blood peripheral smear examination was done in all patients, in one patient Plasmodium falciparum was seen.
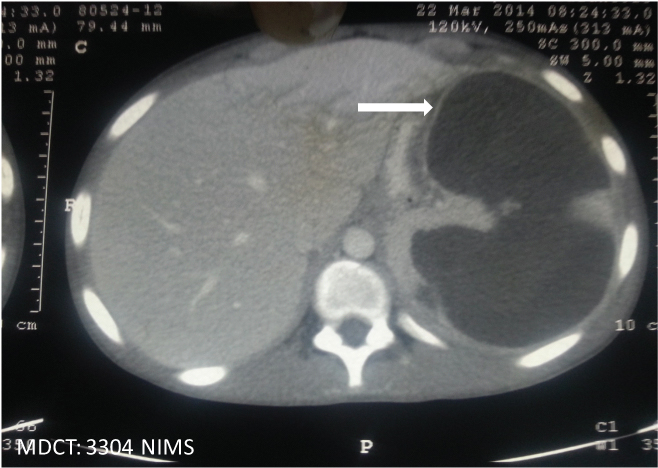
All patients underwent ultrasound abdomen and CT scan abdomen and all were found to have splenic abscess by both modalities. Pleural effusions were seen in four out of nine. Splenic infarcts were noted in 1. Single large abscess [Table/Fig-1] was seen in three [Table/Fig-2], whereas multiple abscesses were noted in the rest [Table/Fig-3]. In addition to splenic abscesses, intra-abdominal abscesses (like hepatic and para-vertebral abscesses) were noted in three and necrotic lymphadenopathy in three. In patients with HIV infection, CT chest was also done and noted to have pulmonary parenchymal nodules in all three and pleural effusions in two.
CT scan abdomen (white arrow) showing single large abscess of spleen in a patient of acute promyelocytic leukaemia.
Clinical Information of patients.
| Sn | Gender | Age (years) | Risk factor | Number of abscess | Size (cm) | Aetiological diagnosis | Treatment | Outcome |
|---|
| 1 | Male | 47 | None | Single | 8.5 X 5.5 | Plasmodium falciparum | PCD, anti-malarials | Recovered |
| 2 | Male | 14 | Leukaemia | Single | 15 X 10 | MRSA & E.fecium | Subtotal splenectomy antibiotics | Recovered |
| 3 | Male | 38 | HIV | Multiple | - | Could not be identified | Empirical Anti tubercular drugs | Recovered |
| 4 | Male | 28 | None | Multiple | - | Could not be identified | Empirical Anti tubercular drugs | Recovered |
| 5 | Male | 42 | HIV | Multiple | - | Could not be identified | Empirical Anti tubercular drugs | Recovered |
| 6 | Female | 50 | Diabetes | Multiple | - | E.coli & P.aeroginosa | PCD, antibiotics | Recovered |
| 7 | Female | 18 | Infective endocarditis | Multiple | - | Could not be identified | Antibiotics | Recovered |
| 8 | Male | 35 | HIV | Multiple | - | Cryptococcus neoformans | Antifungals | Recovered |
| 9 | Female | 30 | None | Single | 5 X 2 | E.coli & Brucella | PCD, Antibiotics | Recovered |
CT Scan abdomen (white arrows) showing multiple abscesses in spleen.

Blood culture showed growth of Cryptococcus neoformansin one and Pseudomonas aeroginosa in another, rest seven did not reveal growth of any organisms. Five patients underwent FNAC Fine Needle Aspiration for Cytology (FNAC) from splenic abscess. One patient underwent splenic biopsy which showed evidence of Cryptococci on staining of pus. Three patients had an evidence of bacterial growth on pus culture. Escherecia coli of ESBL (Extended Spectrum Beta Lactamase) type, was grown in two (one of them had serological evidence of Brucella abortus infection also). Third patient in this group had a growth of Methicillin Resistant Staphylococcus aures and Enterococcus faecium.
From the above evidence it was noted as bacterial sepsis in three, fungal sepsis in one and malaria in one [Table/Fig-2]. Hence, three patients were treated with antibiotics in accordance with anti-biogram reports E.coli ESBL with Imipenem, Brucella with Rifampicin, Doxycycline, one with antifungals (amphotericin) and another with anti-malarials (artesunate). One patient was treated as culture negative Infective Endocarditis, possible Infective Endocarditis diagnosis was made based on modified Duke’s criteria)with antibiotics. Rest of the three were diagnosed to have disseminated Koch’s infection basing on clinical profile & imageological evidence and treated with empiricalanti-tuberculous drugs, Isoniazide, Rifampicin, Pyrizanamide, Ethambutol for two months and Isoniazide, Rifampicin for 4 months [Table/Fig-2].
A total of four out of nine patients required invasive procedures. PCD was done in three patients when abscess was located superficially & liquified, subtotal splenectomy was done in one patient who had very large abscess. None of them underwent total spleencetomy [Table/Fig-2].
Underlying predisposing conditions were managed with specific therapies along with supportive care. All improved clinically from septicaemia and splenic abscesses. There was no mortality [Table/Fig-2]. All were under follow-up.
Discussion
Splenic abscess is an uncommon condition [10] with Bi-model age distribution in splenic abscesses was described in literature [11]. Peak incidences are between ages 30-40 and 60-70 years; males and females are equally affected [11]. But in our study we found that the age of the patients varied from 14 to 50 years with a mean of 33.5 years, similar to Sreekar et al., [Table/Fig-4] [12]. The discrepancy was because of narrow range of age which may be due to short period of collection, when compared to other studies, where the period study was extended to more than a decade.
Comparison of results of present study with other published studies [1,7,10,12,14–18].
| Variable | S Anuradh et al., [16] | Dhiraj Agarwal et al., [17] | Dubhasigupta et al., [7] | Mamom A Khalid et al., [10] | Abdul Rehman et al., [18] | Kuo-Chin Chang et al., [1] | Giovanna Ferraioli et al., [14] | I-Shun Chiang et al., [15] | H. Sreekar et al., [12] |
|---|
| Year published | 2000 | 2012 to 2015 | 2015 | 2006 | 2008 | 2006 | 2009 | 2003 | 2011 |
| Country | India | India | India | Basrah | Pakistan | Taiwan | Italy | Taiwan | CMC (India) |
| Duration of study (yrs) | NA | 3years | NA | 1999-2005 | 1988-2000 | 1985-2004 | 1979 –2005 | 1990 –2001 | 1999 –2009 |
| Number of cases | 3 | 18 | 5 | 10 | 27 | 67 | 16 | 29 | 75 |
| Male : female | 1:2 | 11:7 | 4:1 | 6:4 | 12:15 | 41:26 | 12:4 | 18:11 | 52:23 |
| Mean age (yr) | 39 | 37.22 | 45 | 25 | 43.52 | 54.1 | 39.9 | 44 | 34.98 |
| Age range (yr) | 32-50 | 16-60 | 40-50 | 11-45 | 15-70 | 19-79 | 16-72 | 4-85 | 3-88 |
| Risk factors n(%) | 2/3(66.66%) | 10(55%) | 3/5(60%) | 3(30%) | 25(90.6%) | 54/67 (80.6) | 16/16 (100) | 22/29 (75.8) | 60/75 (80) |
| Fever (%) | 3/3(100%) | 16(85%) | 5(100%) | 10(100%) | 92.6% | 85 | 93.8 | 90 | 89 |
| Left upper quadrant pain (%) | 2/3(66.66%) | 8(46%) | 5(100%) | 10(100%) | 55.6% | 43.3 | 81.3 | 31 | 84 |
| Splenomegaly (%) | 2/3(66.66%) | 9(50%) | 5/5(100%) | 5/10(50%) | 9/27(30%) | 67.2 | 43.8 | 17.2 | 33 |
| Left pleural effusion (%) | NA | NA | 2/5(20%) | NA | NA | 41.5 | NA* | 3 | NA* |
| Most common aaetiological agent | Streptococcus Virandans | E Coli & Staphylococcus | Staphylococcus | Streptococcus | Streptococcus, Staphylococcus, Ecoli | E.coli | Staph aureus | Staph aureus | Staph aureus & E.coli |
| Treatment | | | | | | | | | |
| Antibiotics only n(%) | 1 | 8 | - | 1 | 13 | 20(29.9) | 1(6) | 24(82.7) | 14(18.6) |
| Per Cutaneous Drainage & antibiotics n(%) | 2 | 4 | - | 3 | 8 | 21(31.3) | 12(75) | 2(6.9) | 19(25.3) |
| Splenectomy & antibiotics n(%) | - | 6 | 5 | 6 | 6 | 26(38.8) | 3(18.7) | 3(10.3) | 42(56) |
| Mortality n(%) | - | 4 | - | - | 2 | 12(18) | 7(43.7) | 8(27.6) | 5(6.7) |
In our study, fever was most common presenting symptom (90%), followed by left hypochondrial pain (66.7%) similar to Won suk lee et al., [13]. Splenomegaly was seen in all patients unlike other studies where it is seen in 17 to 77.8% [1,12–15]. Risk factors were present in 55% where as in other studies it is about from 70 to 100% [Table/Fig-4] [1,12–18]. Clinical triad of fever, left hypochondrial pain, splenomegaly is seen in 66.7%, higher than in other studies [1,13,15–17]. As there is an increased incidence of infections with drug resistant bacteria, the immuno-competent persons are also becoming vulnerable to septicaemia and splenic abscesses formation.
In our study, two patients had sterile blood cultures but growth was identified from pus culture. In one patient, different organisms were isolated from both blood and pus. In one patient blood culture showed growth of fungus but pus culture was sterile similar to study by Ferraioli et al., [14].
In our study, most common aetiological agent isolated was Escherichia coli, a Gram Negative Bacili, similar to Kuo-chingchang et al., and Sreekar et al., [1,12]. Staphylococcal aureus was seen in only one patient unlike other studies Ferraioli et al., and I-Shun Chiang et al., where it was the most common [Table/Fig-4] [14,15].
In our study, we found that ultrasonogram test was equally sensitive to CT abdomen in diagnosing splenic abscess in all patients similar to sreekar et al., even though CT has high resolution and better definition of abscess [11]. Ultrasonogram is easy to perform, cost effective and can also be used as a therapeutic tool for PCD. Similar inference was made by KO WC et al., from their study [19].
In our study, a clinical diagnosis of disseminated Koch’s was made in three patients, based on clinical, imgeological and histopathological (granulomas) profile from lymphnode biopsy. Invasive methods like FNAC/biopsy were not performed in these patients, similarly it was stated by SK Sharma et al., that other invasive methods of spleenic lesion need not to be done for diagnosing Koch [20].
Most of our patients (88%) received conservative management similar to I-Shun Chiang et al. All patients in our study recovered unlike in other studies where mortality was varied from 6.7 to 43.7% [1,12–15]. This may be because of more number of immune-competent patients and less mean age of participants when compared to other studies.
Limitation
As study had a small number of patients its statistical analysis becomes weak, since it was a retrospective study all data could not be retrieved like in prospective study and follow-up data could not be presented.
Conclusion
Splenic abcess is a rare entity, which can be diagnosed early by high degree of suspicion, with judicious use of ultrasound and CT abdomen and with prompt early intervention mortality can be minimized.