Palatonasal Fistula Repair – A Case of Unanticipated Difficult Intubation
Hemraj Tungaria1, Lalit K. Raiger2, Rajkumar Paliwal3, Shekhar Suman Saxena4, Bishan Kumar Bairwa5
1 Assistant Professor, Department of Anaesthesia, Rabindranath Tagore Medical College, Udaipur, Rajasthan, India.
2 Senior Professor, Department of Anaesthesia, Rabindranath Tagore Medical College, Udaipur, Rajasthan, India.
3 Professor, Department of Plastic Surgery, Rabindranath Tagore Medical College, Udaipur, Rajasthan, India.
4 Junior Registrar, Department of Anaesthesia, Rabindranath Tagore Medical College, Udaipur, Rajasthan, India.
5 Assistant Professor, Department of Anaesthesia, Rabindranath Tagore Medical College, Udaipur, Rajasthan, India.
NAME, ADDRESS, E-MAIL ID OF THE CORRESPONDING AUTHOR: Dr. Hemraj Tungaria, 201, The Vintage Delight, Madhav Nagar, Shobhagpura, Udaipur-313011, Rajasthan, India.
E-mail: htungaria@gmail.com
Patients with present or previous history of facio-maxillary trauma will mostly be associated with a difficult airway. Surgical correction of these injuries might not always correct the altered airway. We report a case of palatonasal fistula following an old facio-maxillary fracture, which has led to interpretation of a difficult airway into a normal one. The patient was found to be having difficult airway during direct laryngoscopy which caused failure to intubate initially. Though, the patient was successfully intubated in the third attempt by senior anaesthesiologist making use of manoeuvres and equipment available, it made an impact for us to do a proper pre-op evaluation of patients with history of surgical correction of facial injuries and also for being prepared for can’t ventilate and can’t intubate situation in such type of cases. Through, this case report we stress the importance of airway anatomical alterations following facio-maxillary trauma and their corresponding management.
Difficult airway, Facio-maxillary trauma, Mallampati scoring
Case Report
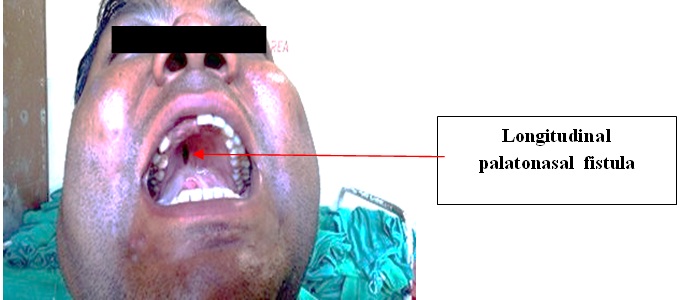
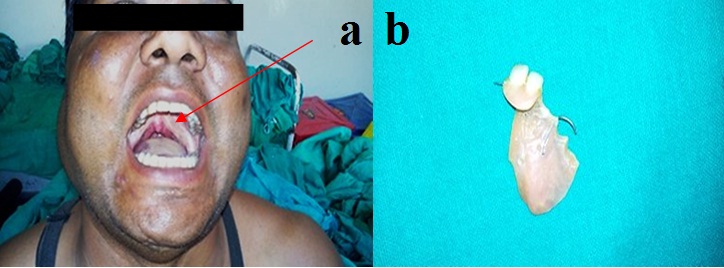
A 34-year-old male patient with old repaired facio-maxillary injury following road traffic accident, presented with vertical slit like opening in posterior hard palate on right side [Table/Fig-1]. He had complaints of regurgitation of food material from nose while eating and nasal twang while speaking. He used palatal obturator with dental retainers [Table/Fig-2a,b] to prevent regurgitation and hyper nasality but some symptoms still persisted. He needed surgical correction as the obturator couldn’t seal the fistula properly. Hence, he was planned for flap closure of the fistula by the plastic surgeon.
Patient without palatal obturator.
(a) Patient wearing palatal obturator. (b) Palatal obturator with dental retainer worn by the patient.
His pre anaesthetic evaluation revealed that he was chronic alcoholic, smoker, tobacco and betel nut chewer with no associated medical illness. He was morbidly obese with airway examination assessment showing Mallampati score 1, mouth opening 2½ fingers (approx.), heavy jaw, submucous fibrosis of gingival mucosa, increased trans mandibular width (post injury as per history reported by patient) [Table/Fig-1,2a]. Documentation of previous injury and surgical repair was not available.
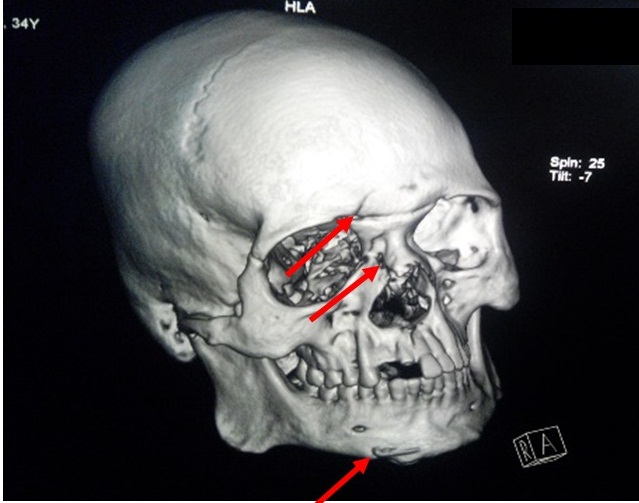
On investigation complete blood count, liver function, renal function, coagulation profiles were in normal range. A 3D-CT of face showed multiple healed facial bone fractures (e.g., root of nose, right mandibular condyle) also seen intra-osseous wiring along right parasymphyseal region of mandible [Table/Fig-3].
CT showing multiple fractures of facial bones fixed with wire.
Patient was posted for elective surgery. Standard monitoring started and patient was premedicated with Inj. Midazolam 1mg, Inj. Glycopyrrolate 0.2mg, Inj. Ondansetron 4mg, Inj. Fentanyl 100μg along with Inj. Lignocaine (IV) 60mg to attenuate laryngoscopic sympathetic response followed by preoxygenation with 100% O2. Induction done with Inj. Thiopentone 300mg along with sevoflurane inhalation. Once loss of reflexes and apnoea achieved, bag and mask ventilation tried but difficulty occurred for single person to ventilate. Hence, facemask was held by both hands of one anaesthesiologist and another anaesthesiologist made bag ventilation. Once bag and mask ventilation was achieved satisfactorily Inj. Succinylcholine 100mg was given. After disappearance of fasciculation, direct laryngoscopy was done for endotracheal intubation. On laryngoscopy with no.4 Macintosh blade only the tip of epiglottis was visible (Comark and Lehane grade 3). There was no space between epiglottis and tongue for upward lifting of the larynx and there was little room for manipulating laryngoscopic blade in the oral cavity which made intubation difficult further. Patient was not able to be intubated in the first 2 attempts by the resident anaesthesiologist and junior consultant and hence bag mask ventilation continued to maintain saturation. Successful intubation achieved only in third attempt by senior anaesthesiologist with Portex ET Tube No 8 with the help of stylet after moulding it to hockey stick shape along with BURP (Backward upward, rightward pressure) manoeuvre and sliding the tube along the epiglottis blindly.
After confirming bilateral air entry tube was fixed. Patient was maintained on O2, N2O, sevoflurane and Inj. Atracurium. Surgeon made oropharyngeal packing himself. Surgeon also faced difficulty in reaching the surgical site to repair even after application of mouth retractor. Rest of the intraoperative period was uneventful and surgery accomplished with closing fistula by suturing on nasal side and with flap closure on oral side.
Patient was extubated after gaining all reflexes, alertness and following verbal command. Post extubation, patient was oxygenated for 10 min and observed for another 30 min in recovery room. Patient was shifted to postoperative ward and discharged after 48 hours without any complications.
Discussion
Palatonasal fistula can occur following faciomaxillary injuries [1] or following unsuccessful [2] surgery involving the oral cavity tumour, cleft palate and fixation of faciomaxillary fractures [3] and also due to consumption of tobacco product. In palato-nasal fistula there is persistent passage between oral and nasal cavity. There is problem of regurgitation of solid food particles and liquids in the nostrils along with speech problems. They are result of inadequate dissection of flap, closure under tension, postoperative bleeding, haematoma formation between the oral and nasal layers and infection. Palatal fistulae represent failure of surgical technique [4]. Treatment for these fistulae involves wearing a fistula obturator or permanent surgical repair involving flap closure [5]. Securing the airway in such patients, during elective surgeries involving general anaesthesia with endotracheal intubation, can be challenging due to restricted mouth opening and or due to dental malocclusion, even Mallampati may be score I. Hence, difficult ventilation and difficult intubation cart has to be kept ready [6].
Palatal fistula may present on hard palate, soft palate or on uvula and are classified as longitudinal or transverse. Palatal fistula in our case was as a result of trauma involving multiple fractures of facial bones fixed with wire [Table/Fig-3].
Fistula was vertical on right side of hard palate approx. 1cm in size [Table/Fig-1,2a]. After previous surgery patient had history of increase trans mandibular width which may be due to increase soft tissue or fat deposition during healing process. Along with these he had heavy jaw, large tongue, obesity which made mask ventilation difficult. All these factors created non-visualization of glottic opening.
Multiple fractures of facial bones and their surgical repair may lead to disturbed anatomy of facial structures which might be due to malocclusion, non-union osteomyelitis, oronasal fistula, increase transverse diameter of facial planes and cranio-facial dysjunction. (Le Fort 3rd) [6].
In our patient there is upward pulling of uvula, mightbe due to previous surgery/repair which was interpreted as mallampati grading 1 and normal mouth opening. We have to be more cautious in these types of patients during preanaesthetic evaluation to examine facial anatomy and intraoral examination carefully. These patients may pose difficulty in mask ventilation, direct laryngoscopy and intubation even though graded normally.
So we have to be prepared with difficult intubation cart with different size mask, endotracheal tubes, blades (McIntosh, Miller’s and McCoy), LMA, combitube, LTS, bougie, stylet, fiberoptic laryngoscope, needle Cricothyroidotomy kit, retrograde intubation kit and a skilled anaesthesiologist and tuned assistant.
Conclusion
Postsurgical repair cases especially of maxillofacial injury should be kept in difficult intubation category even though they are graded normally with mallampati airway assessment. Numerous techniques and devices are in current use, such as the Bullard laryngoscope, malleable stylet, light wand, blind nasal intubation, flexible fiberoptic bronchoscope, intubation through Laryngeal Mask (LMA) and retrograde intubation using guidewire/ cathetersWhenever anticipate, the best available resources should be make available and must plan according to difficult airway algorithm. Basic rules of anaesthesia should always be kept in mind in each and every case.
[1]. Moghe S, Gupta MK, Pillai A, Repair of oronasal fistula with split-thickness palatal graftIOSR Journal of Dental and Medical Sciences 2014 (13):89-92. [Google Scholar]
[2]. Chowdhury S, Gokkulakrishnan S, Prasanna D, Dhaka G, Kumari N, Management of post traumatic residual deformity: a case report and literature reviewJournal of Dental Sciences and Oral Rehabilitation 2012 :37-40. [Google Scholar]
[3]. Masjid Omer W, Persistent oronasal fistula after primary management of facial gunshot injuriesBr J Oral Maxillofac Surg 2008 46(1):50-52. [Google Scholar]
[4]. Richardson S, Agni NA, Palatal Fistulae: A comprehensive classification and difficulty indexJ Maxillofac Oral Surg 2014 13(3):305-09. [Google Scholar]
[5]. Garner Justin M, Wein Richard O, Use of the palatal flap for closure of an oronasal fistulaAm J Otolaryngol 2006 27(4):268-70. [Google Scholar]
[6]. Sood J, Maxillofacial and upper airway injuries anaesthetic impactIndian Journal of Anaesthesia 2008 52(5):688-98. [Google Scholar]