Patients with liver cirrhosis are believed to be at increased risk of mortality and morbidity after surgery [1]. Deciding whether patients with cirrhosis are fit to undergo surgery is a common clinical dilemma. Not only do the complications of cirrhosis, such as coagulopathy, thrombocytopenia, varices and ascites increase the difficulty and risk of the surgical procedure directly, but general anaesthesia and abdominal incisions may lead to new or worsening hepatic decompensation [2]. Many risk- factors have been identified to be associated with poor outcomes, including intra-operative blood transfusion, low albumin level, abnormal coagulation, ascites, gastrointestinal bleeding, biliary surgery, urinary tract infection, pulmonary failure, emergency surgery and Child-Turcotte-Pugh (CTP) score [3–5].
Two risk stratifications have been widely used to evaluate the peri-operative risk of patients with liver cirrhosis. These are CTP and End-stage Liver Disease (MELD) scores. The CTP score was developed to predict mortality after portacaval shunt surgery, but it has since been used to predict peri-operative mortality rates for patients undergoing hepatic and non- hepatic intra-abdominal surgeries. Patients with CTP Class A are estimated to have a 10% mortality rate after abdominal surgery. That mortality rate increases to 30%-31% for CTP Class B and 76%-82% for CTP Class C [6]. Telem and co-workers demonstrated lower mortality rates (CTP A 2%, CTP B 12%, CTP C 12%) when surgeries were performed at hepatology and liver transplantation specialized institution [7]. However, the CTP scoring system has been challenged for its ambiguity and inter-observer variability because it includes subjective parameters (e.g., degree of ascites and encephalopathy). Additionally, patients within a given class are not homogeneous but also not distinctive, features for which it has also been criticized [8].
The MELD score was originally developed to predict short-term mortality for patients undergoing Transjugular Intrahepatic Portosystemic Shunt (TIPS) placement. It has since been adopted as the tool to prioritize patients with cirrhosis for liver transplantation [9].
Teh et al., performed a retrospective, multivariate analysis that showed among patients with cirrhosis undergoing multiple types of major surgeries, the MELD but not the CTP score predicted increased mortality at 30, 90 days and 1 year, and over the long-term [10].
The debate on the best method and the best individual parameter for risk stratification is still ongoing. MELD scoring system has not been used adequately to evaluate surgical risk in Egyptian patients with liver cirrhosis undergoing non-hepatic surgeries under general anaesthesia. The main aim of this study was to evaluate the value of MELD scoring system as compared to CTP score for prediction of 30-day post-operative mortality in patients with HCV- related liver cirrhosis undergoing non-hepatic surgery under general anaesthesia.
Materials and Methods
This study was conducted on 80 Egyptian patients admitted at Aim Shams University Hospitals, Cairo, Egypt; during the period from May 2014 to November 2015. A prospective analysis was done for clinical and laboratory data of all subjects for this case-control study. Patients with HCV- related liver cirrhosis who were candidates for non-hepato-billiary surgeries (i.e., appendectomy, hernioplasty, subtotal thyroidectomy, etc.) under general anaesthesia were included in this study.
Patients were divided into two groups as follow:
Group A: Sixty patients with HCV- related liver cirrhosis (diagnosed on the basis of clinical, biochemical and radiological criteria).
Group B: Twenty patients who had no clinical, biochemical or radiological evidence of liver disease who served as a control group. All patients were subjected to the following: history taking and thorough clinical examination, laboratory investigations including: Liver Function Tests (LFT), Prothrombin Time (PT) and International Normalized Ratio (INR), Complete Blood Count (CBC), Serum Alpha Feto Protein (AFP) level, renal function tests, fasting and 2 hours post- prandial blood glucose level, Glycosylated Haemoglobin A1c (HbA1c), urine analysis, Erythrocyte Sedimentation Rate (ESR), C-Reactive Protein (CRP), Thyroid Function Tests (TSH, Free T3, Free T4), Anti -Nuclear Antibody (ANA), Rheumatoid Factor (RF), Hepatitis B Virus Surface Antigen (HBsAg), Human Immunodeficiency Virus (HIV) and Hepatitis C Virus (HCV) antibodies using 3rd generation ELISA technique, ascitic fluid sampling for biochemical, bacteriological and pathological examination, imaging studies including pelvi-abdominal ultrasonography, chest X-ray and Electrocardiogram (ECG).
• Calculation of the pre-operative CTP score [Table/Fig-1] [5]:
Child- Turcotte- Pugh score.
| Parameter | Points assigned |
|---|
| 1 | 2 | 3 |
|---|
| Ascites | absent | Slight | moderate |
| Serum bilirubin | <2 mg/dl | 2-3 mg/dl | >3 mg/dl |
| Serum albumin | >3.5 g/dl | 2.8-3.5 g/dl | <2.8 g/dl |
| Prothrombin time (seconds over control) | <4 | 4-6 | >6 |
| INR | <1.7 | 1.7-2.3 | >2.3 |
| Encephalopathy | none | Grade1-2 | Grade3-4 |
Where Child Score A= 5-6, B=7-9 and C=10-15
Calculation of the pre-operative MELD scores using the following formula [11]: MELD = [0.957 x log (creatinine) + 0.378 x log (bilirubin) +1.12 x log (INR) +0.643] x 10.
Patients were followed up during the 30-day post-operative period as regards: clinical examination, laboratory investigations including CBC, LFT, PT and INR, renal function tests, urine analysis, CRP and recalculation of CTP and MELD scores. Patients who had any of the following conditions were excluded from the study: patients under the age of 18 years, liver transplant recipients, patients who were candidates for hepato-billiary surgeries or minor surgical interventions under local and/ or epidural anaesthesia, history of antiviral treatment for HCV and /or HBV infections, advanced cardiopulmonary diseases, acute or chronic kidney disease (including hepato-renal syndrome), uncontrolled thyroid illness, uncontrolled psychiatric illness, any form of acute and/or chronic infection (including spontaneous bacterial peritonitis), morbidly obese patients, patients with liver disease other than HCV- related cirrhosis [i.e., Non-Alcoholic Steato-Hepatitis (NASH), HBV infection, Hemochromatosis, etc.], patients who had any hepatic focal lesions (detected by abdominal ultrasonography) and patients who received any form of treatment for hepatocellular carcinoma.
Statistical Analysis
Data was collected, coded and entered into a personal computer IBM compatible 2.6 GHZ. Data were analyzed with the program Statistical Package for Social Science (SPSS) under windows version 11.0.1. The statistical tests used in this study were: calculation of the mean value, Standard Deviation (SD), Student’s t-test (t), and Chi-square test (χ2). The probability of error (p-value) was expressed as the following:
> 0.05: non-significant, ≤ 0.05: significant, < 0.01: highly significant. Sensitivity, specificity, positive and negative predictive values and the overall accuracy were calculated as follows: sensitivity = true positive/ true positive+ false negative, specificity= true negative/true negative+ false positive, positive predictive value = true positive/ true positive+ false positive, negative predictive value = true negative/true negative +false negative, accuracy= true positive +true negative/ all cases examined. The overall diagnostic performance of a test was assessed by Receiver-Operating Characteristics (ROC) curve analysis.
Results
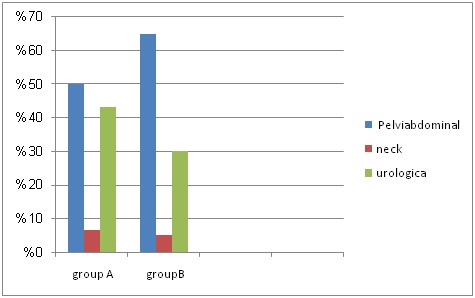
Most of Group A patients were males (63.3%) and the mean age of this group was 50 ± 12.2 years. The majority of Group B patients were also males (60%) with a mean age of 45.1 ± 8.7 years. Insignificant differences were found between both groups as regards gender and type of surgeries [pelvic-abdominal (i.e., strangulated paraumbilical hernia, jejunal fistula, haemorrhagic pelvic cyst, ilio-transverse anastomosis for Crohn’s disease), neck (i.e., hyperparathyroidism, large multinodular goitre), urological (i.e., ruptured bladder secondary to pelvic trauma, cystocele with stress incontinence, haematuria secondary to bladder papilloma)] [Table/Fig-2]. The statistical differences between both groups regarding laboratory investigations are shown in [Table/Fig-3].
Comparison between both groups regarding type of surgeries. Comparison was done using Chi-square test (χ2); p-value = 0.5 (not significant).
Comparison between both groups as regards laboratory investigations. Comparison was done using Student’s t-test (t); p-value < 0.05 (significant). SD: Standard Deviation, ALT: Alanine aminotransferase, AST:Aspartate aminotransferase.
| Group AMean ±SD | Group BMean±SD | t | p-value |
|---|
| ALT | 49.1±36.3 | 30.9±9.5 | 2.7 | 0.007 |
| AST | 55.5± 39.4 | 32.0±9.8 | 3.1 | 0.002 |
| Total Bilirubin | 1.6±1 4 | 0.6±0.3 | 3.2 | 0.001 |
| Serum Albumin | 3.1± 0.6 | 3.8±0.2 | 6.7 | 0.000 |
| Serum Creatinine | 1.0±0.8 | 0.6±0.2 | 2.9 | 0.004 |
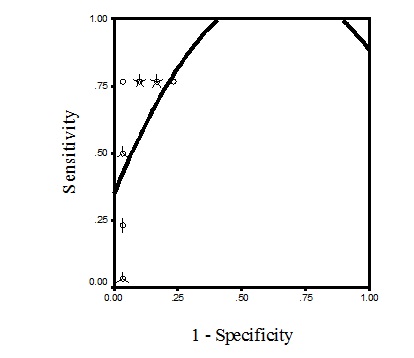
ROC curve analysis was applied for detection of the best cut-off value of MELD score for detection of post-operative mortality. The highest sensitivity and specificity (100% and 76% respectively) for detection of post-operative mortality was detected at a MELD score of 13.5 [Table/Fig-4].
ROC curve analysis for detection of the best cut-off point of MELD score for prediction of post-operative mortality. Area under the curve ROC curve is 0.91.
A highly significant higher percentage of MELD score (>13.5) was found among Child C patients [Table/Fig-5].
Comparison between Child and MELD scores. Comparison was done using Chi-square test (χ2); p-value <0.05 (significant); No. : Number.
| MEDL <13.5 | MELD >13.5 | χ2 | p-value |
|---|
| No. | % | No | % |
|---|
| Child A | 23 | 82.1 | 5 | 17.9 | 13.6 | 0.001 |
| Child B | 15 | 55.6 | 12 | 44.4 |
| Child C | 0 | 0.0 | 5 | 100.0 |
While all patients of Group B survived the post-operative period, four hepatic patients in Group A passed away. A significant higher mean MELD score was found among deceased patients [Table/Fig-6]. Also, a highly significant higher percentage of mortality was found among Child C patients [Table/Fig-7].
Post-operative mortality and MELD score. Comparison was done using Student’s t-test (t); p-value < 0.05 (significant); SD: Standard Deviation.
| MELDMean±SD | t | p-value |
|---|
| Living patients | 12.9±5.4 | 13.6 | 0.001 |
| Deceased patients | 19.7±5.3 |
Post-operative mortality and CTP score. Comparison was done using Chi-square test (χ2); p-value <0.05 (significant); No. : Number.
| Living patients | Deceased patients | χ2 | p-value |
|---|
| No. | % | No | % |
|---|
| Child A | 28 | 100.0 | 0 | 0.0 | 25.2 | 0.00 |
| Child B | 26 | 96.3 | 1 | 3.7 |
| Child C | 2 | 40.0 | 3 | 60.0 |
Significant prediction of post-operative mortality was detected with each point increase in MELD score in logistic regression model (14% higher increase in relative risk of post-operative mortality with each point increase in MELD score above 13.5) [Table/Fig-8].
Logistic regression model of MELD score for detection of post-operative mortality. Dependent variable is mortality and independent variable is MELD score.
| p-value | OR | 95% CI |
|---|
| MELD score | 0.03 | 1.14 | 1.01-1.28 |
CTP score had a sensitivity of 75%, a specificity of 96.4%, a positive predictive value of 60% and a negative predictive value of 98.2% and an overall accuracy of 95% for prediction of post-operative mortality in patients with HCV-related liver cirrhosis. On the other side and at a cut-off value of 13.5, MELD score had a sensitivity of 100%, a specificity of 64.0%, a positive predictive value of 16.6%, and a negative predictive value of 100% and an overall accuracy of 66.6% for prediction of post-operative mortality [Table/Fig-9].
Sensitivity and specificity of child and MELD scores in detection of post-operative mortality; No. : Number
| Group A | Living patients | Deceased patients |
|---|
| No. | % | No. | % |
|---|
| Child A and B | 54 | 96.4 | 1 | 25.0 |
| Child C | 2 | 3.6 | 3 | 75.0 |
| MELD Score<13.5 | 36 | 60.0 | 0 | 0.0 |
| MELD Score> 13.5 | 20 | 33.3 | 4 | 6.6 |
A statistically highly significant reduction in MELD score was detected after surgery [Table/Fig-10]. On the other hand, the low Kappa value (0.41) indicated an inconsistent result in the comparison between CTP scores before and after surgery [Table/Fig-11].
MELD score before and after surgery. Comparison was done using Student’s t-test (t); p-value < 0.05(significant); SD: Standard Deviation.
| Before surgeryMean±SD | After surgeryMean±SD | t | p-value |
|---|
| Group A | 12.9±5.4 | 11.7±3.3 | 2.6 | 0.009 |
CTP score before and after surgery. Comparison was done using Chi-square test (χ2); p-value <0.05 (significant); No. : Number, Kappa value = 0.41
| After surgeryBefore surgery | Child A | Child B | Child C | χ2 | p-value |
|---|
| No. | % | No | % | No | % |
|---|
| Child A | 22 | 78.6 | 6 | 21.4 | 0 | 0.0 | 19.2 | 0.001 |
| Child B | 8 | 30.0 | 15 | 57.7 | 3 | 11.5 |
| Child C | 0 | 0.0 | 1 | 50.0 | 1 | 50.0 |
Discussion
The number of patients with cirrhosis who require surgery is on the rise. Despite advances in antiviral treatment, the prevalence of HCV-related cirrhosis continues to increase. On the other hand, the number of medications aimed at improving survival of patients with cirrhosis has been increasing. Therefore, it can be expected that a growing number of patients with cirrhosis will undergo surgery. Some reports have stated that as many as 10% of patients with advanced cirrhosis will undergo surgery in the last two years of their lives [12]. Patients with cirrhosis are at high-risk for morbidity and mortality in the post-operative period due to the stress of surgery and the effects of anaesthesia. Furthermore, decompensated cirrhosis increases the risk of post-operative complications (e.g., acute hepatic failure, infections, bleeding, poor wound healing and renal dysfunction). Assessing mortality risk in patients with cirrhosis is a challenging but important endeavour [13].
The main focus of this study was to evaluate the value of MELD score, as compared to CTP score, as a predictor of 30-day post-operative mortality in patients with HCV-related cirrhosis undergoing non-hepatic surgery.
The current study revealed higher sensitivity but lower specificity of MELD score, as compared to CTP score, for prediction of post-operative mortality in patients with HCV- related cirrhosis. In contrast to this finding Suman et al., found CTP score to be the best predictor of 30-day post-operative mortality in patients with decompensated cirrhosis, Child-Pugh score >7 was found to have a sensitivity of 86% and a specificity of 92% for prediction of post-operative mortality, with a negative predictive value of 97% and a positive predictive value of 67% [9]. Rahimi et al., findings were in agreement with the current study, Rahimi and co workers found the best cut-off point for predicting post-operative mortality in patient with decompensated cirrhosis to be 8 for CTP and 13.67 for MELD [14]. The sensitivity and specificity for CTP was 74% and 67%, respectively and 74% and 58%, for MELD scoring system.
In this study, the 30-day post-operative mortality was found to be 6.7% in the total cohort of the cirrhotic patients. The mortality rate identified in this study was comparable to other published reports. Patrick et al., reported an in-hospital total mortality rate of 16.4% in a retrospective review of 140 patients with decompensated cirrhosis undergoing surgical procedures [15]. Ziser and co-workers reported an in-hospital mortality rate of 9.8% in a retrospective study of 733 patients with liver cirrhosis undergoing surgical procedures [16]. A higher value was reported by Rice and coworkers who found a 30-day mortality rate of 28% in a smaller cohort of patients with cirrhosis undergoing non-hepatic surgeries [17]. The discrepancy in mortality rates across different studies could be partly explained by selection bias towards patients with less severe decompensated cirrhosis. The current study avoided such a selection bias as the distribution of MELD score included a broad sample of patients with decompensated cirrhosis.
Approximately 50% of the patients of this study underwent pelvic-abdominal surgeries. The 30-day mortality for this subgroup of patients was in line with the reported values of Rice et al., [17]. Cirrhotic patients undergoing abdominal surgeries represent a critical group of patients due to increased surgical complexity, longer anaesthesia time, higher complication rates, and longer recovery times.
The results of the present study strongly highlight the importance of both the objective assessment obtained from MELD score and a categorical system with subjective parameters, such as the CTP system, in individually assessing cirrhotic patients for post-operative mortality risk. MELD score offers a simple, objective, easily used tool that avoids the subjectivity of CTP classification, making for more uniform and precise risk assessment. However, MELD score has notable limitations. Although it uses objective parameters, these variables can be labile, causing dramatic changes in MELD score as a result of infection, medication side-effects, bleeding, dehydration and fluid shifts. Fluid changes are of at most importance, as serum creatinine is a major determinant of mortality. Also, a common problem with MELD, CTP and other risk stratifications is determining the best time for risk assessment [18]. Further studies are needed to determine if therapeutic correction of MELD score parameters can lead to any changes in post-operative mortality rates.
Limitation
The current study had a number of weaknesses. Because the indications and priority (i.e., emergency versus elective surgeries) for various surgical procedures were so varied across the spectrum of surgical diseases in the cirrhotic patients, it is not possible to make a recommendation for an absolute cut-off point where surgery is “too risky” based on the MELD and/or CTP scores. Certainly, the higher MELD score values indicate higher surgical risk (especially among Child C patients) while the lower MELD score rates impart some sense of safety, especially when the MELD score is less than 13.5. Second, it was not possible to determine the number of patients with HCV-related cirrhosis who were considered for surgical intervention in whom no surgical procedures were performed. Third, because of the small sample size, especially in the sub-group analyses, the possibility of type II error is significant. Further validation of the MELD and CTP scores in large surgical datasets is needed to answer these concerns.
Conclusion
MELD score proved to be more sensitive but less specific than CTP score for prediction of 30 days post-operative mortality. CTP and MELD scores may be complementary rather than competitive in predicting post-operative mortality in patients with HCV-related liver cirrhosis.
Conflict of Interest: There is no conflict of interest regarding this manuscript.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not for profit sectors.
Compliance with Ethical Standards: All procedures performed were in accordance with the ethical standards of Aim Shams University Research Committee and with the 1964 Declaration of Helsinki and its later amendments. Informed consent was obtained from all individual participants included in the study.