Anaesthetic Management of a Case of Down’s Syndrome with Achalasia Cardia
Neeta Santha1, Madhusudan Upadya2, Sravanthi Vishwanatham3
1 Assistant Professor, Department of Anesthesiology, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
2 Professor, Department of Anesthesiology, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
3 Post Graduate, Department of Anesthesiology, Kasturba Medical College, Manipal University, Mangalore, Karnataka, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Santha Neeta, Assistant Professor, Department of Anesthesiology, Kasturba Medical College, Mangalore-575001, Karnataka, India.
E-mail: drneetas@yahoo.com
Achalasia cardia is a disorder of the gastrointestinal tract characterized by dilatation of the oesophagus and collection of food and fluids in the oesophagus leading to massive regurgitation and aspiration of gastric contents. Down’s syndrome has multisystem effects which can also present as difficult airway. Here, we present a case of a 14-year-old girl, a case of Down’s syndrome with Achalasia cardia and mitral valve prolapse posted for Heller’s cardiomyotomy. Anaesthetic concerns were difficult airway due to Downs’s syndrome, massive aspiration risks of Achalasia cardia and haemodynamic instability due to mitral regurgitation. In spite of proper preparation of the patient there was massive regurgitation of oesophageal contents during intubation which was managed successfully. Haemodynamic changes due to mitral valve prolapse also had to be taken care of during the intraoperative period. Postoperative period was uneventful and the child was discharged after one week.
Aspiration, Heller’s cardiomyotomy, Mitral valve prolapse
Case Report
A 14-year-old female child, weighing 16 kilograms, known case of Down’s syndrome posted for Heller’s cardiomyotomy. A thorough pre-anaesthetic evaluation was done. Child was irritable and poorly built. Airway examination revealed receding mandible, high arched palate, and Mallampatti grade 3. Auscultation of lung fields revealed occasional crepitations. A pan systolic murmur was heard in the mitral area.
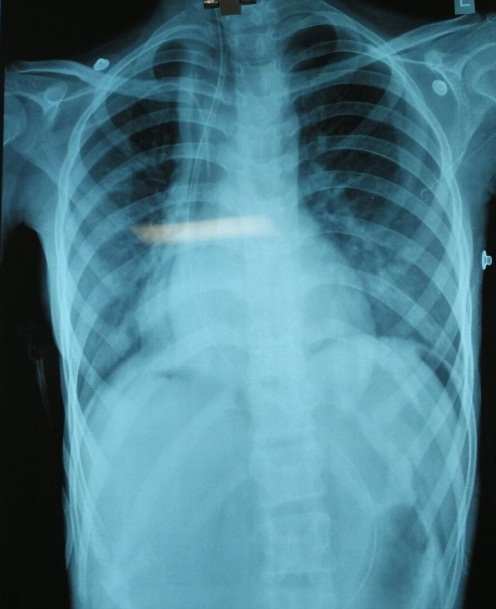
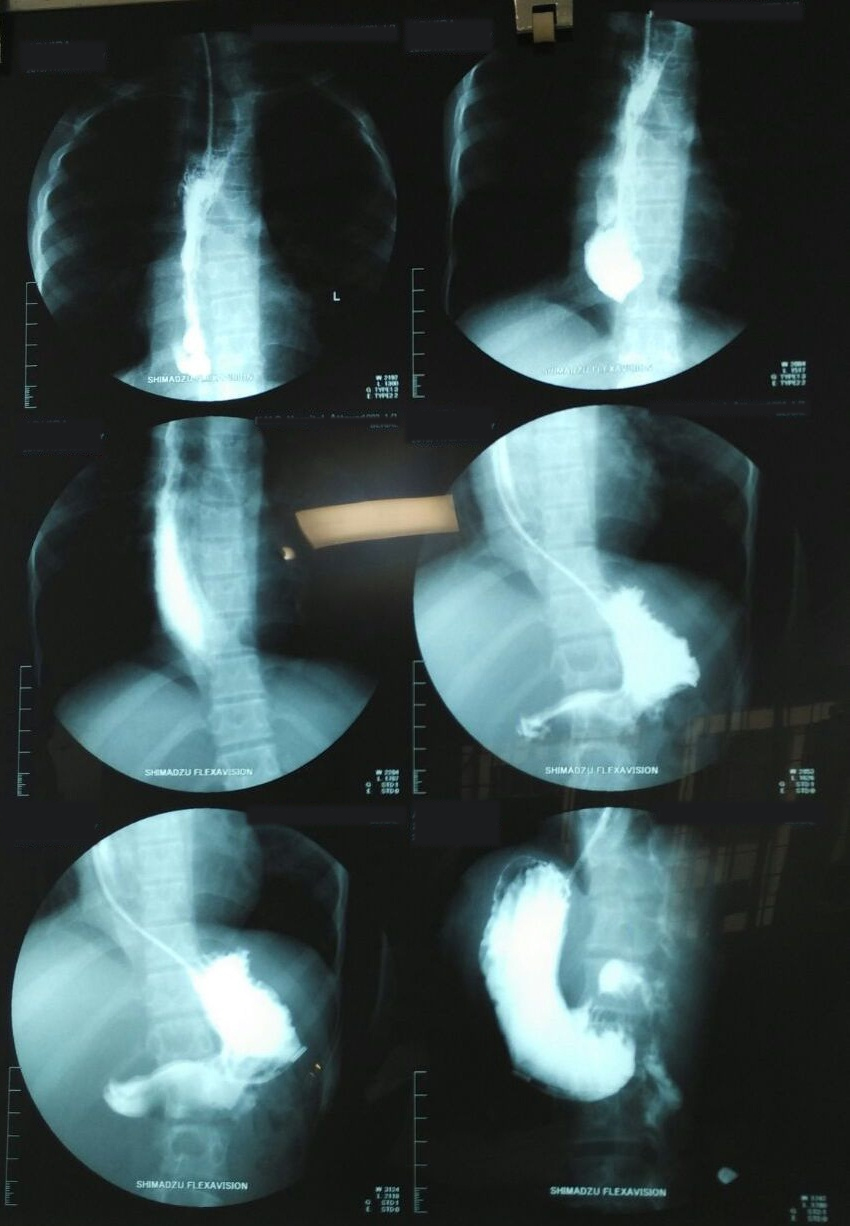
A 2D echo revealed mitral valve prolapse with mitral regurgitation with normal LV function and no pulmonary hypertension. Chest X-ray revealed dilated oesophagus [Table/Fig-1]. Computerized tomography of thorax and barium swallow revealed entire thoracic oesophagus grossly dilated and distended with fluid and food particles [Table/Fig-2]. This patient was diagnosed to have Achalasia cardia and was planned for Heller’s cardiomyotomy. It was an anticipated difficult intubation situation in view of Down’s syndrome.
Chest X-ray showing the dilated oesophagus
Computerized tomography of thorax and barium swallow.
The patient was shifted to the operation room and monitors connected. Acid aspiration prophylaxis was given. Ryle’s tube was inserted and oesophagus was decompressed. The equipments for difficult airway were kept ready. Our plan was to go ahead with rapid sequence induction.
The child was preoxygenated with 100% Oxygen for 3 minutes. She was premedicated with 0.2mg midazolam and 20μg fentanyl. Rapid sequence induction done with Ketamine 20mg, Propofol 20mg and Succinyl choline 20mg along with application of cricoids pressure. Under direct laryngoscopic vision, bilateral vocal cords were visualized with difficulty as the child had enlarged glossoepiglottic folds and enlarged hanging epiglottis. Trachea was intubated with 5mm Cuffed Oral Endotracheal Tube (COETT) and fixed at 17 centimeters after confirming bilateral air entry. We made sure that cuff was inflated immediately after intubation. Cricoid pressure was released.
A 250ml of foul smelling collected secretions regurgitated out of the oesophagus. Immediately patient was positioned in right lateral position and secretions were suctioned. We found it difficult to fix the tube as the secretions were pouring out. Auscultation of the chest revealed mild crepitations. Sterile ET tube suctioning was done. Small volume of aspirate came out suggesting micro aspirations around the tube cuff.
Atracurium 10 mg was given. Intra-operatively patient was maintained on O2: N2O (1:1) and sevoflurane 2%. Fentanyl was supplemented as required. Under aseptic precautions, left dorsalis pedis arterial line was secured. Right sided subclavian central line also was secured. Heart rate was around 100 beats per minute and blood pressure was maintained around 90 to 120mmHg systolic. After the procedure incision site was infiltrated with 0.25% Bupivacaine. Intravenous paracetamol was given. Patient was reversed with neostigmine 1mg and glycopyrrolate 0.2mg. When child was fully awake, responding to commands, the trachea was extubated.
Post extubation the heart rate increased to 160 beats per minute and blood pressure dropped to 70mmHg systolic. Intravenous lignocaine and fentanyl boluses were given. Heart rate came down to 120 beats per minute and blood pressure increased to 100mmHg systolic. Central Venous Pressure (CVP) measured around 6 mm Hg. IV fluids were given to bring up the blood pressure as there was no intraoperative blood loss.
Postoperatively, intravenous fentanyl infusion was started at 10μg/h. After 1 day, fentanyl infusion was stopped. Child was haemodynamically stable. The child recovered fully without any cardiovascular or respiratory complications and was discharged after one week.
Discussion
Achalasia cardia is an uncommon disorder characterized by degeneration of nerve cells in the oesophagus. This can lead to decreased peristaltic movements. Lower oesophageal sphincter remains persistently contracted and oesophagus starts to dilate and large volumes of food and saliva can accumulate in the dilated oesophagus. Other symptoms include regurgitation of swallowed food and liquid, chest pain, heartburn, a sensation of fullness or a lump in the throat, hiccups and weight loss [1,2].
The incidence of achalasia is about 0.3–11/106 per year and the aetiology is still not completely understood [3]. There are various treatment modalities that include pharmacological therapy, administration of a calcium channel blocker or nitrates [4]. Balloon dilatation, botulinum toxin injection, per oral endoscopic myotomy, laparoscopic cardiomyotomy are some of the surgical modalities [5]. Down’s syndrome is a genetic disorder occurring in 1 in 800 live births [6].
There are not many literatures on achalasia cardia. Our anaesthetic concerns included a possible difficult airway, risk of aspiration and cardiovascular instability due to mitral valve prolapse and mitral regurgitation. These children are at increased risk of gastro oesophageal reflux. So routine acid aspiration prophylaxis and rapid sequence induction is recommended.
These patients are at an increased risk for atlanto axial instability, so care should be taken while positioning during anaesthesia and laryngoscopy. The associated microcephaly, macroglossia, subglottic stenosis and sleep apnea may contribute to the difficult airway; which recommend awake intubation and smaller sized endotracheal tubes. They are prone for recurrent respiratory tract infections [7].
Our patient was a suspected case of difficult airway. The intubation had to be done as quickly as possible as the risk of aspiration was high and the risk of desaturation was also higher due to Lower Respiratory Tract Infection (LRTI). Also, the risks of sudden hypotension associated with rapid sequence induction in a patient with mitral regurgitation should be considered. In our case it took few seconds more than the normal intubation time, as airway anatomy was abnormal.
Application of cricoid pressure is supposed to be protective against gastric regurgitation and aspiration [8]. In our case post intubaton, the moment we released the cricoid pressure there was massive regurgitation of gastric secretions, which happened in spite of nasogastric tube aspiration. Also, there were micro aspirations around the cuff of the tube and audible crepitations.
Thus, in our case whether rapid sequence induction or faster intubation protected the airway from aspiration remains a question. In a paper by Hannuah M et al., in which two cases of achalasia cardia were reported, rapid sequence induction did protect against aspiration in one case, but the other patient had micro aspiration like in our patient. This points to the incomplete aspiration protection that large-volume, low-pressure endotracheal tube cuffs provide [9].
Other options to prevent aspiration in such a scenario includes, pulling the nasogastric tube to the oesophagus and aspirating the contents before paralyzing the patient. Putting a suction catheter into oesophagus and aspirating the contents before anaesthetizing is another option. Intubation can be tried in lateral and head down position also.
Patients with Down syndrome can have acyanotic and cyanotic congenital heart disease. Also, there is an increased risk of mitral valve prolapse and aortic regurgitation in these adolescent and adult populations. Our patient had mitral regurgitation. Intraoperatively the patient was stable. Once patient was reversed there was tachycardia and haemodynamic instability. Tachycardia decreases the regurgitant volume by shortening systole. But also can compromise diastolic filling and cardiac output. Adequate anaesthetic depth, systemic vasodilators, or inodilators may be clinical options; depending on the situation [10]. The tachycardia in our patient could be due to pain which was managed with fentanyl infusion. Once the heart rate settled, the blood pressure too stabilized.
Conclusion
Anaesthetic management in a case of Downs syndrome with multisystem involvement and achalasia cardia is an anaesthetic challenge. Down syndrome itself presents as difficult airway and cricoid pressure makes it worse. The message that requires to be conveyed is that rapid sequence induction and intubation with cuffed endotracheal tube may not be hundred percent protective against aspiration. Thus proper pre anaesthetic pre-paration for difficult airway management and preparedness to do immediate measures to prevent aspiration like lateral position or suctioning should be kept in mind.
[1]. Bhandarkar DS, Salgaonkar H, Sharma P, Achalasia cardiaGI Surgery Annual 2013 20:1-22. [Google Scholar]
[2]. Patel DA, Kim HP, Zifodya JS, Vaez MF, Idiopathic (primary) achalasia: a reviewOrphanet Journal of Rare Diseases 2015 10:89 [Google Scholar]
[3]. Lileswar K, Javid I, Rakesh K, Laparoscopic hellermyotomy for Achalasia cardia—Initial experience in a teaching instituteIndian J Surg 2013 75(5):391-94. [Google Scholar]
[4]. Miyazaki T, Sohda M, Sakai M, Tanaka N, Suzuki S, Yokobori T, Primary oesophageal motility disorders; especially about oesophageal achalasiaThe Japanese Journal of Thoracic Surgery 2011 64(8 Suppl):770-75. [Google Scholar]
[5]. Yang D, Wagh MS, Peroral endoscopic myotomy for the treatment of achalasia: an analysisDiagn Ther Endosc 2013 2013:389596 [Google Scholar]
[6]. Yang Q, Rasmussen SA, Friedman JM, Mortality associated with Down’s syndrome in USA from 1983 to 1997: A population based studyLancet 2002 359(9311):1019-25. [Google Scholar]
[7]. Mark CM, Julie AS, Anaesthetic considerations for patients with Down’s syndromeAANA Journal 2005 73(2):103-07. [Google Scholar]
[8]. Landsman I, Cricoid pressure; indications and complicationsPaediatr Anaesth 2004 14(1):43-47. [Google Scholar]
[9]. Hannallah M, Airway protection during anaesthesia for oesophagogastroduo-dendoscopy in patients with achalasiaJ Anaesthe Clinic Res 2011 4:307 [Google Scholar]
[10]. Nussmeier NA, Valvular heart disease in the patient undergoing noncardiac surgeryIARS review course lecture 2010 :54-59. [Google Scholar]