A Case of Interosseous Membrane Calcification
Kannan Rajendran1, Shrilakshmi Swarathmika2, Prasanna Karthik Suthakaran3, Warun Kumar Muthupillai Rathinam4, Sivasubramanian Kandasamy5
1 Professor, Department of General Medicine, Saveetha Medical College and Hospital, Saveetha University, Saveetha Nagar, Thandalam, Chennai, Tamilnadu, India.
2 CRRI, Department of General Medicine, Saveetha Medical College and Hospital, Saveetha University, Saveetha Nagar, Thandalam, Chennai, Tamilnadu, India.
3 Assistant Professor, Department of General Medicine, Saveetha Medical College and Hospital, Saveetha University, Saveetha Nagar, Thandalam, Chennai, Tamilnadu, India.
4 Assistant Professor, Department of General Medicine, Saveetha Medical College and Hospital, Saveetha University, Saveetha Nagar, Thandalam, Chennai, Tamilnadu, India.
5 Professor, Department of General Medicine, Saveetha Medical College and Hospital, Saveetha University, Saveetha Nagar, Thandalam, Chennai, Tamilnadu, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Kannan Rajendran, Professor, Department of General Medicine, Saveetha Medical College and Hospital, Saveetha University, Saveetha Nagar, Thandalam, Chennai–602 105, Tamilnadu, India.
E-mail: endork@yahoo.com
Fluorosis, Metastatic calcification, Renal Osteodystrophy
A 69-year-old male presented with complaints of progressive easy fatigability, low back ache and pain in the right forearm for the past one year. He had associated swelling of legs for the past three months and had noticed a decrease in his urine output. He never had any other associated joint pains, burning micturition or oral ulcers. He was hypertensive and was on medical treatment, with no other co-morbid illnesses. Examination revealed pallor and bilateral pitting pedal oedema. Vitals were within normal limits. Systemic examination was unremarkable. Musculoskeletal examination revealed bony tenderness over the L3 – L4 spine with no obvious swelling and tenderness over the lower half of the right forearm. There were no visible deformities.
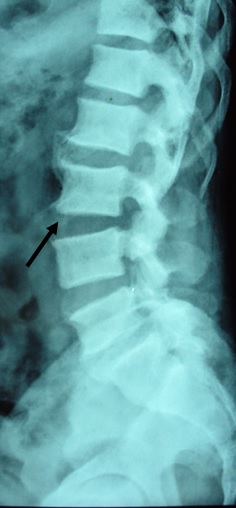
Investigations revealed anemia, elevated urea and creatinine with normal electrolytes. ESR was elevated. Rheumatoid factor, anti-CCP, ANA and CRP were negative. His biochemical investigations revealed low calcium (8.78mg/dL, N:8. –10.2 g/dL) and low vitamin D3 levels (13ng/mL, N:15–75ng/mL) while serum phosphorus (4.2mg/dL, N:2.5–4.3 mg/dL) and alkaline phosphatase (143IU/L, N:33–96IU/L) were elevated. Serum parathormone level (intact) was elevated (84pg/mL, N:8–51pg/mL). Urine examination revealed moderate (2+) proteinuria. Ultrasonogram revealed bilateral contracted kidneys which was suggestive of chronic kidney disease. X-ray lumbosacral spine [Table/Fig-1] revealed increased density of L2, L3 and L4 vertebral bodies with marginal osteophytes and X-ray right forearm [Table/Fig-2] showed interosseous membrane calcification. There was no evidence of vascular or pulmonary calcification. ECG, 2D echocardiogram and other baseline investigations were within normal limits.
X-Ray of the lumbosacral spine showing diffuse osteosclerosis and osteophytes (arrow).
X-Ray of the right forearm showing interosseous membrane calcification (arrow).

The diagnosis of Chronic Kidney Disease (CKD) was made on the basis of elevated serum creatinine, proteinuria and shrunken kidneys on ultrasound. The presence of interosseous membrane calcification in the background of CKD lead to the diagnosis of Renal Osteodystrophy (ROD) in this patient. He was treated conservatively with salt and fluid restriction, oral frusemide 40mg twice daily, oral vitamin D3 60k units once weekly for 6 weeks and oral calcium carbonate 500mg once daily. His oedema improved after one week of hospital stay and he was discharged. He was subsequently lost to follow-up.
Metastatic calcification is a form of pathological calcification that may occur in otherwise normal tissues in the presence of hypercalcemia. Soft tissue calcification is one form of metastatic calcification. The common sites of involvement are stomach, kidney, lungs and heart with the pulmonary parenchyma being the most susceptible area for calcification [1]. Interosseous membrane calcification is an unusual site for metastatic calcification. The causes of interosseous membrane calcification are fluorosis, X linked hypophosphatemic rickets, osteogenesis imperfecta type V, ROD, bone metastasis, Paget’s disease, osteopetrosis, seronegative spondyloarthritis [2,3].
Fluorosis, a chronic metabolic bone disease, occurs due to long term ingestion of excess amount of fluoride, is diagnosed by osteophytosis, osteosclerosis and ligamentous calcification [2–4]. The dental changes (mottling of teeth) and elevated urine fluoride levels in addition to the presence of membranous calcification point towards a diagnosis of fluorosis which was not evident in our patient. Fluorosis usually presents commonly with neurological manifestations like neuropathy and myelopathy [2,3].
The absence of classical bony changes excludes the diagnosis of osteopetrosis, Paget’s disease and osteogenesis imperfecta in our patient. The presence of CKD with hyperphosphatemia and elevated PTH points towards the diagnosis of ROD in our patient. In patients with CKD, the compensatory response to maintain the calcium homeostasis gradually fails, resulting in altered serum levels of calcium, phosphorus and parathormone. It also leads to disturbances in bone remodeling and mineralization and extraskeletal calcification in soft tissues and arteries. These abnormalities are interrelated in both the pathophysiology of the disease and the response to treatment [5].
ROD is a term that encompasses the various bony abnormalities that occur in end stage renal disease. The disease is classified into osteitis fibrosa, adynamic bone disease, osteomalacia, mixed disease and mild disease on the basis of their histological changes. In patients with osteitis fibrosa, secondary hyperparathyroidism is seen while parathyroid hormone suppression is seen in patients with adynamic bone disease [6].
The treatment of ROD is conservative with low phosphate (800–1000mg/day) and low protein diet with phosphate binders to reduce the circulating phosphate to a target of about 3.5 to 5.5 mg/dL in patients undergoing dialysis. Serum calcium should be maintained between 8.4 to 10mg/dL and hypercalcaemia should be treated when the values exceed 10.2mg/dL. Also in patients having intact parathormone levels greater than 300pg/ml, treatment with calcitriol should be initiated to suppress the secondary hyperparathyroidism [7].
This report presents the finding of heterotopic calcification of the interosseous membrane which is a rare manifestation of end stage renal disease. ROD, occurs in patients with end stage renal disease due to the altered calcium and phosphate metabolism, which leads to heterotopic calcification. ROD is a major cause of morbidity in patients with CKD and is amenable to treatment if identified early.
[1]. Kumar V, Abbas AK, Aster JC, Robbins and Cotran Pathologic Basis of Disease 2015 9th edElsevier [Google Scholar]
[2]. Wang Y, Yin Y, Gilula LA, Endemic fluorosis of the skeleton: radiographic features in 127 patientsAm J Roentgenol 1994 162:93-98. [Google Scholar]
[3]. Kumar R, Balachandran K, Kamalanathan S, A unique cause of interosseous membrane calcificationBMJ Case Rep 2015 [Google Scholar]
[4]. Lantz O, Jouvin MH, De Vernejoul MC, Druet P, Fluoride-induced chronic renal failureAm J Kidney Dis 1987 10:136-38. [Google Scholar]
[5]. Moe SM, Sprague SM, Chronic Kidney Disease – Mineral Bone Disorder. In: Taal MW, Cherlow GM, Marsden PA, Skorecki K, Yu ASL, Brenner BM editorsBrenner & Rector’s The Kidney 2012 9th edElsevier [Google Scholar]
[6]. Hruska KA, Teitelbaum SL, Renal Osteodystrophy–ReviewN Eng J Med 1995 333(3):166-74. [Google Scholar]
[7]. Indian Society of Nephrology. Treatment of renal osteodystrophy in chronic kidney patients on dialysis. Indian J Nephrol. 2005;15 Supplement 1:S65-S71. Available from http://www.medind.nic.in/iav/t05/s1/iavt05s1p65.pdf [ Accessed 20th June 2016] [Google Scholar]