Immune Thrombocytopenia as a Presenting Manifestation of Tuberculosis- Challenge in Resource Constraint Settings
Deba Prasad Dhibar1, Kamal Kant Sahu2, Varun Dhir3, Surjit Singh4
1 Senior Resident, Department of Internal Medicine, PGIMER, Chandigarh, India.
2 Senior Resident, Department of Haematology, PGIMER, Chandigarh, India.
3 Assistant Professor, Department of Internal Medicine, PGIMER, Chandigarh, India.
4 Professor, Department of Internal Medicine, PGIMER, Chandigarh, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Deba Prasad Dhibar, Senior Resident, Department of Internal Medicine, PGIMER, Chandigarh-160012, India.
E-mail: drdeba_prasad@yahoo.co.in
Tuberculosis can infect almost any organ of our body leading to various presentations and its complication. Various haematological manifestations of tuberculosis are well known. But isolated thrombocytopenia and Immune Thrombocytopenia (ITP) in patients with tuberculosis is very rare. Here we report a case of young man who presented with acute onset of bleeding manifestations in the form of epistaxis and macroscopic haematuria with platelets count of 5×109/L. The patient was diagnosed to have ITP along with clinical and radiological evidence of active tuberculosis. The patient was treated with Anti Tubercular Therapy (ATT) along with Intravenous (IV) pulse of methyl prednisolone followed by tapering dose of oral prednisolone.
Anti tubercular therapy, Bleeding manifestations, Prednisolone
Case Report
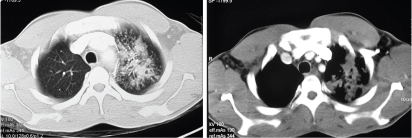
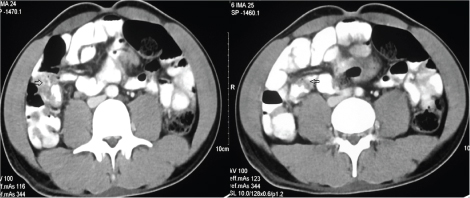
A 20-year-old man with no previous co-morbidities presented with three days history of haemorrhagic manifestations in the form of epistaxis, subconjuntival haemorrhage and haematuria. On evaluation, he was haemodynamically stable, conscious and oriented. Further enquiry revealed that he had low grade fever with dry cough associated with loss of appetite and loss of weight for last 3 months. His complete blood count suggested thrombocytopenia with platelets count of 5×109/L. Chest X-ray showed opacity at the left upper lobe suggestive of consolidation. Contrast-Enhanced Computed Tomography (CECT) chest showed consolidation and centrilobular nodule with tree in bud appearance in left upper lobe of the lung suggestive of possible active tuberculosis [Table/Fig-1]. Hypertonic saline induced sputum examination was negative for acid fast bacilli thrice. Subsequently, CECT abdomen [Table/Fig-2] showed circumferential mural thickening of the terminal ileum, suggestive of possible ileal tuberculosis. Bone marrow examination showed normocellular marrow spaces and increased megakaryocytes with no evidence of tubercular infiltration or granuloma formation, suggestive of peripheral destruction of platelets due to immune thrombocytopenia. Possibility of Immune Thrombocytopenic Purpura (ITP) along with clinico-radiological disseminated tuberculosis was kept. Aetiologic work up for thrombocytopenia was done. There was no evidence of Disseminated Intravascular Coagulation (DIC), coagulation parameter was within normal limit, blood culture and bone marrow aspirate culture were sterile and the patient was negative for Human Immunodeficiency Virus (HIV), Hepatitis C Virus (HCV), and HBV serology. There was no evidence of tubercular marrow infiltration, no evidence of Systemic Lupus Erythematosus (SLE); Antinuclear Antibody (ANA) was negative, there was no evidence of Haemophagocytic Lymphohistiocytosis (HLH) or lymphoreticular malignancy and no history of prior drug intake. As patient could not arrange for best supportive care (single donor apheresis platelets), endoscopic and bronchoscopic intervention for tissue diagnosis of tuberculosis could not be done because of severe thrombocytopenia with active bleeding manifestation.
CECT chest showing left upper lobe consolidation with breakdown.
CECT abdomen showing circumferential mural thickening of the terminal ileum.
The patient was managed conservatively with transfusion of Random Donor Platelets (RDPS) and bilateral nasal packing was done for epistaxis. Antitubercular Therapy (ATT) was started empirically with isoniazid, rifampicin, pyrazinamide and ethambutol. For definitive therapy of ITP in the presence of co-existent active tuberculosis, he was planned to give IV injection of human immunoglobulin (IV Ig) but could not be given due to lack of finance. While ATT was continued, he was given IV pulse of methyl prednisolone of 1 g/day for three days after explaining relatives of patient that there may be chance of flair up of the tuberculosis. Patient was continued on oral prednisolone 1mg/kg body weight for 3 weeks along with ATT. After five days of steroid therapy, platelet count showed rising trend of 50×109/L, which increased further to 70×109/L on 10th day of steroid therapy. With recovery of platelet counts, diagnostic bronchoscopy was planned but as the bleeding manifestations was resolving, patient and his relatives did not give consent. Hence, he was discharged on ATT and oral steroids. Two weeks later, on outdoor visit, his platelet count rose to 234×109/L. His serial chest x-rays showed gradual resolution of the size of consolidation [Table/Fig-3]. There was no recurrence of thrombocytopenia and bleeding manifestations. Presently ATT is being continued while steroids have been tapered off gradually.
Serial chest X-rays showing gradual resolution of the left upper lobe consolidation.

Discussion
The haematological manifestations of tuberculosis include anaemia, leucocytosis, leukemoid reaction, leucopenia, lymphopenia, pancytopenia and thrombocytopenia [1–3]. Thrombocytopenia usually appears along with pancytopenia due to non-immunologic phenomenon because to tubercular marrow infiltration in the disseminated form of tuberculosis [3]. Isolated thrombocytopenia or ITP in patients with tuberculosis is very rare. There are only few cases, reported ITP as a presenting manifestation of tuberculosis [4–8].
Diagnosis of tuberculosis in our case was based on clinical and radiological evidence. Therapeutic response in the form of increased platelet count with steroid and radiologic evidence of resolution of lung shadows with ATT consolidated our presumed diagnosis of ITP and pulmonary tuberculosis. Whether it was a rare presentation of pulmonary tuberculosis in the form of ITP or it was a mere coincidence is debatable. Like our case, many authors have reported therapeutic response to ATT along with steroids, so it is more likely to be an unusual presentation of TB in the form of ITP [4–8]. The exact pathophysiology for thrombocytopenia in tuberculosis is not well known. Some authors hypothesised that, there is immune mediated destruction of platelets by circulating anti-platelets antibody, which is likely to be produced by abnormal stimulation of B lymphocytes by Mycobacterium tuberculosis [3,6–8]. Our case was given intravenous methyl prednisolone pulse to prevent further catastrophic complication like intracranial bleeding, haemoptysis to which he responded. In the presence of active tuberculosis, IV-Ig is considered as the first choice [9,10]. But due to financial constraints, we could not give IV-Ig to our patient.
The purpose of reporting this case is to stress upon the challenges which is faced by physicians while managing co-existent TB and ITP. We still recommend use of IV-Ig as a frontline agent of choice in such cases [9,10]. But in resource limited countries like India where TB is prevalent, many a times courageous decision of treating with steroids may be rewarding and lifesaving.
Conclusion
In the developing nation like India, where prevalence of tuberculosis is very high, tuberculosis should be ruled out in patients presenting with ITP like picture. Though IV Ig should be the first choice of drug for ITP in the presence of active TB or other infections, IV pulse of methyl prednisolone may be given after judging the risk and benefit ratio, along with ATT or antimicrobials.
[1]. Pal S, Biswas NM, Dutta S, Brahmachari R, Immune thrombocytopenic purpura in a case of tubercular pleural effusion: A rare presentationLung India 2016 33(1):105-08. [Google Scholar]
[2]. Wessels G, Schaaf HS, Beyers N, Gie RP, Nel E, Donald PR, Haematological abnormalities in children with tuberculosisJ Trop Pediatr 1999 45(5):307-10. [Google Scholar]
[3]. Mert A, Bilir M, Tabak F, Ozaras R, Ozturk R, Senturk H, Miliary tuberculosis: clinical manifestation, diagnosis and outcome in 38 adultsRespirology 2001 6:217-24. [Google Scholar]
[4]. Ghobrial MW, Albornoz MA, Immune thrombocytopenia: a rare presenting manifestation of tuberculosisAm J Haematol 2001 67(2):139-43. [Google Scholar]
[5]. Al-Majed SA, Al-Momen AK, Al-Kassimi FA, Al-Zeer A, Kambal AM, Baaqil H, Tuberculosis presenting as immune thrombocytopenic purpuraActa Haematol 1995 94(3):135-38. [Google Scholar]
[6]. Ozkalemkas F, Ali R, Ozkan A, Ozcelik T, Ozkocaman V, Kunt-Uzaslan E, Tuberculosis presenting as immune thrombocytopenic purpuraAnn Clin Microbiol Antimicrob 2004 3:16 [Google Scholar]
[7]. Tabarsi P, Merza MA, Marjani M, Active pulmonary tuberculosis manifesting with idiopathic thrombocytopenic purpura: a rare presentationBraz J Infect Dis 2010 14(6):639-40. [Google Scholar]
[8]. Srividya G, Nikhila GS, Kaushik AV, Jayachandran K, Immune thrombocytopenia in tuberculosis: causal or coincidental?J Global Infect Dis 2014 6(13):128-31. [Google Scholar]
[9]. The American Society of Haematology ITP Practice Guideline PanelDiagnosis and treatment of idiopathic thrombocytopenic purpura: recommendations of the American Society of HaematologyAnn Intern Med 1997 126:319-26. [Google Scholar]
[10]. Neunert C, Lim W, Crowther M, Cohen A, Solberg L Jr, Crowther MA, American Society of Haematology. The American Society of Haematology 2011 evidence-based practice guideline for immune thrombocytopeniaBlood 2011 117(16):4190-207. [Google Scholar]