The continuous goal of minimal access cholecystectomy is to reduce the number and size of the ports. The outcomes in minimal access surgeries are not only judged by patients’ safety but also by a better quality of care in terms of pain and cosmesis. Minimal or scar-less surgery is the ultimate demand by the patients and also strived by the surgeons [8].
Pelosi et al., made the beginning of SILS by performing the first single incision appendicectomy in the year 1992 on a child [9]. Navarra et al., in the year 1997 subsequently performed the first SILS via two trans-umbilical trocars and three trans-abdominal gall bladder stay sutures [10]. We sought to investigate the technical feasibility, safety and benefit of SILC versus C4PLC in our set-up.
Materials and Methods
This prospective randomized comparative study was aimed to compare the following parameters in SILC and C4PLC:
Operative Time (in minutes).
Surgical related morbidity.
Mortality.
Procedure related: CBD injury, GB wall perforation, Bleeding from the liver bed, Bile leak, Iatrogenic liver injury.
Port site haematoma/seroma/infection.
Port site hernia.
Conversion to multi-incision/ multiport lap chole or open cholecystectomy.
Post-operative Pain.
Pain score (using VAS).
Analgesic Requirement (injectable and tablet).
Hospital Stay (number of days).
Return to normal activity.
Cosmetic satisfaction.
A total of 64 patients were enrolled for the study from June 2014 to June 2015 and divided equally into two groups: Group A: Single Incision Laparoscopic Cholecystectomy (SILC) Group B: Conventional Four-Port Laparoscopic Cholecystectomy (C4PLC).
Sampling Technique
Randomization was done by computer generated numbers.
Statistical Analysis
Statistical analysis was done by SPSS version 22.0. Simple comparative statistical analyses were carried out. Results on continuous measurements are presented as Mean ± SD (Min-Max) and results on categorical measurements are presented in Number (%). Significance is assessed at 5% level of significance.
Fisher-exact test has been used to find the significance of the study parameters on continuous scale between two groups (Inter group analysis) on metric parameters.
Sample Selection
Inclusion Criteria
Patients between 18 to 70years of age of either sex attending the hospital for laparoscopic cholecystectomy were randomly assigned to either group after taking signed informed consent.
Preoperative work up included a complete history and physical examination, standard laboratory tests including abdominal ultrasound. Ultrasonography confirmed the presence of gallbladder stones in all patients.
Exclusion Criteria
Patients who did not want to undergo laparoscopic cholecystectomy.
Suspected presence of common bile duct stones.
History of jaundice.
History of gallstone pancreatitis.
Patients with chronic cholecystitis who showed GB wall thickening in the ultrasound scan, pericholecystic collection, adhesion etc.
Patients with psychiatric disorders.
Patients with severe co-morbid conditions like heart diseases, stroke and vascular diseases.
Surgical Procedure
Surgeries were performed by a single surgeon under general anaesthesia in supine position. Pneumoperitoneum was preset at 12-14mmHg. The conventional four port technique involved inserting a 10mm trocar through the umbilical incision through or just above the umbilicus, second 10mm port was inserted in the epigastrium in the midline about 2cm below the xiphoid process, one 5mm trocar was inserted in the right hypochondrium in the anterior axillary line 3cm below the costal margin and another 5mm trocar was inserted in the right mid clavicular line around 2cm from the costal margin. The patient was then placed in reverse Trendelenburg position with a left down tilt.
For the SILC procedure one 1.5-2cm transumbilical incision was made in a horizontal fashion without extension of the incision beyond outer limit of the umbilical folds. Blunt dissection was used to expose the base of the umbilicus. A fascial incision tailored to the access port was made with a scalpel while lifting the umbilicus. A haemostat or finger was gently advanced through the fascial incision to ensure that there are no attachments or adhesions. The commercial port was then inserted into the body cavity. Pneumoperitoneum was created by joining the CO2 input tube to the inlet in the port and the pressure was set up to 14mmHg. The patient was then placed in reverse Trendelenburg position with a slight left lateral decubitus in order to expose the surgical field. A 10mm camera port was used and the routinely available 10mm rigid 30 degree endoscope introduced to visualize the operative field. We used two 5 mm ports for the hand instrument and the harmonic ace scalpel or the hook cautery was used during the procedure. The special roticulating graspers and endoscissors and 5mm clip applicator were utilized during the procedures.
Results
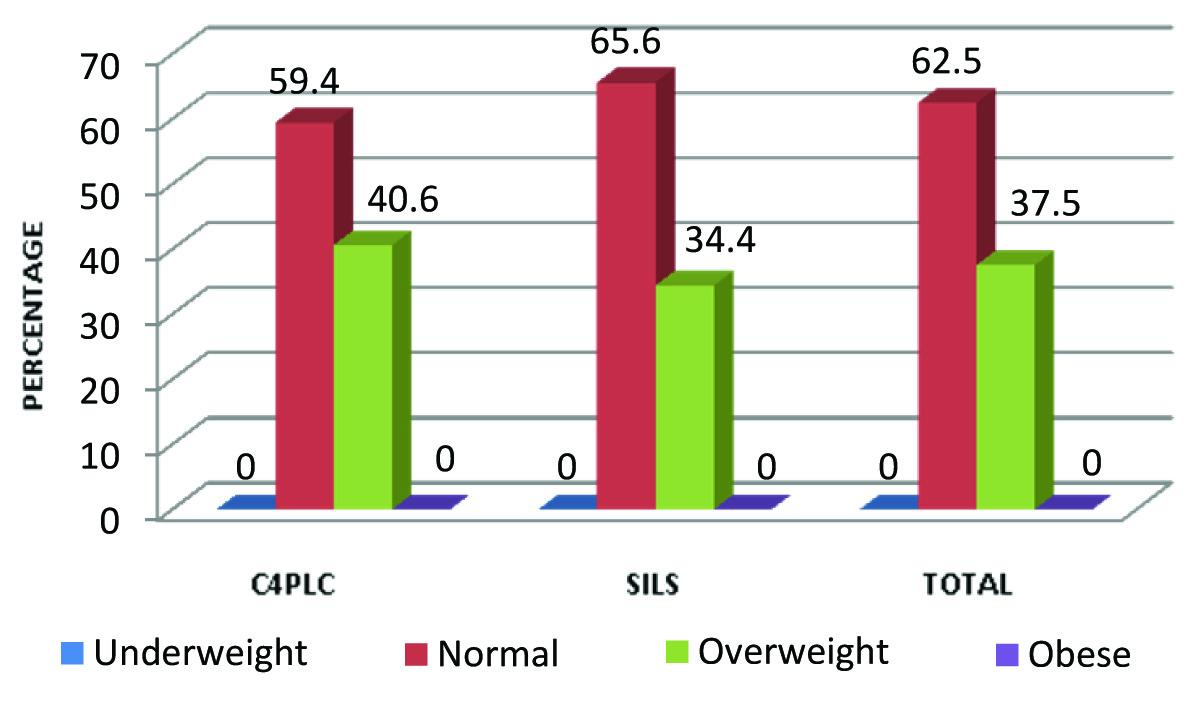
There was female predominance in the study (87.5% versus 12.5%). The age and BMI wise distribution of the participants are depicted in [Table/Fig-1,2].
Age distribution of the patients in percentage.
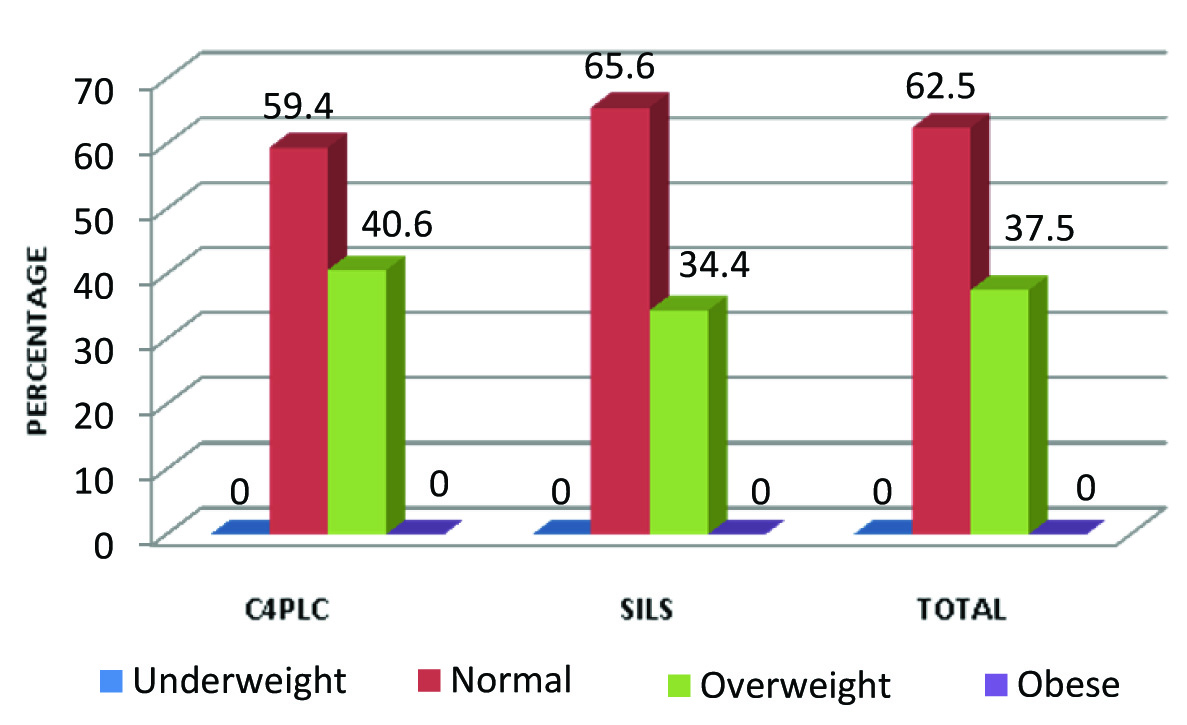
Distribution of the patients by BMI.
The duration of hospital stay, cosmetic outcome are shown in [Table/Fig-3,4]. All patients returned to normal activity within four days in SILC [Table/Fig-5]. Patients who had C4PLC had high pain score (>2.5) than those who had SILC and this finding was found to be significant (p<0.05) [Table/Fig-6].
Average operating timing (OT) and hospital stay.
| Parameter | C4PLCMean ± SD | SILCMean ± SD | Total |
|---|
| OT time(in minutes) | 38.53 ± 4.00 | 69 ± 4.00 | t= -30.561 (p-0.001) |
| Hospital stay(in days) | 2.468 ± 0.59 | 1.72 ± 0.40 | t= 5.917 (p-0.001) |
| Cosmetic satisfaction | C4PLC | SILC | Total | Fisher-exact test |
|---|
| Not satisfied | 4 (12.5) | 0 (0.0) | 4 (6.2) | 4.27 (p-0.11) |
| Satisfied* | 28 (87.5) | 8 (25.0) | 36 (56.2) |
| Very satisfied* | 0 (0.0) | 24 (75.0) | 24 (37.6) |
| Total | 32 (100.0) | 32 (100.0) | 64 (100.0) |
*cells were clubbed together for analysis.
Return to normal activity.
| Return to normal activity in days | C4PLC | SILC | Total | Fisher-exact test |
|---|
| Three* | 0 (0.0) | 26 (81.2) | 26 (40.6) | 49.78 (p-0.001) |
| Four* | 4 (12.5) | 6 (18.8) | 10 (15.6) |
| Five# | 22 (68.8) | 0 (0.0) | 22 (34.4) |
| Six# | 6 (18.8) | 0 (0.0) | 6 (9.4) |
| Total | 32 (100.0) | 32 (100.0) | 64 (100.0) |
*cells and #cells were clubbed for analysis.
| Score | C4PLC | SILC | Total | Fisher-exact test |
|---|
| 1* | 0 (0.0) | 1 (3.1) | 1 (1.6) | 60.12 (p-0.001) |
| 1.5* | 0 (0.0) | 9 (28.1) | 9 (14.1) |
| 2* | 0 (0.0) | 20 (62.5) | 20 (31.2) |
| 2.5* | 0 (0.0) | 1 (3.1) | 1 (1.6) |
| 3# | 13 (40.6) | 1 (3.1) | 14 (21.9) |
| 3.5# | 8 (25.0) | 0 (0.0) | 8 (12.5) |
| 4# | 10 (31.2) | 0 (0.0) | 10 (15.6) |
| 5# | 1 (3.1) | 0 (0.0) | 1 (1.6) |
| Total | 32 (100.0) | 32 (100.0) | 64 (100.0) |
*cells and #cells were clubbed together for analysis.
As shown in [Table/Fig-7], in C4PLC group, the mean dose of analgesic injection was 2.78±0.75 (208.5mg) and in SILS group was 1.84±0.57 (138mg). Each dose consists of 75mg of diclofenac sodium. This suggests that there was significant difference in analgesic injection in these two groups (p<0.05).
Injectable analgesic requirement.
| Number of injection | C4PLC | SILC | Fisher-exact test |
|---|
| 1* | 0 (0.0) | 8 (25.0) | 26.35 (p-0.001) |
| 2* | 13 (40.6) | 21 (65.6) |
| 3# | 13 (40.6) | 3 (9.4) |
| 4# | 6 (18.8) | 0 (0.0) |
| Total | 32 (100.0) | 32 (100.0) |
| Mean ± SD | 2.78 ± 0.75 | 1.84 ± 0.57 |
*cells and #cells were clubbed for analysis.
As shown in [Table/Fig-8], the mean dose of oral analgesic taken by C4PLC group was 3.75±0.67 (375mg), while in SILC group was 2.40±0.55 (240mg). Each dose consisted of 100mg of aceclofenac tablet. This suggests that there is statistical difference in two groups with regard to analgesic tablets taken (p<0.05).
Oral analgesic requirement.
| Number of tablets | C4PLC | SILC | Fisher-exact test |
|---|
| 1* | 0 (0.0) | 0 (0.0) | 25.59(p-0.001) |
| 2* | 0 (0.0) | 20 (62.5) |
| 3* | 12 (37.5) | 11 (34.4) |
| 4 # | 16 (50.0) | 1 (3.1) |
| 5# | 4 (12.5) | 0 (0.0) |
| Total | 32 (100.0) | 32 (100.0) |
| Mean ± SD | 3.75 ± 0.67 | 2.40 ± 0.55 |
*cells and #cells were clubbed together for analysis.
Discussion
Lesser post-operative pain and early return to normal activities are the major goals in minimal access surgery. As minimally invasive surgeries continue to evolve, so does the quest to reduce the surgical footprint based on several potential benefits of reduced post-operative pain, hospital stay, cosmesis and overall surgical expenditure. The results show that SILC yields almost the same success rate as the conventional procedure. Furthermore, the results of the single port technique were more favorable in that it reduces pain, so that fewer analgesic injections were needed for pain control post-operatively. The single incision group also took fewer analgesic tablets as compared to the conventional four port group, which was statistically significant (p=0.001). Similar results were shown by many authors [10,11].
The cosmesis achieved with the SILC technique is one of the most satisfactory points to score over the conventional four port technique. The result in our study showed most patient being satisfied with their post-operative scar even though the result was statistically in significant (p=>0.05).
Patients in the SILC group had a shorter hospital stay (1.72 ± 0.40 days vs. 2.468 ± 0.59 days) may be owing to significantly less post-operative pain and returned to normal activity earlier than the C4PLC group. Both the values were found to be statistically significant (p=<0.05) as in other studies [12–14].
There was no significant difference in terms of procedure related complications like gall bladder wall perforation, bile leak, and liver bed bleeding or iatrogenic liver injury, and port site hematoma formation. No mortality was reported in our series. In two cases, an extra port was required for better dissection of the Calot’s triangle as there was moderate adhesion with mildly fibrosed gall bladder wall. In another case, a conversion to conventional four port procedure was done because of gross fibrosis and thickening of the gallbladder and Calot’s triangle area with moderate adhesion of the intestine. None of the procedure needed a conversion to an open procedure. No increased incidence of bile duct injury occurred in either group similar to the study of Allemann P et al., [15].
The mean operative time was higher in the SILC group (69 ± 4.00 mins vs. 38.53 ± 4.00 min), which was statistically significant (p<0.05) and correlates well with the previous studies [16–18]. The reason behind the longer operative time being the use of limited instruments and difficult ergonomics associated with the single port technique. SILC also has a higher procedure failure rate and associated with more blood loss and takes longer than Conventional Laparoscopic Cholecystectomy (CLC) [19].
Marks JM et al., reported an increased incidence in port site herniation in patients undergoing SILC when compared with patients undergoing the conventional 4 ports technique (8.4% versus 1.2%) [20]. No port site herniation was reported in our patients.
The average operative cost was significantly higher in the SILC group due to the use of commercially available access ports. Similar result was found by Matyia M et al., [21].
A limitation of the SILS procedure is in very obese patients and in patients who had undergone multiple previous abdominal operations as shown by Jacob DA et al., [22].
For patients with a higher body mass index or acute cholecystitis, it may be better to consider performing conventional laparoscopic cholecystectomy or to use additional retraction devices [23], but SILC has been done safely for the treatment of acute cholecystitis and acute gallstone cholangitis in some series [24,25].
SILC is a safe and feasible procedure that is comparable to Multi-Incision Laparoscopic Cholecystectomy (MILC), but requires a step-by-step training program [12]. SILC provides surgeons with an alternative minimally invasive surgical option and to hide the surgical scar within the umbilicus [26].
Limitation
More number of cases could have been better in validating the safety profile and feasibility of SILC over the conventional four ports technique.
Conclusion
SILC is safe and has almost similar clinical outcomes to those of C4PLC, with no obvious increase in bile duct injuries, a reduced need for analgesics, less days of hospital stay, with better cosmetic result in lieu of a little more extra operative time. It can be safely offered to patients requiring laparoscopic cholecystectomy.
*cells were clubbed together for analysis.
*cells and #cells were clubbed for analysis.
*cells and #cells were clubbed together for analysis.
*cells and #cells were clubbed for analysis.
*cells and #cells were clubbed together for analysis.