Paclitaxel Induced Acute ST Elevation Myocardial Infarction: A Rare Case Report
Gautam Rawal1, Sankalp Yadav2, Raj Kumar3
1 Attending Consultant, Respiratory Intensive Care, Max Super Specialty Hospital, Saket, New Delhi, India.
2 General Duty Medical Officer-II, Department of Medicine and TB, Chest Clinic Moti Nagar, North Delhi Municipal Corporation, New Delhi, India.
3 Senior Consultant and Incharge, Respiratory Intensive Care, Max Super Specialty Hospital, Saket, New Delhi, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Gautam Rawal, Flat No. 417, Dhruva Apartments, Plot No. 4, I P Extension, Patparganj, Delhi -110092, India.
E-mail: drgautamrawal@hotmail.com
Paclitaxel, is a frequently used anti-neoplastic agent and is included in various chemotherapy regimens. The life threatening cardio toxicity associated with its use and the still unclear pathophysiology, has limited the use of this drug. Acute myocardial infarction is a rare adverse event associated with this drug. We report a case of acute ST-elevation myocardial infarction induced by paclitaxel infusion in a patient of oesophageal carcinoma who was saved by percutaneous primary intervention. The authors emphasize the awareness of this side effect of Paclitaxel among the clinicians.
Bradyarrhythmia, Chemotherapy, Coronary thrombosis, Oesophageal carcinoma, Taxol
Case Report
A 63-year-old Indian male patient, known case of carcinoma oesophagus (upper one third) diagnosed in 2015, post radiation therapy and now started on chemotherapy, was admitted with complaints of progressively increasing breathing difficulty associated with a dry cough since one month. He was diagnosed to have right sided pleural effusion which was drained and the patient was relieved of his symptoms. The patient had no history of hypertension or diabetes or cardiac illness and his base line Electrocardiogram (ECG) was normal. He was planned for the next Cycle Chemotherapy with Paclitaxel, Carboplatin and 5-fluorouracil. The patient was given premedication with ranitidine, dexamethasone and diphenhydramine. The patient developed acute onset of left-sided chest pain radiating to back associated with diaphoresis, breathlessness and hypotension, just after completion of paclitaxel infusion. On examination, he was conscious, oriented, the heart rate was 40 per minute, blood pressure was 90/40mmHg, respiratory rate was 28 per minute and blood oxygen saturation was 96% on room air, cold and clammy extremities with pale look.
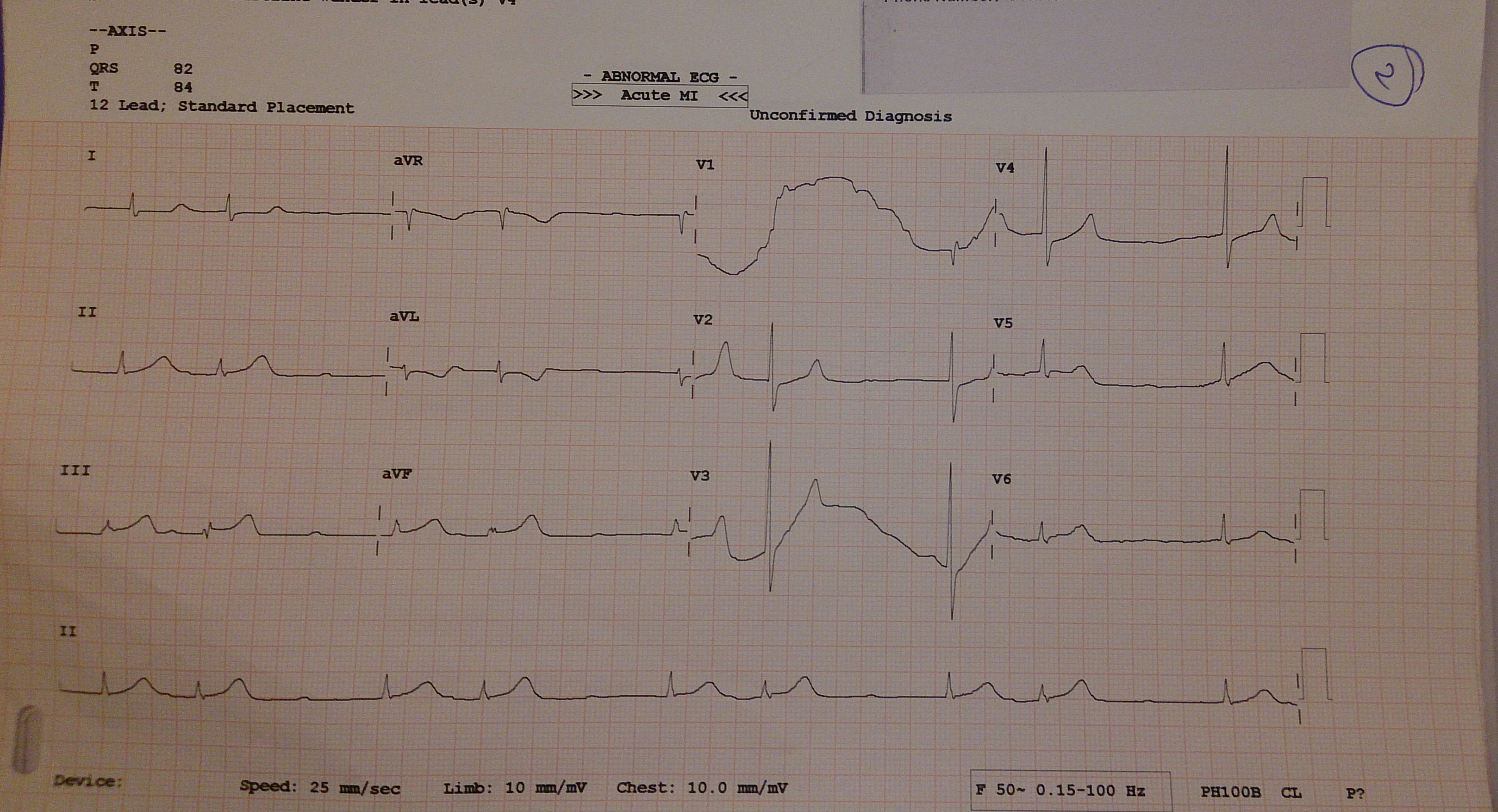
He was started on oxygen and immediately transferred to the Intensive Care Unit (ICU) and initiated on inotropic support with norepinephrine and dopamine. The ECG showed ST elevation in the inferior leads (lead II, III and aVF), bradycardia (HR 40/min) with junctional escape rhythm suggestive of Acute Inferior Wall Myocardial Infarction (AIWMI) [Table/Fig-1]. He was immediately administered intravenous fluids, Ecosprin (300mg) and Clopidogrel (600mg). The troponin t-test was positive. Complete blood count, liver function tests, renal function tests and electrolytes were within normal limits.
ECG showing ST elevation in the inferior leads (lead II, III and aVF), bradycardia (HR 40/min) with junctional escape rhythm s/o acute inferior wall myocardial infarction (AIWMI).
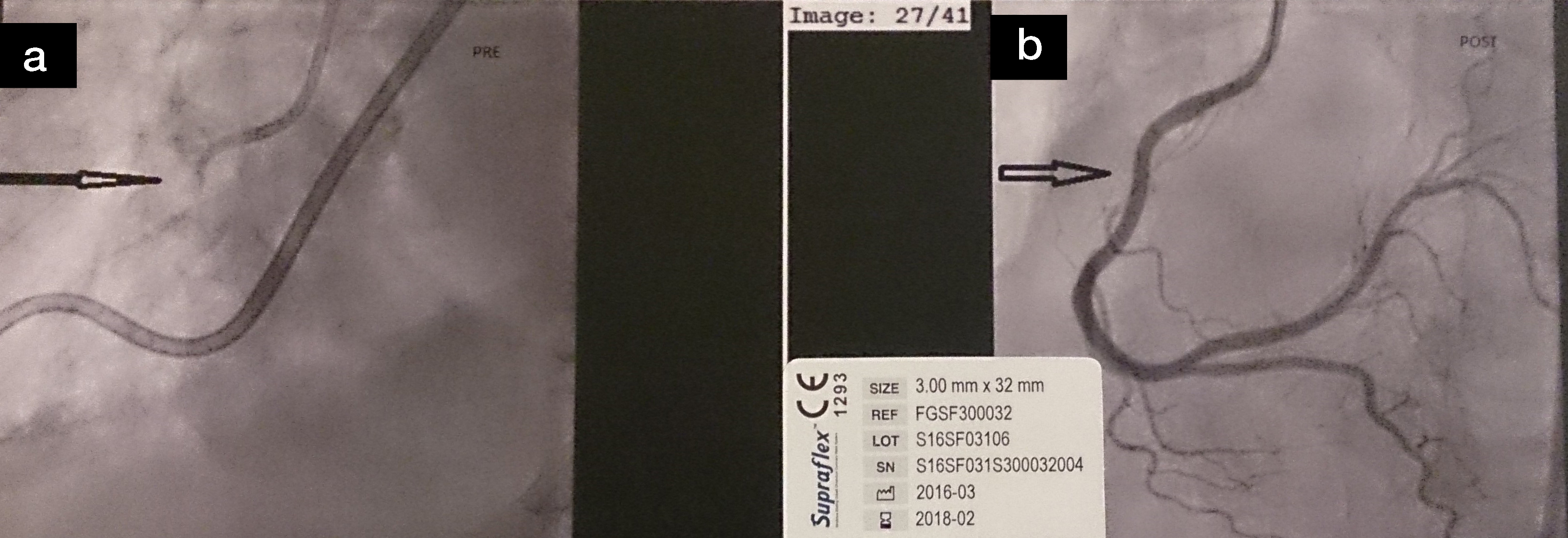
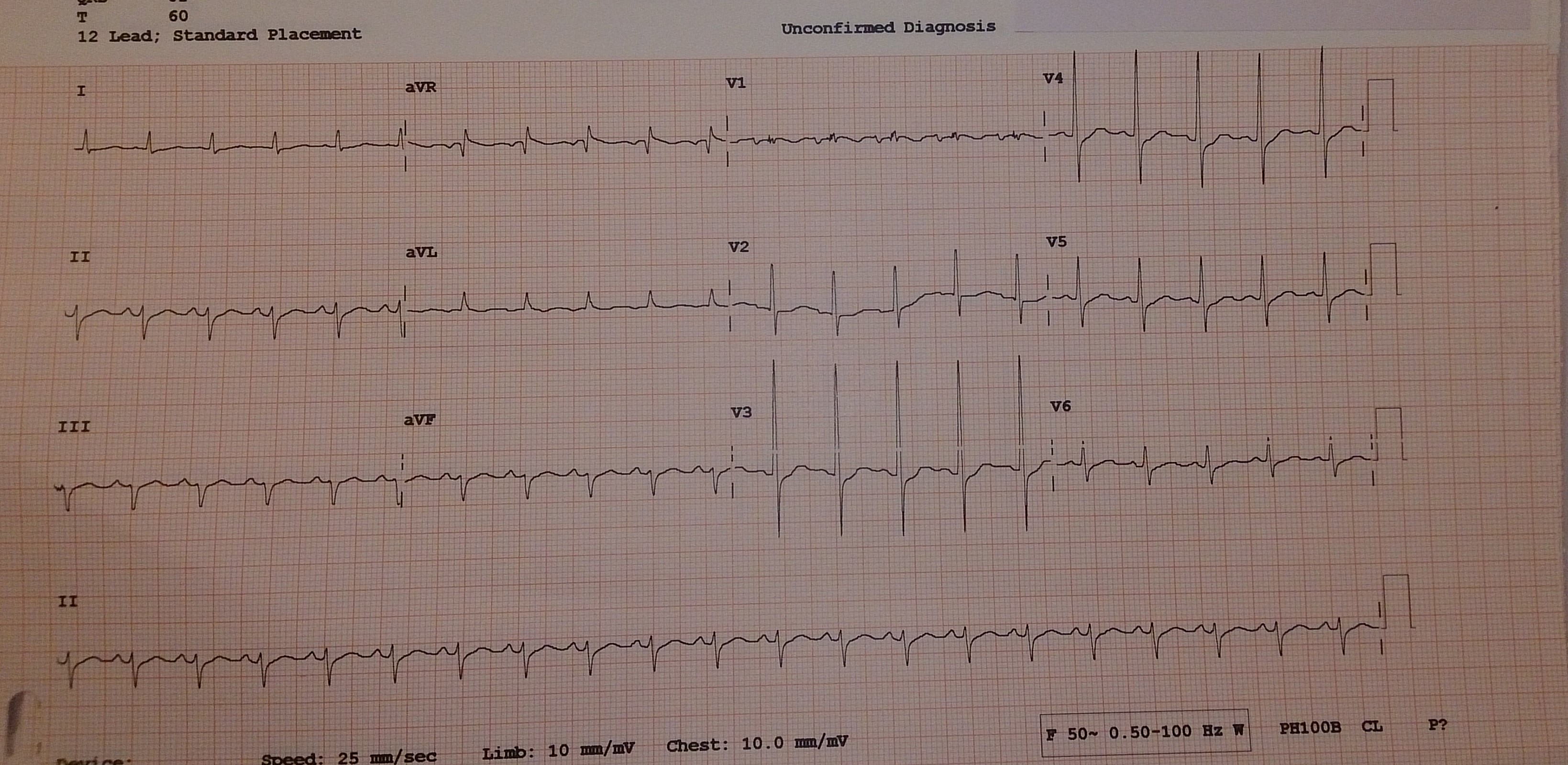
Transthoracic echocardiography showed hypokinesia of the basal inferior wall, posterior wall and the lower and mid interventricular septum, with depressed left ventricular systolic function and a left ventricular ejection fraction of 45%. A diagnosis of AIWMI induced by Paclitaxel was made. It was decided to take the patient immediately for Coronary Angiogram (CAG) for primary Percutaneous Transluminal Coronary Angioplasty (PTCA) and the patient was shifted to catheterization laboratory. His CAG showed 100% block of the proximal Right Coronary Artery (RCA) [Table/Fig-2a], for which stent placement was done. The other coronary arteries showed normal flow. Post procedure, the coronary perfusion improved [Table/Fig-2b], also the ECG changes normalized with normal heart rate and rhythm [Table/Fig-3]. The patient improved symptomatically and his hemodynamics stabilized and inotrope tapered off. He was transferred to the oncology ward from the ICU and planned for further management using second line chemotherapy. An informed consent was obtained for using the clinical images and the details of the case.
(a) Coronary angiography revealing 100% stenosis of proximal RCA (arrow); (b) Post PTCA with stent placement in RCA showing normal flow (arrow).
ECG post PTCA showing reversal of ST changes and normal sinus rhythm.
Discussion
Paclitaxel is an anti-neoplastic agent commonly and widely used and approved for the treatment of various malignancies, including oesophageal cancer, breast, ovarian and other cancers [1]. Though an effective drug, it is not devoid of side effects, which include bone marrow suppression, alopecia, polyneuropathy and cardiac toxicities [2,3]. The major concern among the cardiac toxicities is the life threatening myocardial infarction, which has been reported in less than four percent of the patients receiving this drug, and only nine such cases have been reported in the literature in the author’s knowledge [3–5]. Other cardiac abnormalities include acute or sub-acute bradycardia, atrioventricular conduction blocks, atrial or ventricular arrhythmias, negative inotropic effect and congestive cardiac failure reported in 0.5% of the patients [2–6].
The exact mechanism which leads to myocardial infarction while receiving Paclitaxel is not clearly described and understood in the literature. Various pathophysiologies have been described in the literature, including coronary artery vasospasm (histamine-mediated coronary vasospasm in response to Cremophor EL (derivative of castor oil) which is the suspension medium, or vasospasm due to increased intracellular calcium concentrations or Paclitaxel-associated allergic myocardial infarction) [3,5–7]. Park et al., in their case postulated that Paclitaxel can itself cause coronary artery thrombosis [8].
The presented case describes a patient who developed acute MI due to possible acute coronary thrombus formation as described by Park et al., as the flow in the other coronary arteries was normal with no visible plaques [8]. The other cause could have been due to coronary vasospasm superimposed on a previously undiagnosed obstructive coronary lesion leading to acute myocardial infarction.
Thus, the potential cardio toxic effects of the chemotherapeutic agents should be considered and recognized before and during infusion of these drugs, especially in patients with possible or known cardiac disease [9].
Conclusion
Paclitaxel is a commonly used chemotherapeutic agent. Myocardial infarction secondary to Paclitaxel infusion is a rare, but known life-threatening adverse effect and caution with proper observation should be exercised during its infusion, even in a patient with no previous cardiac risk factors. Further studies are required to know the exact mechanism of its cardio toxicity, so that preventive steps can be taken beforehand.
[1]. Ilson DH, Oesophageal cancer chemotherapy: Recent AdvancesGastrointest Cancer Res 2008 2(2):85-92. [Google Scholar]
[2]. Schlitt A, Jordan K, Vordermark D, Schwamborn J, Langer T, Thomssen C, Cardiotoxicity and oncological treatmentsDtsch Arztebl Int 2014 111(10):161-68. [Google Scholar]
[3]. Shah K, Gupta S, Ghosh J, Bajpai J, Maheshwari A, Acute non-ST elevation myocardial infarction following paclitaxel administration for ovarian carcinoma: A case report and review of literatureJ Cancer Res Ther 2012 8(3):442-44. [Google Scholar]
[4]. Londhey VA, Parikh FS, Paclitaxel-induced myocardial infarction in a case of carcinoma ovaryJ Assoc Physicians India 2009 57:342-43. [Google Scholar]
[5]. Esber C, Breathett K, Sachak T, Moore S, Lilly SM, Acute myocardial infarction in patient with triple negative breast cancer after paclitaxel infusion: A Case ReportCardiol Res 2014 5:3-4.:108-11. [Google Scholar]
[6]. Schrader C, Keussen C, Bewig B, von Freier A, Lins M, Symptoms and signs of an acute myocardial ischemia caused by chemotherapy with paclitaxel (taxol) in a patient with metastatic ovarian carcinomaEur J Med Res 2005 10(11):498-501. [Google Scholar]
[7]. Oneglia C, Kounis NG, Beretta G, Ghizzoni G, Gualeni A, Berti M, Kounis syndrome in a patient with ovarian cancer and allergy to iodinated contrast media: Report of a case of vasospastic angina induced by chemotherapyInt J Cardiol 2011 149(2):e62-65. [Google Scholar]
[8]. Park SH, Byon JS, Lee SW, Lee SJ, Jin DK, Shin WY, Coronary artery thrombosis associated with paclitaxel in advanced ovarian cancerKorean Circ J 2009 39:124-27. [Google Scholar]
[9]. Pai VB, Nahata MC, Cardiotoxicity of chemotherapeutic agents: Incidence, treatment and preventionDrug Saf 2000 22:263-302. [Google Scholar]