Introduction
Essential hypertension is one of the most common diseases of the Indian population contributing greatly to the morbidity, mortality and economic burden. It has a strong association with cardiovascular disease and abnormal lipid metabolism. Not only the traditional lipid parameters, but also the novel lipid components like Apo A1 and Apo B100 also have been identified to play a role.
Aim
The present study was done to evaluate serum lipid profile and Apo A1, Apo B 100 in essential hypertensive patients and correlate their values with the degree of hypertension.
Materials and Methods
Fasting samples from 55 age and sex matched controls and 55 essential hypertensives were tested for plasma glucose, serum urea, creatinine, lipid profile, apo A1 and apo B100. The cases were subclassified based on the severity of hypertension according to JNC criteria.
Results
The study showed a significantly raised value for serum cholesterol, triacylglycerol, Low Density Lipoprotein (LDL), Very Low-Density Lipoprotein (VLDL) in the hypertensive patients than the control group whereas serum High-Density Lipoprotein (HDL) registered a fall in the cases. Apo A1 revealed a non-significant fall in the hypertensive patients. In contrast, there was a rise in the serum apo B100 in the cases. Apo B100/apo A1 ratio was significantly raised in both stage I and stage II hypertensive patients in comparision to the controls. When correlated, serum apo A1 revealed a negative association where as serum apo B 100 showed a positive association with systolic and diastolic bloood pressure. Both LDL/HDL and apoB100/apo A1 and apo B100 revealed a significant positive association with both SBP and DBP. However, apoB100/apo A1 revealed a more positive association in comparision to LDL/HDL ratio (r=0.749, p<0.001, r=0.756, p<0.001 vs r=0.336, p<0.000, r=0.312, p<0.001).
Conclusion
Apo B100/apoA1 has emerged as an important complementary parameter in addition to traditional lipid ratio for evaluation of risk for future cardiovascular disease.
Introduction
Essential hypertension, a major health problem in the developed countries, affecting nearly one billion people worldwide [1]. It has a strong association with cardiovascular disease and contributes greatly to morbidity, mortality and economic burden [2], Accounting for about 57% of all deaths due to stroke and 24% of all deaths due to coronary heart disease in India [3]. By 2025, the number of hypertensive individuals may rise to 213 million from 118 million in 2000 [4]. The major risk factors for hypertension include obesity, smoking, alcohol consumption, dyslipidemia apart from the dietary pattern [5]. Various studies have implicated a close association of dyslipidemia and hypertension [6,7].
Altered serum lipid and lipoprotein levels are considered as independent modifiable risk factors for hypertension which can be corrected by diet, drugs and exercise. The untreated hypertensives are more prone for dyslipidemia than normotensives and studies reveal that there is an increase in blood pressure with rise in lipid level [8]. Studies by Osuji et al., reveal that hypertensives do not have specific pattern of dyslipidemia and total cholesterol, triglycerides and all fractions of lipoproteins tend to be more frequently abnormal in the hypertensives than the general population [9]. Recent studies suggest that plasma concentration of Apo A1 and Apo B100 and their ratio are more sensitive and specific biochemical markers for the risk of coronary heart disease than the conventional lipid and lipoprotein measurement [10,11].
Apo A1 is the major protein component of High Density Lipoprotein (HDL) and associated with fat efflux including cholesterol from tissue to liver for excretion. It activates plasma Lecithin Cholesterol Acyl Transferase (LCAT) which is responsible for the formation of most plasma cholesterol esters. ApoB100 is the main functional protein for transporting cholesterol to the peripheral cells and responsible for cellular recognition and catabolism of cholesterol of Low Density Lipoprotein (LDL). LDL, & VLDL particles present an apoB100 molecule in their structure, therefore the plasma concentration of Apo B100 indicates the total number of potentially atherogenic particles where as the measurement of Apo A1 represents total antiatherogenicity owing to reverse cholesterol transport by apoA1.
Aim
The aim of the present study was to evaluate serum lipid profile and Apo A1, Apo B 100 in essential hypertensive patients and correlate their values with the degree of hypertension.
Materials and Methods
This was a case control study conducted in the Department of Biochemistry, in collaboration with Department of Medicine SCB Medical College and Hospital Cuttack from March 2014 to September 2015. The study has undergone institutional ethical clearance. Written, informed consent was obtained from all subjects for collection of the blood samples as well as data required for the study.
The study group comprised of 55 essential hypertension patients-39 males and 16 females within age group 30-50 years, attending OPD and indoors in the Department of Medicine, SCB. Medical College and Hospital, Cuttack and 55 healthy volunteers-30 males and 25 females between 30-50 years of age with no symptoms and signs suggestive of hypertension and no family history of the hypertensive disease as controls. The lipid profile of most of the patients of the control group was within the reference range.
The selection of the essential hypertension cases was made on the basis of their history, physical examination, biochemical investigations according to the JNC 7 (Joint National Committee on Prevention, Detection, Evaluation and Treatment of High Blood Pressure) Criteria for the diagnosis of hypertension [12].
A 3ml of venous blood was collected after overnight fasting of 8 hours from all enrolled patients and healthy controls for the assessment of Apolipoprotein A1 and Apolipoprotein B100 levels and other biochemical parameters like fasting plasma glucose, serum urea, creatinine, lipid profile. Detailed history and physical examination which includes systolic and diastolic blood pressures, Waist- Hip Ratio (WHR), weight were recorded. Patient with diabetes mellitus, renal disease, endocrinopathy, pregnancy induced hypertension, immunosupression and history of illicit drug use were excluded from the study. In the control group, subjects with family history of hypertension, renal diseases and chronic metabolic diseases were also excluded. All the case records were collected in a specified proforma.
The blood pressure measurement was taken while the subject was in the sitting position. Manual blood pressure measuring instrument sphygmomanometer was used. Two readings were taken at a single visit and the average was calculated. The routine biochemical parameters were carried out by the standard methods using Toshiba 120 FR autoanalyser. The novel markers Apo A1 and Apo B 100 were assayed by immunoturbidimetric methods in the Biolis 24i autoanalyser. Anti – Apo A1 and Anti – apo B100 antibodies when mixed with samples containing Apo A and Apo B, form insoluble complexes causing an absorbance change, depending upon the apoA and apo B concentration of the patient sample. The ApoA and ApoB levels in the patients samples be quantified can be comparison with calibrators of known Apo A and Apo B concentration.
Statistical Analysis
All statistical analyses were performed using SPSS version 16.0 software and Microsoft Office Excel 2007. Data were expressed as mean ± SD. Student’s t-test and Anova test were used to compare mean values and calculate significance. Data were considered statistically significant if p-values were < 0.05. Pearson’s coefficient of correlation was used to assess linear correlation between serum apolipoprotein A1, B100 and other variables.
Results
[Table/Fig-1] reveals majority of the hypertensive patients were smokers, belonged to the good socioeconomic status and had higher WHR in comparison to the control group. [Table/Fig-2] revealed that the hypertensive patients had raised values for Fasting Blood Sugar (FBS), renal function and all fractions of lipid profile in comparison to the control group. Comparision of data was done by one-way ANOVA and post-hoc Tukey HSD. [Table/Fig-3] reveals significant positive association of different fractions lipid profile with systolic, diastolic blood pressure.
Demographic parameter is the study group.
| Parameters | Control (N=55) | Stage-1 (N=39) | Stage -2 (N=16) |
|---|
| Age (in yrs) | 37.2± 5.05 | 39.6±5.23 | 40.6+4.95 |
| Sex (M/F) | 30/25 | 23/16 | 10/6 |
| WHR | 0.9±0.04 | 0.95±0.051* | 0.96±0.03* |
| SBP (mm Hg) | 119±8.74 | 151±4.68* | 162±2.68*o |
| DBP (mm Hg) | 72.7±3.5 | 93±4.6* | 95±4.6* |
| Smoking (Smokers/Nonsmokers) | 15/40 | 21/18 | 13/3 |
| Socio Economic status (Good/Average) | 30/25 | 25/14 | 14/2 |
*p<0.001 when compared with the control group
op<0.001 when compared between two stages of hypertension
Routine Biochemical parameters in the study group.
| Parameters | ControlMean ± SD(N=55) | Stage-1HypertensionMean ± SD(N=39) | Stage-IIMean ± SD(N=16) |
|---|
| FBS(mg/dl) | 73.9±7.60 | 83.2±9.05* | 88.1±5.38* |
| UREA(mg/dl) | 19.7±3.23 | 22.9±7.77* | 26.0±11.78* |
| CREATININE(mg/dl) | 0.718±0.12 | 0.79±0.17 | 0.83±0.16 |
| Total Cholesterol(mg/dl) | 143±15.7 | 194±34.9* | 200±33.0* |
| TG (mg/dl) | 107±32.5 | 205±66.2* | 197±70.5* |
| HDL (mg/dl) | 38.3±7.99 | 36.2±4.7* | 33.2±2.9* |
| LDL (mg/dl) | 83.5±12.4 | 118±30.7* | 129±28.7* |
| VLDL (mg/dl) | 27.22±6.79 | 31.34±7.63* | 33.4±4.86* |
*p<0.001 when compared with the control group
Correlation of serum lipid profile with systolic and diastolic blood pressure.
| Parameters | Systolic Blood Pressure | Diastolic blood pressure |
|---|
| r | p | r | p |
|---|
| Total Cholesterol(mg/dl) | 0.665* | <0.001 | 0.681* | <0.001 |
| TG(mg/dl) | 0.640* | <0.001 | 0.569* | <0.001 |
| HDL(mg/dl) | 0.370* | <0.001 | 0.428* | <0.001 |
| LDL(mg/dl) | 0.523* | <0.001 | 0.567* | <0.001 |
| VLDL(mg/dl) | 0.652* | <0.001 | 0.577* | <0.001 |
*p<0.001 considered significant
In [Table/Fig-4] revealed a significant rise in apoB100 and nonsignificant fall in the apo A1 in both stages of hypertensive patients as compared to the control group.
Comparison of serum Apo lipoprotein A1 & B-100 among controls hypertension patient.
| Parameters | Control(N=55) | Stage-1Hypertension(n=39) | Stage-IIhypertension(n=16) |
|---|
| Apo A1(mg/dl) | 117±7.06 | 110±7.63 | 109±5.29 |
| ApoB 100(mg/dl) | 61.0±18.2 | 101±14.2* | 99.4±10.9* |
| Apo B 100/Apo A1 | 0.516±0.15 | 0.915±0.11* | 0.909±0.09* |
*p<0.001 when compared with the control group
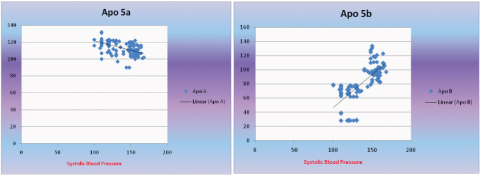
[Table/Fig-5a&b] revealed a positive association of apo B100 with Systolic Blood Pressure (SBP) and a and a negative association of apo A with SBP. [Table/Fig-6] reveals a more positive association of ApoB100/ApoA1 with both systolic and diastolic blood pressure than the LDL/HDL ratio.
Correlation of Apo A & Apo B 100 with Systolic Blood Pressure.
X Axis- Systolic Blood Pressure (mm Hg)
Y Axis- apoA(mg/dl)
X Axis - Systolic Blood Pressure (mm Hg)
Y Axis – apoB (mg/dl)
Correlation of ratio of Apo B100/ApoA1 and LDL/HDL with Systolic and Diastolic Blood Pressure.
| Parameters | LDL/HDLr | p | APO B100/APOA1r | p-value |
|---|
| SBP | 0.336* | <0.001 | 0.749* | <0.001 |
| DBP | 0.312* | 0.001 | 0.756* | <0.001 |
*p<0.001 considered significant
Discussion
The present study aims to identify the association of conventional lipid parameters LDL and HDL and new parameters such as Apo A1 and Apo B 100 in essential hypertensive patients. The mean Systolic Blood Pressure (SBP) and Diastolic Blood Pressure (DBP) were significantly higher in stage 1 and stage II hypertensive patients than the controls. The stage II hypertensive patients had significantly raised SBP in comparison to the stage 1 patients [Table/Fig-1]. The blood pressure has a continuous and consistent relationship with the risk of cardiovascular events, the higher the BP, the higher the chance of cardiovascular disease [13]. The hypertensive patients belonged to the older age group and had higher WHR in comparison to the controls which was significant statistically [Table/Fig-1]. 90% of the hypertensive patients were from the good socio economic status and adopted a sedentary life style [Table/Fig-1]. This is in accordance with the study conducted by James and Welborn who observed that WHR can be used as an indicator of risk in the ethically diverse population [14,15]. With ageing there is a rise in the systolic blood pressure which may be due to an increase in vascular stiffness of the arteries in combination which atherosclerotic change in the vessel wall. Several epidemiological studies have highlighted the association of arterial stiffness in hypertensive patients and other cardiovascular diseases in aged as compared to the younger age group. The prevalence of arterial stiffness and hypertension increases with age [16,17].
A rising trend for serum cholesterol TG, LDL, and VLDL along with a fall in HDL was found with the severity of hypertension [Table/Fig-2]. Significant positive correlation between serum lipid profile and both systolic and diastolic blood pressure was observed with increasing severity [Table/Fig-3]. Hypertension and dyslipidemia are well established and partially overlapping risk factors for cardiovascular disease [18,19]. Dyslipidemia plays a role in endothelial dysfunction which is central in the pathogenesis of atherosclerosis, thrombosis, insulin resistance as well hypertension. Triglyceride rich lipoproteins and LDL cholesterol have been shown to be toxic to endothelial cells, where as HDL cholesterol may be protective [20]. High levels of serum cholesterol are known to increase the risk of developing macrovascular complications such as Coronary Heart Disease (CHD) and stroke [21]. The increased risk of CHD when the cholesterol level exceeds 5.0 mmol [22] as seen in several epidemiological studies prompted Lewis [23] to suggest that serum TC in the range 5.0–6.5mmol/L may be considered undesirable.
Various studies [24–27] have revealed the role of apolipoproteins- Apo A1 & Apo B100, the two major apolipoprotein for lipid transport in the processes involving atherosclerosis and its complications. In the present study, we found a non-significant fall in the value of serum Apo A1 in the hypertensive patients when compared to controls (110±7.63 and 109±5.29 vs 117±7.06) [Table/Fig-4]. Estimation of serum Apo B100 revealed a significant increasing trend from the control group to Stage I and Stage II hypertensive patients reflecting its contributing role as cardiovascular risk marker (61.0±18.2 vs 101±14.2 and 99.4±10.9) [Table/Fig-4]. There was no significant change in the apolipoprotein levels in both stages of hypertension. These results simulate the study in a group of men at Harvard Medical School who found out the plasma concentration of atherogenic lipoprotein patients i.e., Apo B100 worked better in predicting coronary artery disease [28]. Haidari et al., showed that the severity of atherosclerosis correlated significantly with the serum Apo B which is in the normolipidemic subgroup [29]. Sabino et al., found out that after adjusting the role of gender, age, smoking and hypertension, Apo B level and Apo B/A1 ratio correlated independently with peripheral atherosclerosis and brain stroke [30].
Apo B100 /Apo A1 ratio is an indicator of the balance between the atherogenic and antiatherogenic cholesterol particles. In the present study, this ratio increased with the severity of hypertension. As hypertension is associated with increased risk of cardiovascular disease, Apo B/A1 ratio may serve as a potential predictive marker for future cardiovascular disease. Our observation corroborates with the study of Waldius et al., and Sniderman et al., [31,32]. In their study, ApoB100/Apo A1 was the best variable in comparison to other lipid ratios such as total cholesterol/HDL, LDL/HDL, Non HDL/HDL in quantifying cardiovascular diseases.
The ratio of Apo B100/A1 revealed a significant positive correlation with hypertension in the study group. LDL/HDL also revealed similar significant positive association with hypertension, but the former ratio showed a more positive correlation as compared to the latter ratio [Table/Fig-6]. A total of 36 out of 55 patients had a Apo B/A1 ratio above the cut-off value (0.9 in males and 0.8 in females).
Similar observation was also studied in large population based studies such as the “INTER HEART” study [25], MONICA/KORA study [26], and AMORIS STUDY [27]. The INTERHEART study is the largest case control study comprising of 15,152 patients with myocardial infarction compared to 14,820 subjects from 52 countries worldwide. The aim of the study was to find out the most common of the identified risk factors of MI. The strongest and most prevalent of the risk factor was apo ratio both in men and women in each of the 52 countries worldwide.
In the AMORIS study, the relationship between different types of stroke and lipid fractions, Apo B100, Apo A1, their ratio were examined in large group of, men and women and followed for a mean period of 10.3 years. The risk of stroke was seen in patients with high apo B and low apo A1 values. In multivariate risk analysis, the apo ratio was a stronger risk predictor than total cholesterol/HDL-C and LDL-C/HDL-C ratios.
The German MONICA/Kora study showed that in 1414 men and 1436 women without prior median follow-up of 13 years the TC/HDL C ratio predicted MI risk. In addition, the apo ratio was significantly related to increased risk of MI adjusted for age, smoking, alcohol, BMI, diabetes and hypertension.
Apolipoprotein measurement also present with some methodological advantages when compared to LDL [33]. LDL is quantified by Friedwald equation and cannot be extended in samples presenting with higher TG levels. On the other hand apolipoprotein may be measured directly in the plasma through accurate and precise internationally standardized methods [34,35] by using common reference material for Apo A1 and Apo B 100. Plasma apolipoprotein levels are less influenced by biological variables in contrast to plasma lipid levels which fluctuate during different metabolic alterations [36]. Therefore preanalytical variables have less influence in the measurements of apolipoproteins A-I and B [29,37].
Limitation
The limitation of the study includes smaller sample size and association of Apo B100, Apo A1and their ratio with other risk factors associated with CHD.
Conclusion
Apo B/Apo A1 ratio has emerged as an important complementary parameter for the evaluation of risk for future cardiovascular disease especially in essential hypertensive patients. However this study can be strengthened by taking a larger sample size and correlating the Apo B100/ Apo A1 ratio with angiographic studies, intimal thickness or other associated laboratory markers.
*p<0.001 when compared with the control group
op<0.001 when compared between two stages of hypertension
*p<0.001 when compared with the control group
*p<0.001 considered significant
*p<0.001 when compared with the control group
*p<0.001 considered significant
[1]. Kotchen TA, Hypertensive Vascular DiseaseHarrison’s Principles of Internal MedicinePart 1018th Edition(Section 5):2042-2052.Chapter 247 [Google Scholar]
[2]. Buttar HS, Li T, Nivedita R, Prevention of cardiovascular diseases: Role of exercise, dietary interventions, obesity and smoking cessationExp Clin Cardiol 2005 10(4):229-49. [Google Scholar]
[3]. Gupta R, Gupta N, Hypertension epidemiology in the 21st centuryIndia J Preventive Cardiology 2013 2(4):1-6. [Google Scholar]
[4]. Reddy KS, Shah B, Varghese C, Ramadoss A, Responding to the threat of chronic diseases in IndiaLancet 2005 366:1744-49. [Google Scholar]
[5]. Bhavani BA, Padma T, Sastry BK, Krishna Reddy N, Plasma Lipoprotein (a) levels in patients with untreated essential hypertensionIndian J Hum Genet 2003 9(2):65-68. [Google Scholar]
[6]. Selby JV, Newman B, Quiroga J, Christian JC, Austin MA, Fabsitz RR, Concordance for dyslipidemic hypertension in male twinsJAMA 1991 265:2079-84. [Google Scholar]
[7]. Borghi C, Interactions between hypercholesterolemia and hypertension; implications for therapyCurrent Opinion in Nephrology and Hypertension 2002 11(5):489-96. [Google Scholar]
[8]. Neaton JD, Wentworth D, Serum cholesterol, blood pressure, cigarette smoking, and death from coronary heart disease: overall finding and differences by age for 316 099 white menArchives of Internal Medicine 1992 152(1):56-64. [Google Scholar]
[9]. Osuji CU, OmejuaE G, Onwubuya Gladys I, Ahaneku GI, Serum lipid profile of newly diagnosed hypertensive patients in nnewi, south-east nigeriaInternational Journal of Hypertension 2012 1-7(710486):1-7. [Google Scholar]
[10]. Naito HK, Apolipoproteins: Biochemistry, metabolism and clinical significance developed by lipid and lipoprotien divisionClin Chem 1987 33:1051-52. [Google Scholar]
[11]. Stein EA, LipidsIn: Text Book of Clinical. Chemistry. Ed Teitz NB 1986 London, WBSaunders Co:829-900. [Google Scholar]
[12]. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 reportJAMA 2003 289:2560-72. [Google Scholar]
[13]. Stanley S, Franklin Nathan D, Wong Hypertension and cardiovascular disease: contributions of the framingham heart studyGlobal Heart 2013 8(1):49-57. [Google Scholar]
[14]. Flier JS, Maratos E, Obesity. Kasper, D.L. and Fauci, A.S. (eds)Harrison’s Principles of Internal Medicine 2005 16th edition:423-40. [Google Scholar]
[15]. Cameron AJ, Welborn TA, Zimmet PZ, Dunstan DW, Owen N, Overweight and Obesity in Australia: the 1999-2000 Australian Diabetes, Obesity and lifestyle studyMed J Aust 2004 180(8):418 [Google Scholar]
[16]. AlGhatrif M, Strait JB, Morrell CH, Canepa M, Wright J, Elango P, Longitudinal trajectories of arterial stiffness and the role of blood pressure: The baltimore longitudinal study of agingHypertension 2013 62:934-41. [Google Scholar]
[17]. Ferreira I, van de Laar RJ, Prins MH, Twisk JW, Stehouwer CD, Carotid stiffness in young adults: a life-course analysis of its early determinants: the Amsterdam Growth and Health Longitudinal StudyHypertension 2012 59:54-61. [Google Scholar]
[18]. Carmena R, Duriez P, Fruchart J-C, Atherogenic lipoprotein perticles in atherosclerosisCirculation 2004 109:III-2-7. [Google Scholar]
[19]. Gotto AM Jr, Evolving concepts of dyslipidemia, atherosclerosis, and cardiovascular diseaseJ Am Coll Cardial 2005 46:1219-24. [Google Scholar]
[20]. O’Connell BJ, Genest JR, High-density lipoproteins and endothelial functionCirculation 2001 104:2420-27. [Google Scholar]
[21]. Albuche J, Ferrieres J, Ruidavets JB, Guiraud-Chaumeil B, Perret BP, Chollet F, Serum lipids in young patients with ischaemic stroke: a case-control studyJournal of Neurology Neurosurgery and Psychiatry 2000 69(1):29-33. [Google Scholar]
[22]. McGill HC, Introduction to the geographic pathology of atherosclerosisLaboratory Investigation 1968 18(5):465-67. [Google Scholar]
[23]. Lewis B, The appropriate use of diagnostic services: (viii) the investigation of hyperlipidaemia: why, how and for whom?Health trends 1986 18(1):1-4. [Google Scholar]
[24]. Luc G, Bard JM, Ferrieres J, Evans A, Amouyel P, Arvelier D, Value of HDL cholesterol, apolipoprotein A1, lipoprotein A1, and lipoprotein A-1/A-II in prediction of coronary heart diseaseArterioscler Thromb Vasc Biol 2002 22:1155-61. [Google Scholar]
[25]. Yusuf S, Hawken S, Öunpuu S, Dans T, Avezum A, Lanas F, Effect of potentially modifiable risk factors associated with myocardial infarction in 52 countries (the INTERHEART study): case-control studyLancet 2004 364:937-52. [Google Scholar]
[26]. Meisinger C, Loewel H, Mraz W, Koenig W, Prognostic value of apolipoprotein B and A-I in the prediction of myocardial infarction in middle-aged men and women: results from the MONICA/KORA Augsburg cohort studyEur Heart J 2005 26:271-78. [Google Scholar]
[27]. Walldius G, Jungner I, Holme I, Aastveit AH, Kolar W, Steiner E, High apolipoprotein B, low apolipoprotein A-I, and improvement in the prediction of fatal myocardial infarction (AMORIS Study): a prospective studyLancet 2001 358:2026-33. [Google Scholar]
[28]. Pischon T, Girman CJ, Sacks FM, Rifai N, Stampfer MJ, Rimm EB, Non-high-density lipoprotein cholesterol and apolipoproteins B in the prediction of coronary heart disease in menCirculation 2005 112(22):3375-83. [Google Scholar]
[29]. Haidari M, Moghadam M, Chinicar M, Ahmadieh A, Doosti M, Apolipoprotein B as the best predictor of coronary artery disease in Iranian normolipidemic patientsClin Biochem 2001 34:149-55. [Google Scholar]
[30]. Sabino AP, De Oliveira Sousa M, Moreira Lima L, Dias Ribeiro D, Das Gracas Carvalho M, Apo B/A1 ratio in young patients with ischemic cerebral stroke or peripheral arterial diseaseTransl Res 2008 152(3):113-18. [Google Scholar]
[31]. Walldius G, Jungner I, Aastveit AH, Holme I, Furberg CD, Sniderman AD, The apoB/apoA-I ratio is better than cholesterol ratios to estimate the balance between plasma proatherogenic and antiatherogenic lipoproteins and to predict coronary riskClin Chem Lab Med 2004 42:1355-63. [Google Scholar]
[32]. Sniderman AD, Jungner I, Holme I, Aastveit A, Walldius G, Errors that result from the TC/HDL C ratio rather than the apoB/apoA-I ratio to identify the lipoprotein-related risk of vascular diseaseJ Intern Med 2006 259:455-61. [Google Scholar]
[33]. Lima LM, Carvalho MG, Sousa MO, Apo B/Apo A-I Ratio and Cardiovascular Risk PredictionArq Bras Cardiol 2007 88(6):e140-43. [Google Scholar]
[34]. Marcovina SM, Alberts JJ, Henderson LO, Hannon WH, International Federation of Clinical Chemistry standardization project for measurements of apolipoproteins A-I and B. III comparability of apolipoprotein A-I values by use of international reference materialClin Chem 1993 39:773-81. [Google Scholar]
[35]. Marcovina SM, Alberts JJ, Kennedy H, Mei JV, Henderson LO, Hannon WH, International Federation of Clinical Chemistry standardization project for measurements of apolipoproteins A-I and B. IV comparability of apolipoprotein B values by use of international reference materialClin Chem 1994 40:586-92. [Google Scholar]
[36]. Rifai N, Bachorik PS, Alberts JJ, Lipids, lipoproteins, and apolipoproteins. In: Burtis CA, Ashwood ER (eds)Tietz - textbook of clinical chemistry 1999 3rd edPhiladelphiaSaunders:809-61. [Google Scholar]
[37]. Talmud PJ, Hawe E, Miller GJ, Humphries SE, Non-fasting apolipoprotein B and triglyceride levels as a useful predictor of coronary heart disease risk in middle-aged UK menArterioscler Thromb Vasc Biol 2002 22:1918-23. [Google Scholar]